CANVAS Trial)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2008/0317805 A1 Mckay Et Al
US 20080317805A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2008/0317805 A1 McKay et al. (43) Pub. Date: Dec. 25, 2008 (54) LOCALLY ADMINISTRATED LOW DOSES Publication Classification OF CORTICOSTEROIDS (51) Int. Cl. A6II 3/566 (2006.01) (76) Inventors: William F. McKay, Memphis, TN A6II 3/56 (2006.01) (US); John Myers Zanella, A6IR 9/00 (2006.01) Cordova, TN (US); Christopher M. A6IP 25/04 (2006.01) Hobot, Tonka Bay, MN (US) (52) U.S. Cl. .......... 424/422:514/169; 514/179; 514/180 (57) ABSTRACT Correspondence Address: This invention provides for using a locally delivered low dose Medtronic Spinal and Biologics of a corticosteroid to treat pain caused by any inflammatory Attn: Noreen Johnson - IP Legal Department disease including sciatica, herniated disc, Stenosis, mylopa 2600 Sofamor Danek Drive thy, low back pain, facet pain, osteoarthritis, rheumatoid Memphis, TN38132 (US) arthritis, osteolysis, tendonitis, carpal tunnel syndrome, or tarsal tunnel syndrome. More specifically, a locally delivered low dose of a corticosteroid can be released into the epidural (21) Appl. No.: 11/765,040 space, perineural space, or the foramenal space at or near the site of a patient's pain by a drug pump or a biodegradable drug (22) Filed: Jun. 19, 2007 depot. E Day 7 8 Day 14 El Day 21 3OO 2OO OO OO Control Dexamethasone DexamethasOne Dexamethasone Fuocinolone Fluocinolone Fuocinolone 2.0 ng/hr 1Ong/hr 50 ng/hr 0.0032ng/hr 0.016 ng/hr 0.08 ng/hr Patent Application Publication Dec. 25, 2008 Sheet 1 of 2 US 2008/0317805 A1 900 ----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- 80.0 - 7OO – 6OO - 5OO - E Day 7 EDay 14 40.0 - : El Day 21 2OO - OO = OO – Dexamethasone Dexamethasone Dexamethasone Fuocinolone Fluocinolone Fuocinolone 2.0 ng/hr 1Ong/hr 50 ng/hr O.OO32ng/hr O.016 ng/hr 0.08 nghr Patent Application Publication Dec. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

Correlation Between Clinical Response to Hormone Therapy and Steroid Receptor Content in Prostatic Cancer1
[CANCER RESEARCH 38, 4345-4348, November 1978] 0008-5472/78/0038-0000$02.00 Correlation between Clinical Response to Hormone Therapy and Steroid Receptor Content in Prostatic Cancer1 Jan-Àke Gustafsson, Peter Ekman, Marek Snochowski, Anders Zetterberg, Ake Pousette, and Bertil Hogberg Department of Chemistry, Karolinska Institute [J.-A. G., M. S., A. P.], and Department of Urology [P. E.¡and Clinical Pathology Laboratory ¡A.2.], Karolinska Hospital, 104 01 Stockholm 60, Sweden, and Department of Pharmacology, Karolinska Institute and AB LEO Research Laboratories, Helsingborg, Sweden [B. H.] Abstract radical prostatectomy (3); in most other countries the figures are much lower. Hormonal therapy is the dominating form of treatment Thus, hormonal treatment (orchidectomy, estrogen or for prostatic carcinoma. The majority of cases (80%) are progestin administration) is the major tool to control the well controlled for varying times with this regimen. How growth of prostatic cancer. Estrogen therapy is the most ever, thus far there have been no adequate methods to common form of therapy in many countries. However, this predict in which cases hormonal therapy is of less benefit. treatment has many side effects, and the cardiovascular Measurement of cancer tissue content of intracellular complications have gained increasing attention. The mech hormone receptors constitutes progress toward a more anism behind the estrogen activity is still obscure; the individualized therapy in prostatic carcinoma. In this study secretion of luteinizing hormone from the pituitary is de biopsies from 16 cancer patients were taken before ther creased, and, consequently, androgen secretion from the apy was given, and the specimens were analyzed with testes is decreased. -

A Pharmaceutical Product for Hormone Replacement Therapy Comprising Tibolone Or a Derivative Thereof and Estradiol Or a Derivative Thereof
Europäisches Patentamt *EP001522306A1* (19) European Patent Office Office européen des brevets (11) EP 1 522 306 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.7: A61K 31/567, A61K 31/565, 13.04.2005 Bulletin 2005/15 A61P 15/12 (21) Application number: 03103726.0 (22) Date of filing: 08.10.2003 (84) Designated Contracting States: • Perez, Francisco AT BE BG CH CY CZ DE DK EE ES FI FR GB GR 08970 Sant Joan Despi (Barcelona) (ES) HU IE IT LI LU MC NL PT RO SE SI SK TR • Banado M., Carlos Designated Extension States: 28033 Madrid (ES) AL LT LV MK (74) Representative: Markvardsen, Peter et al (71) Applicant: Liconsa, Liberacion Controlada de Markvardsen Patents, Sustancias Activas, S.A. Patent Department, 08028 Barcelona (ES) P.O. Box 114, Favrholmvaenget 40 (72) Inventors: 3400 Hilleroed (DK) • Palacios, Santiago 28001 Madrid (ES) (54) A pharmaceutical product for hormone replacement therapy comprising tibolone or a derivative thereof and estradiol or a derivative thereof (57) A pharmaceutical product comprising an effec- arate or sequential use in a method for hormone re- tive amount of tibolone or derivative thereof, an effective placement therapy or prevention of hypoestrogenism amount of estradiol or derivative thereof and a pharma- associated clinical symptoms in a human person, in par- ceutically acceptable carrier, wherein the product is pro- ticular wherein the human is a postmenopausal woman. vided as a combined preparation for simultaneous, sep- EP 1 522 306 A1 Printed by Jouve, 75001 PARIS (FR) 1 EP 1 522 306 A1 2 Description [0008] The review article of Journal of Steroid Bio- chemistry and Molecular Biology (2001), 76(1-5), FIELD OF THE INVENTION: 231-238 provides a review of some of these compara- tive studies. -
Jan 19, 2009 Listing of Generic, Non
http://www.medword.com/uspa.html Jan 19, 2009 Listing of generic, non-prescription, prescription, and OTC (over-the-counter) p harmaceuticals A-200 Gel Concentrate A-200 Shampoo Concentrate A-25 A-Cillin A-Fil A-Hydrocort A-methaPred A-Phedrin A-Spas S/L A Plus A.C. & C. A.P.L. A.R.M. Allergy Relief A.R.M. Maximum Strength Caplets A/B Otic A/Fish Oil A/T/S abacavir abarelix-depot-F abarelix-depot-M Abbokinase Abbokinase Open-Cath Abelcet Abenol Abitrate Absorbine Athletes Foot Absorbine Jock Itch Absorbine Jr. Antifungal AC acarbose Accolate Accupep HPF Accupril Accuretic Accutane Accutane Roche acebutolol Acel-Imune Acellular DTP Aceon Acet-2 Acet-3 Acet Codeine 30 Acet Codeine 60 Aceta Aceta Elixir Aceta Tablets acetaminophen acetaminophen-butalbital acetaminophen-caffeine acetaminophen-chlorpheniramine acetaminophen-codeine acetaminophen-dextromethorphan acetaminophen-diphenhydramine acetaminophen-hydrocodone acetaminophen-oxycodone acetaminophen-phenyltoloxamine acetaminophen-propoxyphene acetaminophen-propoxyphene hydrochloride acetaminophen-propoxyphene napsylate acetaminophen-pseudoephedrine acetazolam acetazolamide Acetest acetic acid Acetocot acetohexamide acetophenazine Acetoxyl 10 Gel Acetoxyl 2.5 Gel Acetoxyl 20 Gel Acetoxyl 5 Gel acetylsalicylic acid Achromycin Achromycin V aciclovir Acid Control Acid Phos Fluor Rinse Acilac Aciphex acitretin Aclophen Aclovate Acne-10 Lotion Acne-5 Lotion Acne-Aid Aqua Gel Acne-Aid Gel Acne-Aid Vanishing Cream Acne Aid 10 Cream Acne Lotion 10 Acne Prone Skin Sunscreen Acne Wash Acno Acnomel -

Eligibility Regulations for Transgender Athletes
ELIGIBILITY REGULATIONS FOR TRANSGENDER ATHLETES In the case of confidential queries regarding cases affected by these Transgender Regulations, please contact: WT Medical Manager (email: [email protected]) Table of Contents 1. Introduction ....................................................................................................................... 1 2. Application ........................................................................................................................ 3 3. Eligibility Conditions For Transgender Athletes ................................................................... 5 3a. Eligibility conditions for Transgender male athletes .......................................................... 5 3b. Eligibility conditions for Transgender female athletes ....................................................... 5 3c. Provisions applicable to all Transgender athletes .............................................................. 5 4. Assessment by the Expert Panel ......................................................................................... 7 5. Monitoring/Investigating Compliance ................................................................................ 9 6. Disciplinary Proceedings .................................................................................................... 11 7. Dispute Resolution ............................................................................................................ 12 8. Confidentiality ................................................................................................................. -
Steroid Hormones Part Two
Steroid Hormones Part Two Medicinal Chemistry III / 4th stage/ 1st Semester Lecture 9 Dr.Narmin Hama Amin Androgens Endogenous Androgens Testosterone and its more potent reduction product 5α-DHT are produced in significantly greater amounts in males than in females, but females also produce low amounts of these “male” sex hormones. Endogenous compounds have two important activities: ➢ Androgenic activity (promoting male sex characteristics) ➢ Anabolic activity (muscle building). ➢ Biosynthesis Testosterone can be synthesized through pregnenolone, DHEA(dehydroepiandrosterone) , and androstenedione Metabolism of Androgens ▪ Testosterone is rapidly converted to 5α-DHT in many tissues by the action of 5α-reductase. Depending on the tissue, this is either to activate testosterone to the more potent androgen, DHT (e.g., in the prostate), or a step in the metabolic inactivation of this androgen. The primary route for metabolic inactivation of testosterone and DHT is oxidation to the 17-one. The 3-one group is also reduced to the 3α- (major) and 3α- ols (minor). ▪ Androsterone is the major urinary metabolite and was the first “androgenic” steroid isolated. These metabolites are excreted mainly as the corresponding glucuronides Metabolism of Androgens SARs Of Androgens Testosterone exerts its physiological activity after its conversion to Dihydrotestosterone. A steroidal skeleton is minimum structural requirement to have androgenic activity. 17β hydroxyl function to be essential for androgenic and anabolic activity. Reduction of the A ring e.g., DHT may increase potency. Introduction of 17α methyl group confers oral activity on testosterone. Testosterone not effective orally, because metabolic changes at 17-β oxygen, which is used to attach the receptor site. 17-α alkyl groups prevent these metabolic changes so that compounds are orally active. -

(12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 De Juan Et Al
US 20110159073A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 de Juan et al. (43) Pub. Date: Jun. 30, 2011 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA A6F 2/00 (2006.01) (US); Signe E. Varner, Los (52) U.S. Cl. ........................................................ 424/427 Angeles, CA (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Featured is a method for instilling one or more bioactive (21) Appl. No.: 12/981,038 agents into ocular tissue within an eye of a patient for the treatment of an ocular condition, the method comprising con (22) Filed: Dec. 29, 2010 currently using at least two of the following bioactive agent delivery methods (A)-(C): (A) implanting a Sustained release Related U.S. Application Data delivery device comprising one or more bioactive agents in a (63) Continuation of application No. 1 1/175,850, filed on posterior region of the eye so that it delivers the one or more Jul. 5, 2005, now abandoned. bioactive agents into the vitreous humor of the eye; (B) instill ing (e.g., injecting or implanting) one or more bioactive (60) Provisional application No. 60/585,236, filed on Jul. 2, agents Subretinally; and (C) instilling (e.g., injecting or deliv 2004, provisional application No. 60/669,701, filed on ering by ocular iontophoresis) one or more bioactive agents Apr. 8, 2005. into the vitreous humor of the eye. Patent Application Publication Jun. 30, 2011 Sheet 1 of 22 US 2011/O159073 A1 Patent Application Publication Jun. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -
Cumulative Cross Index to Iarc Monographs
PERSONAL HABITS AND INDOOR COMBUSTIONS volume 100 e A review of humAn cArcinogens This publication represents the views and expert opinions of an IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, which met in Lyon, 29 September-6 October 2009 LYON, FRANCE - 2012 iArc monogrAphs on the evAluAtion of cArcinogenic risks to humAns CUMULATIVE CROSS INDEX TO IARC MONOGRAPHS The volume, page and year of publication are given. References to corrigenda are given in parentheses. A A-α-C .............................................................40, 245 (1986); Suppl. 7, 56 (1987) Acenaphthene ........................................................................92, 35 (2010) Acepyrene ............................................................................92, 35 (2010) Acetaldehyde ........................36, 101 (1985) (corr. 42, 263); Suppl. 7, 77 (1987); 71, 319 (1999) Acetaldehyde associated with the consumption of alcoholic beverages ..............100E, 377 (2012) Acetaldehyde formylmethylhydrazone (see Gyromitrin) Acetamide .................................... 7, 197 (1974); Suppl. 7, 56, 389 (1987); 71, 1211 (1999) Acetaminophen (see Paracetamol) Aciclovir ..............................................................................76, 47 (2000) Acid mists (see Sulfuric acid and other strong inorganic acids, occupational exposures to mists and vapours from) Acridine orange ...................................................16, 145 (1978); Suppl. 7, 56 (1987) Acriflavinium chloride ..............................................13, -
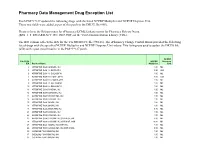
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

Appendix C Medication Tables
Appendix C Medication Tables Note: The medication tables are not meant to be inclusive lists of all available therapeutic agents. Approved medication tables will be updated regularly. Discrepancies must be reported. See Resource Section of this manual for additional contact information. Release Notes: Aspirin Table Version 1.0 Table 1.1 Aspirin and Aspirin-Containing Medications Acetylsalicylic Acid Acuprin 81 Alka-Seltzer Alka-Seltzer Morning Relief Anacin Arthritis Foundation Aspirin Arthritis Pain Ascriptin Arthritis Pain Formula ASA ASA Baby ASA Baby Chewable ASA Baby Coated ASA Bayer ASA Bayer Children's ASA Buffered ASA Children's ASA EC ASA Enteric Coated ASA/Maalox Ascriptin Aspergum Aspir-10 Aspir-Low Aspir-Lox Aspir-Mox Aspir-Trin Aspirbuf Aspircaf Aspirin Aspirin Baby Aspirin Bayer Aspirin Bayer Children's Aspirin Buffered Aspirin Child Aspirin Child Chewable Aspirin Children's Aspirin EC Aspirin Enteric Coated Specifications Manual for National Appendix C-1 Hospital Quality Measures Table 1.1 Aspirin and Aspirin-Containing Medications (continued) Aspirin Litecoat Aspirin Lo-Dose Aspirin Low Strength Aspirin Tri-Buffered Aspirin, Extended Release Aspirin/butalbital/caffeine Aspirin/caffeine Aspirin/pravachol Aspirin/pravastatin Aspirtab Bayer Aspirin Bayer Aspirin PM Extra Strength Bayer Children’s Bayer EC Bayer Enteric Coated Bayer Low Strength Bayer Plus Buffered ASA Buffered Aspirin Buffered Baby ASA Bufferin Bufferin Arthritis Strength Bufferin Extra Strength Buffex Cama Arthritis Reliever Child’s Aspirin Coated Aspirin