The COVID Report Card
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CRITICAL THEORY and AUTHORITARIAN POPULISM Critical Theory and Authoritarian Populism
CDSMS EDITED BY JEREMIAH MORELOCK CRITICAL THEORY AND AUTHORITARIAN POPULISM Critical Theory and Authoritarian Populism edited by Jeremiah Morelock Critical, Digital and Social Media Studies Series Editor: Christian Fuchs The peer-reviewed book series edited by Christian Fuchs publishes books that critically study the role of the internet and digital and social media in society. Titles analyse how power structures, digital capitalism, ideology and social struggles shape and are shaped by digital and social media. They use and develop critical theory discussing the political relevance and implications of studied topics. The series is a theoretical forum for in- ternet and social media research for books using methods and theories that challenge digital positivism; it also seeks to explore digital media ethics grounded in critical social theories and philosophy. Editorial Board Thomas Allmer, Mark Andrejevic, Miriyam Aouragh, Charles Brown, Eran Fisher, Peter Goodwin, Jonathan Hardy, Kylie Jarrett, Anastasia Kavada, Maria Michalis, Stefania Milan, Vincent Mosco, Jack Qiu, Jernej Amon Prodnik, Marisol Sandoval, Se- bastian Sevignani, Pieter Verdegem Published Critical Theory of Communication: New Readings of Lukács, Adorno, Marcuse, Honneth and Habermas in the Age of the Internet Christian Fuchs https://doi.org/10.16997/book1 Knowledge in the Age of Digital Capitalism: An Introduction to Cognitive Materialism Mariano Zukerfeld https://doi.org/10.16997/book3 Politicizing Digital Space: Theory, the Internet, and Renewing Democracy Trevor Garrison Smith https://doi.org/10.16997/book5 Capital, State, Empire: The New American Way of Digital Warfare Scott Timcke https://doi.org/10.16997/book6 The Spectacle 2.0: Reading Debord in the Context of Digital Capitalism Edited by Marco Briziarelli and Emiliana Armano https://doi.org/10.16997/book11 The Big Data Agenda: Data Ethics and Critical Data Studies Annika Richterich https://doi.org/10.16997/book14 Social Capital Online: Alienation and Accumulation Kane X. -

Slovenia Before the Elections
PERSPECTIVE Realignment of the party system – Slovenia before the elections ALEŠ MAVER AND UROŠ URBAS November 2011 The coalition government under Social Democrat Prime make people redundant. Nevertheless, the unemploy- Minister Borut Pahor lost the support it needed in Parlia- ment rate increased by 75 per cent to 107,000 over three ment and early elections had to be called for 4 Decem- years. This policy was financed by loans of 8 billion eu- ber, one year before completing its term of office. What ros, which doubled the public deficit. are the reasons for this development? Which parties are now seeking votes in the »political marketplace«? What However, Prime Minister Pahor overestimated his popu- coalitions are possible after 4 December? And what chal- larity in a situation in which everybody hoped that the lenges will the new government face? economic crisis would soon be over. The governing par- ties had completely different priorities: they were seek- ing economic rents; they could not resist the pressure of Why did the government of lobbies and made concessions; and they were too preoc- Prime Minister Borut Pahor fail? cupied with scandals and other affairs emerging from the ranks of the governing coalition. Although the governing coalition was homogeneously left-wing, it could not work together and registered no significant achievements. The next government will thus Electoral history and development be compelled to achieve something. Due to the deterio- of the party system rating economic situation – for 2012 1 per cent GDP growth, 1.3 per cent inflation, 8.4 per cent unemploy- Since the re-introduction of the multi-party system Slo- ment and a 5.3 per cent budget deficit are predicted – venia has held general elections in 1990, 1992, 1996, the goals will be economic. -

Initiative of President Andrzej Duda Regarding the Change of the Constitution
Teka of Political Science and International Relations – OL PAN/UMCS, 2018, 13/1 DOI: 10.17951/teka.2018.13.1.25-34 INITIATIVE OF PRESIDENT ANDRZEJ DUDA REGARDING THE CHANGE OF THE CONSTITUTION Bożena Dziemidok-Olszewska Maria Curie-Skłodowska University in Lublin Faculty of Political Science, Department of Political Systems e-mail: [email protected] Marta Michalczuk-Wlizło Maria Curie-Skłodowska University in Lublin Faculty of Political Science, Department of Political Systems e-mail: [email protected] Abstract: The objective of the article is to present and evaluate the initiative of President Andrzej Duda regarding the amendment of the Constitution, with which he appeared on 3 May 2017. The activities and presentations of the President in this regard during the previous year and related problems were all demonstrated. The controversies regarding the presidential initiative were di- vided into legal and political. Legal one is the regulation of the institution of referendum in the Constitution of 1997, the political ones result from the opinion and concepts of parties and citizens about the constitution and referendum in its case. Keywords: change of constitution, president, referendum, political science INTRODUCTION During the last year, from 3 May 2017 to 3 May 2018, we witnessed the, still incomplete, process of President Andrzej Duda’s activities regarding the referendum on the amendment to the Constitution of the Republic of Poland. The aim of the article is to present and assess the President’s activities in this area, and also to demonstrate the reactions to the President’s initiative. The research question is the justification, meaningfulness and effectiveness of the presidential initiative; the research hypothesis is the claim that the President’s actions are odd and irrational (pointless). -

H 8302 State of Rhode Island
2018 -- H 8302 ======== LC005884 ======== STATE OF RHODE ISLAND IN GENERAL ASSEMBLY JANUARY SESSION, A.D. 2018 ____________ H O U S E R E S O L U T I O N WELCOMING HIS EXCELLENCY MARCELO REBELO DE SOUSA, PRESIDENT OF THE REPUBLIC OF PORTUGAL AND HIS EXCELLENCY ANTÓNIO COSTA, PRIME MINISTER OF THE REPUBLIC OF PORTUGAL, TO THE STATE OF RHODE ISLAND Introduced By: Representatives Cunha, Solomon, Fellela, Nunes, and Craven Date Introduced: June 07, 2018 Referred To: House read and passed 1 WHEREAS, His Excellency Marcelo Rebelo de Sousa, President of the Republic of 2 Portugal, was born on December 12, 1948, in Lisbon, Portugal, the eldest son of Baltasar Rebelo 3 de Sousa and Maria das Neves Fernandes Duarte. He attained a law degree from the Faculty of 4 Law of the University of Lisbon, and a PhD in Legal and Political Sciences with Distinction and 5 Commendation; and 6 WHEREAS, Throughout the distinguished public service career of President Rebelo de 7 Sousa, he has served with distinction as a government minister, a member of Parliament, a law 8 professor, and as a journalist; and 9 WHEREAS, President Rebelo de Sousa began his professional career as a teacher in the 10 areas of Legal and Political Sciences, and later advanced to serve as the Chairman of the 11 scientific and pedagogical boards and the Institute of Legal and Political Sciences of the Faculty 12 of Law of the University of Lisbon. He also served as a Professor at the Faculty of Social and 13 Human Services and with the Faculty of Law with the Portuguese Catholic University; and 14 WHEREAS, President Rebelo de Sousa also served the citizens of Portugal with honor in 15 the political arena. -

Country Position Name Email Albania President Mr. Ilir Meta [email protected] Prime Minister Mr
Country Position Name Email Albania President Mr. Ilir Meta [email protected] Prime Minister Mr. Edi Rama [email protected] Minister of Foreign Affairs Mr. Ditmir Bushati [email protected] UN Ambassdor in New York H.E. Ms. Besiana Kadare [email protected] UN Ambassdor in Geneva H.E. Ms. Ravesa Lleshi [email protected] Belarus President Mr. Alexander Lukashenko [email protected] Prime Minister Mr. Siarhiej Rumas [email protected] Minister of Foreign Affairs Mr. Vladimir Makei [email protected] UN Ambassdor in New York H.E. Mr. Valentin Rybakov [email protected] UN Ambassdor in Geneva H.E. Mr. Yury Ambrazevich [email protected] Bosnia and HerzegovinaCo-President Mr. Šefik Džaferović [email protected] Co-President Mr. Milorad Dodik [email protected] Co-President Mr. Željko Komšić [email protected] Prime Minister Mr. Zoran Tegeltija [email protected] Minister of Foreign Affairs Mr. Igor Crnadak [email protected] UN Ambassdor in New York H.E. Mr. Sven Alkalaj [email protected] UN Ambassdor in Geneva H.E. Ms. Nermina Kapetanovic [email protected] Bulgaria President Mr. Rumen Radev [email protected] Prime Minister Ms. Boyko Borissov [email protected] Minister of Foreign Affairs Mrs. Ekaterina Spasova Gecheva-Zakharieva [email protected] UN Ambassdor in New York H.E. Mr. Georgi Velikov Panayotov [email protected] UN Ambassdor in Geneva H.E. Ms. Deyana Kostadinova [email protected] Croatia President Mr. Zoran Milanović [email protected] Prime Minister Andrej Plenković [email protected] Minister of Foreign Affairs Mr. -

Agenda EN Blowing
The Week Ahead 11 – 17 April 2016 Plenary session in Strasbourg PNR. Parliament will debate and vote on a provisional agreement with member states on the use of passenger name records (PNR). The passenger data collected by airlines are to be shared with national authorities for the prevention of terrorism and serious crime. A press conference will be held on Wednesday at 14.00. (Debate Wednesday, vote Thursday) Data protection. A reform of data protection laws is also on the agenda. The aim of a regulation is to put internet users in control of their personal data and to regulate data transfers to third countries, while a directive sets high standards on use of data for policing Agenda and judicial purposes. A press conference is scheduled for Tuesday at 12.00. (Debate Wednesday, vote Thursday) EU-Turkey deal. The agreement to return migrants and asylum seekers from Greek islands to Turkey, reached at the meeting of heads of state or government on 18 March in Brussels, will be at the centre of a debate with Council President Donald Tusk and Commission President Jean-Claude Juncker on Wednesday morning. MEPs will also look at the progress made by Turkey towards EU membership. (Debates Wednesday, vote Thursday) Migration and asylum. A centralised asylum system would allow the EU to manage the increasing flows of migrants and asylum seekers better, says a draft resolution which MEPs will debate and vote upon on Tuesday. MEPs advocate safe and lawful ways for third-country nationals to enter the Union without risking their lives and resorting to human smugglers. -
Outcome Report
Outcome Report August, 2019 About the R20 AUSTRIAN WORLD SUMMIT The R20 AUSTRIAN WORLD SUMMIT is a long-term initiative to create a network platform that will help regions, states and cities implement the UN Sustainable Development Goals and meet the global climate protection targets outlined in the Paris Agreement. Our goal is to bring everyone together in order to increase partnerships and exchange experiences and ideas. It is critical that we stay inspired and motivated in our efforts to implement the SDGs and to find effective ways to learn from one another. Arnold Schwarzenegger launched the R20 AUSTRIAN WORLD SUMMIT in 2017, under the direction of R20 Austria&EU Director Monika Langthaler and under the patronage of Federal President Alexander Van der Bellen. On the basis of this initiative, a major international climate conference is held once a year in the Vienna Hofburg. What we want to achieve: • Raising awareness for climate change • Showcasing innovative projects for climate protection • Matchmaking for green solutions Imprint R20 AUSTRIAN WORLD SUMMIT Vienna, August 2019 www.austrianworldsummit.com Outcome Report | R20 AUSTRIAN WORLD SUMMIT 19 2 Table of Content Key Messages ...................................................................................................................................................................... 4 Introduction: Goals and Guests ................................................................................................................................... 4 Opening Show .................................................................................................................................................................... -

Kersti KALJULAID Is a Global Leader Being 5Th President of the Republic of Estonia
Kersti KALJULAID is a global leader being 5th President of the Republic of Estonia. As a firm believer in multilateralism she has spectacular experiences in the fields of economy and energy as well as in public sector, European institutions and international level. Since 2016 President of the Republic of Estonia 2004-2016 Member of the European Court of Auditors 2002-2004 CFO and CEO in Energy sector 1999-2002 Economic Advisor to Prime Minister mr Mart LAAR 1994-1999 different positions in Investment Banking and Telecom sectors INVOLVEMENT IN ORGANISATIONS Since 2018 co-chair of UN High-Level Steering Group „Every Woman Every Child“ 2016-2019 Leading Estonian campaign to UN Security Council 2020-2021 2012-2016 Chair of the Council of University of Tartu 2001-2004 Member of the Supervisory Board of the Estonian Genome Centre Kersti Kaljulaid is also a member of World Bank’s Advisory Panel for the World Development Report 2021 and member of the European Council on Foreign Relations Council. LANGUAGE SKILLS She is fluent in English and French and also speaks German, Finnish, Russian. EDUCATION She graduated from the University of Tartu in 1992 in the field of genetics in the Faculty of Natural Sciences and completed master's studies in the Faculty of Economics and Business Administration in 2001. „Estonia regained its independence in 1991. With 30 years we have gone through comprehensive, rapid and successful reforms, we have built the first truly digital society and developed one of the best education systems in the world according to OECD. These are the experiences I want to bring to the OECD in order to be prepared for the challenges we will face in the next decades.“ Kersti KALJULAID President of the Republic of Estonia . -

'Russia Is a Threat': Estonia Frets About Its Neighbor
Opinions ‘Russia is a threat’: Estonia frets about its neighbor In an interview, President Kersti Kaljulaid says Trump must stand up to Moscow. By Lally Weymouth March 24 Lally Weymouth is a senior associate editor at The Washington Post. TALLINN, ESTONIA Estonian President Kersti Kaljulaid is treading carefully. Sitting in her office this past week, she said she believes Vice President Pence’s assurances that, despite President Trump’s skepticism, the United States is committed to NATO. A NATO battalion just arrived to make this small and vulnerable Baltic nation feel safer from Russia, a powerful neighbor historically ambivalent about its independence. Kaljulaid, chosen last year as a compromise candidate, spoke to The Washington Post’s Lally Weymouth about Vladimir Putin, NATO and a childhood spent under Soviet occupation. Edited excerpts follow. Q. Is Russia a threat? Are you worried? A. Yes, I am worried. Russia is a threat. Not a physical threat to any NATO country but [a threat] to the international security architecture. In 2008, they moved on Georgia. Q. When Russia occupied Abkhazia and South Ossetia? A. That was the first sign. It blew over very quickly — European countries went back to business and life continued. This, of course, taught President Putin a lesson: He could push a little more. Q. He got the message he could do whatever he wants? A. If he does it bit by bit, yes. When he went into Crimea, it stopped for a while because the European countries and America this time recognized that they needed to draw a red line. -

Address by President of the Republic of Poland Mr Andrzej Duda On
Address by President of the Republic of Poland Mr Andrzej Duda on the occasion of the New Year`s meeting with the Diplomatic Corps Presidential Palace, 14 January 2019 Your Excellency, Most Reverend Sir, Dean of the Diplomatic Corps, Your Excellencies, the Ambassadors, Honourable Marshal, Honourable Prime Ministers, Excellencies, Most Reverend Bishops, Honourable Ministers, Madam Justice of the Constitutional Court, Generals, Distinguished Guests, Ladies and Gentlemen, It is my great pleasure to welcome you to our fourth joint New Year`s meeting. 2018 is over, a year rich in numerous events, out of which the most significant, truly momentous ones for us, were undoubtedly the celebrations of the centenary of regaining independence. I wish to thank you warmly for making our jubilee visible also in your home countries; it was often an occasion for grand festivities and joy. Last year we commenced our 2-year-long, non-permanent membership of the United Nations Security Council, whereas in Katowice we presided over the session of the 24th Conference of the Parties to the United Nations Framework Convention on Climate Change. Its successful outcome was reflected in the adoption of the so called Katowice Rulebook, which was possible thanks to the readiness for compromise demonstrated by all parties participating in the negotiations. I would like to thank your countries for cooperation and for expressing acknowledgment of our good and effective organization of the Katowice conference. The year 2018 was marked, once again, by high level of my international activity. Throughout the whole year I paid 26 foreign visits, and met with more than 20 international leaders who visited Poland. -

Young People Are the Future of Entrepreneurial Slovenia
Young people 3rd are the future of entrepreneurial Forum Agenda Slovenia February 3 | Congress Center Brdo | Predoslje 39, 4000 Kranj 8.00–9.00 Dr. Jure Knez, Member of the Board of Directors of SBC, Breakfast with Hofer and registration of Dewesoft participants Matic Vizjak, President of SBC Youth, Vizjak Tjaša Ban Farm, Member of SBC Youth, Protocamel In parallel: Young Entrepreneurship Festival Moderator: Martin Jezeršek, Jezeršek Opening of the forum 9.00-9.15 Studio Commentary: Marjan Batagelj, President of SBC, Postojna Cave Tone Stanovnik, SBC, Spica International 9.15-9.30 Tomaž Lah, SBC, Nectar Natura Borut Pahor, President of the Republic of Slovenia Aljoša Domijan, SBC, Gambit trade LOT 1: YOUNG SLOVENIA COALITION 13.00-14.30 9.30-11.00 Lunch Interview of members of the SBC Club of Slovenian Entrepreneurs with representatives of Slovenian politics 14.30-16.00 on the topic of measures from the SBC 2020-22 Program: LOT 3: HOW TO STRENGTHEN ENTERPRISE “Young people are the future of Slovenia” VALUES (FOR ENTERPRISE SLOVENIA) Participating SBC members: Žiga Gombač, Ambassador for Entrepreneurial Slovenia Marjan Batagelj, SBC President, Postojna Cave Marko Lotrič, Member of the Board of Directors of SBC, Igor Akrapovic, Member of the Board of Directors of SBC, Lotrič Metrology Akrapovič Alenka Knez, Retired Mechanical Engineer, SOS School, Hubert Kosler, Yaskawa Slovenia Ambassador for Entrepreneurial Slovenia Jana Fleisher, Member of SBC Youth, Kindergarten Good Sašo Palčič, Member of SBC Youth, Madwise Aunt Moderator: Moderator: -
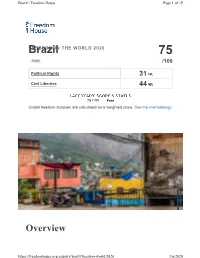
Freedom in the World Report 2020
Brazil | Freedom House Page 1 of 19 BrazilFREEDOM IN THE WORLD 2020 75 FREE /100 Political Rights 31 Civil Liberties 44 75 Free Global freedom statuses are calculated on a weighted scale. See the methodology. Overview https://freedomhouse.org/country/brazil/freedom-world/2020 3/6/2020 Brazil | Freedom House Page 2 of 19 Brazil is a democracy that holds competitive elections, and the political arena is characterized by vibrant public debate. However, independent journalists and civil society activists risk harassment and violent attack, and the government has struggled to address high rates of violent crime and disproportionate violence against and economic exclusion of minorities. Corruption is endemic at top levels, contributing to widespread disillusionment with traditional political parties. Societal discrimination and violence against LGBT+ people remains a serious problem. Key Developments in 2019 • In June, revelations emerged that Justice Minister Sérgio Moro, when he had served as a judge, colluded with federal prosecutors by offered advice on how to handle the corruption case against former president Luiz Inácio “Lula” da Silva, who was convicted of those charges in 2017. The Supreme Court later ruled that defendants could only be imprisoned after all appeals to higher courts had been exhausted, paving the way for Lula’s release from detention in November. • The legislature’s approval of a major pension reform in the fall marked a victory for Brazil’s far-right president, Jair Bolsonaro, who was inaugurated in January after winning the 2018 election. It also signaled a return to the business of governing, following a period in which the executive and legislative branches were preoccupied with major corruption scandals and an impeachment process.