Embryo and Its Mitochondria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Placement of Children with Relatives
STATE STATUTES Current Through January 2018 WHAT’S INSIDE Placement of Children With Giving preference to relatives for out-of-home Relatives placements When a child is removed from the home and placed Approving relative in out-of-home care, relatives are the preferred placements resource because this placement type maintains the child’s connections with his or her family. In fact, in Placement of siblings order for states to receive federal payments for foster care and adoption assistance, federal law under title Adoption by relatives IV-E of the Social Security Act requires that they Summaries of state laws “consider giving preference to an adult relative over a nonrelated caregiver when determining a placement for a child, provided that the relative caregiver meets all relevant state child protection standards.”1 Title To find statute information for a IV-E further requires all states2 operating a title particular state, IV-E program to exercise due diligence to identify go to and provide notice to all grandparents, all parents of a sibling of the child, where such parent has legal https://www.childwelfare. gov/topics/systemwide/ custody of the sibling, and other adult relatives of the laws-policies/state/. child (including any other adult relatives suggested by the parents) that (1) the child has been or is being removed from the custody of his or her parents, (2) the options the relative has to participate in the care and placement of the child, and (3) the requirements to become a foster parent to the child.3 1 42 U.S.C. -

Lecture 19 Placentation and Maternal Recognition of Pregnancy
Blastulation Gap Junctions Lecture 19 Inner Cell Mass Zona Pellucida Placentation and Maternal Recognition of Pregnancy Trophectoderm Na+ [Na+] Animal Science 434 John J. Parrish H2O Tight Junctions Hatching Conceptus Growth Cow • Day 15, 1-2 mm Occurs in cow, pig and sheep Bovine • Day 18-19, 10-20 cm »9 - 11 days Spherical Embryonic Equine, Ovine Area »7 - 8 days Porcine Tubular Elongating »6 days Trophoblast Filamentous Mare remains spherical! Development of Porcine Conceptuses Elongated Day 15 Porcine from Day 10 to 12 Conceptus 5 mm Spherical 10 mm Spherical Inner Cell Mass 15 mm Tubular 150 mm Filamentous Embryo 1 Uterine Location of Elongating Pig Intrauterine Migration Ruminant Blastocyst Day 5 Corpus Luteum Bovine and Ovine Pig Intrauterine Migration Pig Intrauterine Migration Day 7 Day 12 Embryos become fixed Transuterine migration is rare in cow and ewe! Trans-uterine Migration in the Mare Gastrulation Begins Day 10 Inner Cell Mass Trophectoderm Formation Endoderm of Germ Fixation can Fixation occur in either on day Layers horn! 15 - 16 Blastocoele Corpus Cavity Luteum 2 Gastrulation Gastrulation Endoderrm Endoderrm Yolk Sack Yolk Sack Gastrula Gastrula Ectoderm Ectoderm Mesoderm Ectoderm Trophectoderm Trophectoderm Extraembryonic Coelom Yolk Sack Endoderm Endoderm Trophectoderm (Chorion) Germ Layers Placenta Formation Embryonic Amniotic Folds Ectoderm Mesoderm Endoderm Ectoderm » CNS » Circulatory » Digestive » Sense organs » Skeletal » Liver » Mammary » Muscle » Lungs glands » Reproductive » Pancreas Extraembryonic » -

Human Blastocyst Morphological Quality Is Significantly Improved In
Human blastocyst morphological quality is significantly improved in embryos classified as fast on day 3 (R10 cells), bringing into question current embryological dogma Martha Luna, M.D.,a,b Alan B. Copperman, M.D.,a,b Marlena Duke, M.Sc.,a,b Diego Ezcurra, D.V.M.,c Benjamin Sandler, M.D.,a,b and Jason Barritt, Ph.D.a,b a Mount Sinai School of Medicine, Department of Obstetrics and Gynecology, Department of Reproductive Endocrinology and Infertility, and b Reproductive Medicine Associates of New York, New York, New York; and c EMD Serono, Rockland, Massachusetts Objective: To evaluate developmental potential of fast cleaving day 3 embryos. Design: Retrospective analysis. Setting: Academic reproductive center. Patient(s): Three thousand five hundred twenty-nine embryos. Intervention(s): Day 3 embryos were classified according to cell number: slow cleaving: %6 cells, intermediate cleaving: 7–9 cells, and fast cleaving: R10 cells, and further evaluated on day 5. The preimplantation genetic diagnosis (PGD) results of 43 fast cleaving embryos were correlated to blastocyst formation. Clinical outcomes of transfers involving only fast cleaving embryos (n ¼ 4) were evaluated. Main Outcome Measure(s): Blastocyst morphology correlated to day 3 blastomere number. Relationship between euploidy and blastocyst formation of fast cleaving embryos. Implantation, pregnancy (PR), and birth rates resulting from fast embryo transfers. Result(s): Blastocyst formation rate was significantly greater in the intermediate cleaving (72.7%) and fast cleav- ing (54.2%) groups when compared to the slow cleaving group (38%). Highest quality blastocysts were formed significantly more often in the fast cleaving group. Twenty fast cleaving embryos that underwent PGD, formed blastocysts, of which 45% (9/20) were diagnosed as euploid. -

Animal Form & Function
Animals Animal Form & Function By far, most diversity of bauplane (body forms). And most variations within bauplane. Animals are Animated “ANIMAL” ≠ MAMMAL — Fascinating Behaviors Animal Cells • Eukaryotic • No cell wall No plastids No central vacuole • Multicellular: – extensive specialization & differentiation – unique cell-cell junctions Heyer 1 Animals Animals Blastulation & Gastrulation • Motile • Early embryonic development in animals 3 In most animals, cleavage results in the formation of a multicellular stage called a 1 The zygote of an animal • Highly differentiated blastula. The blastula of many animals is a undergoes a succession of mitotic tissues cell divisions called cleavage. hollow ball of cells. Blastocoel • Intercellular junctions Cleavage Cleavage – tissue-specific cadherins 6 The endoderm of the archenteron develops into Eight-cell stage Blastula Cross section Zygote • Extracellular protein the the animal’s of blastula fibers digestive tract. Blastocoel Endoderm – collagen 5 The blind pouch formed by gastrulation, called Ectoderm • Diploid life cycle the archenteron, opens to the outside Gastrula Gastrulation via the blastopore. Blastopore 4 Most animals also undergo gastrulation, a • Blastula/gastrula rearrangement of the embryo in which one end of the embryo folds inward, expands, and eventually fills the embryo blastocoel, producing layers of embryonic tissues: the Figure 32.2 ectoderm (outer layer) and the endoderm (inner layer). Primary embryonic germ layers Primary embryonic germ layers • Diploblastic: two germ -
Ferns of the National Forests in Alaska
Ferns of the National Forests in Alaska United States Forest Service R10-RG-182 Department of Alaska Region June 2010 Agriculture Ferns abound in Alaska’s two national forests, the Chugach and the Tongass, which are situated on the southcentral and southeastern coast respectively. These forests contain myriad habitats where ferns thrive. Most showy are the ferns occupying the forest floor of temperate rainforest habitats. However, ferns grow in nearly all non-forested habitats such as beach meadows, wet meadows, alpine meadows, high alpine, and talus slopes. The cool, wet climate highly influenced by the Pacific Ocean creates ideal growing conditions for ferns. In the past, ferns had been loosely grouped with other spore-bearing vascular plants, often called “fern allies.” Recent genetic studies reveal surprises about the relationships among ferns and fern allies. First, ferns appear to be closely related to horsetails; in fact these plants are now grouped as ferns. Second, plants commonly called fern allies (club-mosses, spike-mosses and quillworts) are not at all related to the ferns. General relationships among members of the plant kingdom are shown in the diagram below. Ferns & Horsetails Flowering Plants Conifers Club-mosses, Spike-mosses & Quillworts Mosses & Liverworts Thirty of the fifty-four ferns and horsetails known to grow in Alaska’s national forests are described and pictured in this brochure. They are arranged in the same order as listed in the fern checklist presented on pages 26 and 27. 2 Midrib Blade Pinnule(s) Frond (leaf) Pinna Petiole (leaf stalk) Parts of a fern frond, northern wood fern (p. -

Stages of Embryonic Development of the Zebrafish
DEVELOPMENTAL DYNAMICS 2032553’10 (1995) Stages of Embryonic Development of the Zebrafish CHARLES B. KIMMEL, WILLIAM W. BALLARD, SETH R. KIMMEL, BONNIE ULLMANN, AND THOMAS F. SCHILLING Institute of Neuroscience, University of Oregon, Eugene, Oregon 97403-1254 (C.B.K., S.R.K., B.U., T.F.S.); Department of Biology, Dartmouth College, Hanover, NH 03755 (W.W.B.) ABSTRACT We describe a series of stages for Segmentation Period (10-24 h) 274 development of the embryo of the zebrafish, Danio (Brachydanio) rerio. We define seven broad peri- Pharyngula Period (24-48 h) 285 ods of embryogenesis-the zygote, cleavage, blas- Hatching Period (48-72 h) 298 tula, gastrula, segmentation, pharyngula, and hatching periods. These divisions highlight the Early Larval Period 303 changing spectrum of major developmental pro- Acknowledgments 303 cesses that occur during the first 3 days after fer- tilization, and we review some of what is known Glossary 303 about morphogenesis and other significant events that occur during each of the periods. Stages sub- References 309 divide the periods. Stages are named, not num- INTRODUCTION bered as in most other series, providing for flexi- A staging series is a tool that provides accuracy in bility and continued evolution of the staging series developmental studies. This is because different em- as we learn more about development in this spe- bryos, even together within a single clutch, develop at cies. The stages, and their names, are based on slightly different rates. We have seen asynchrony ap- morphological features, generally readily identi- pearing in the development of zebrafish, Danio fied by examination of the live embryo with the (Brachydanio) rerio, embryos fertilized simultaneously dissecting stereomicroscope. -

The Origin of Alternation of Generations in Land Plants
Theoriginof alternation of generations inlandplants: afocuson matrotrophy andhexose transport Linda K.E.Graham and LeeW .Wilcox Department of Botany,University of Wisconsin, 430Lincoln Drive, Madison,WI 53706, USA (lkgraham@facsta¡.wisc .edu ) Alifehistory involving alternation of two developmentally associated, multicellular generations (sporophyteand gametophyte) is anautapomorphy of embryophytes (bryophytes + vascularplants) . Microfossil dataindicate that Mid ^Late Ordovicianland plants possessed such alifecycle, and that the originof alternationof generationspreceded this date.Molecular phylogenetic data unambiguously relate charophyceangreen algae to the ancestryof monophyletic embryophytes, and identify bryophytes as early-divergentland plants. Comparison of reproduction in charophyceans and bryophytes suggests that the followingstages occurredduring evolutionary origin of embryophytic alternation of generations: (i) originof oogamy;(ii) retention ofeggsand zygotes on the parentalthallus; (iii) originof matrotrophy (regulatedtransfer ofnutritional and morphogenetic solutes fromparental cells tothe nextgeneration); (iv)origin of a multicellularsporophyte generation ;and(v) origin of non-£ agellate, walled spores. Oogamy,egg/zygoteretention andmatrotrophy characterize at least some moderncharophyceans, and arepostulated to represent pre-adaptativefeatures inherited byembryophytes from ancestral charophyceans.Matrotrophy is hypothesizedto have preceded originof the multicellularsporophytes of plants,and to represent acritical innovation.Molecular -
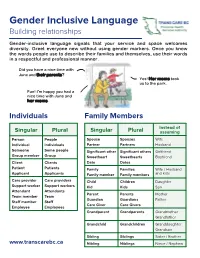
Gender Inclusive Language Building Relationships
Gender Inclusive Language Building relationships Gender-inclusive language signals that your service and space welcomes diversity. Greet everyone new without using gender markers. Once you know the words people use to describe their families and themselves, use their words in a respectful and professional manner. Did you have a nice time with June and their parents? Yes! Her moms took us to the park. Fun! I'm happy you had a nice time with June and her moms. Individuals Family Members Instead of Singular Plural Singular Plural assuming Person People Spouse Spouses Wife Individual Individuals Partner Partners Husband Someone Some people Significant other Significant others Girlfriend Group member Group Sweetheart Sweethearts Boyfriend Client Clients Date Dates Patient Patients Family Families Wife / Husband Applicant Applicants Family member Family members and kids Care provider Care providers Child Children Daughter Support worker Support workers Kid Kids Son Attendant Attendants Parent Parents Mother Team member Team Guardian Guardians Father Staff member Staff Care Giver Care Givers Employee Employees Grandparent Grandparents Grandmother Grandfather Grandchild Grandchildren Granddaughter Grandson Sibling Siblings Sister / Brother www.transcarebc.ca Nibling Niblings Niece / Nephew ii Pronouns (using they in the singular) If you are in a setting where your interactions with people are brief, you may not have time to get to know the person. Using the singular they in these situations can help to avoid pronoun mistakes. subject They They are waiting at the door. object Them The form is for them. possessive Their Their parents will pick them up at 3pm. adjective possessive Theirs They said the wheelchair is not theirs. -

Vertebrate Embryonic Cleavage Pattern Determination
Chapter 4 Vertebrate Embryonic Cleavage Pattern Determination Andrew Hasley, Shawn Chavez, Michael Danilchik, Martin Wühr, and Francisco Pelegri Abstract The pattern of the earliest cell divisions in a vertebrate embryo lays the groundwork for later developmental events such as gastrulation, organogenesis, and overall body plan establishment. Understanding these early cleavage patterns and the mechanisms that create them is thus crucial for the study of vertebrate develop- ment. This chapter describes the early cleavage stages for species representing ray- finned fish, amphibians, birds, reptiles, mammals, and proto-vertebrate ascidians and summarizes current understanding of the mechanisms that govern these pat- terns. The nearly universal influence of cell shape on orientation and positioning of spindles and cleavage furrows and the mechanisms that mediate this influence are discussed. We discuss in particular models of aster and spindle centering and orien- tation in large embryonic blastomeres that rely on asymmetric internal pulling forces generated by the cleavage furrow for the previous cell cycle. Also explored are mechanisms that integrate cell division given the limited supply of cellular building blocks in the egg and several-fold changes of cell size during early devel- opment, as well as cytoskeletal specializations specific to early blastomeres A. Hasley • F. Pelegri (*) Laboratory of Genetics, University of Wisconsin—Madison, Genetics/Biotech Addition, Room 2424, 425-G Henry Mall, Madison, WI 53706, USA e-mail: [email protected] S. Chavez Division of Reproductive & Developmental Sciences, Oregon National Primate Research Center, Department of Physiology & Pharmacology, Oregon Heath & Science University, 505 NW 185th Avenue, Beaverton, OR 97006, USA Division of Reproductive & Developmental Sciences, Oregon National Primate Research Center, Department of Obstetrics & Gynecology, Oregon Heath & Science University, 505 NW 185th Avenue, Beaverton, OR 97006, USA M. -
Placement Process Resource Guide
Placement Process Resource Guide Updated September 2021 Table of Contents Table of Contents ..................................................................................................................................... i The Placement Process Overview ......................................................................................................... 1 Definition of Placement ........................................................................................................................ 1 Initial Placement .................................................................................................................................... 2 Short-Term Emergency Placements .................................................................................................... 2 Subsequent Placements ........................................................................................................................ 2 Placement Types and Definitions ......................................................................................................... 3 Own Home ............................................................................................................................................. 3 Substitute Care ....................................................................................................................................... 3 Regulated Foster Care........................................................................................................................... 4 Types of Regulated -
Development of Chick Development of Chick
Unit 15 Development of Chick UNIT 15 DEVELOPMENT OF CHICK StructureStructureStructure 15.1 Introduction Fully Formed Gastrula Objectives 15.6 Neurulation in Chick 15.2 Structure of Egg of Chick Mechanisms of Neural Plate 15.3 Fertilisation Formation 15.4 Cleavage and Blastulation Morphogenesis of Mesodermal Derivatives 15.5 Gastrulation 15.7 Folding of Embryo Role of Hypoblast 15.8 Development of Extra- Fate Map Embryonic Membranes The Gastrulation Process: Development of Amnion and Formation of Primitive Streak Chorion Completion of Endoderm Development of Allantois Regression of Primitive Streak 15.9 Hatching Epiboly of Ectoderm 15.10 Summary Characteristic Features of 15.11 Terminal Questions Avian Gastrulation 15.12 Answers Comparison with Amphibian Gastrulation 15.1 INTRODUCTION Different animals have evolved a variety of strategies of development. However, since all animals are related, the basic mechanism of early development has been conserved in the course of evolution, and so there are some important similarities in early embryonic development of all metazoan animals as you have already learnt in Block 3. This unit speaks about development of chick as an example of an amniote organism. Recall that amniotes are those vertebrates (reptiles, birds and mammals) that have a water sac or amnion surrounding the developing 163 Block 4 Developmental Biology of Vertebrates-II organism protecting it from the external environment. Chick has been one of the first model organisms to be studied in detail as it is easy to maintain and large enough to be manipulated surgically and genetically during all stages of development. You will study about strictly coordinated sequential changes that take place during the course of chick development viz. -

Extracellular Vesicles Secreted During Blastulation Show Viability of Bovine Embryos
158 6 REPRODUCTIONRESEARCH Extracellular vesicles secreted during blastulation show viability of bovine embryos Edwin A Mellisho, Mario A Briones, Alejandra E Velásquez, Joel Cabezas, Fidel O Castro and Lleretny Rodríguez-Álvarez Laboratory of Animal Biotechnology, Department of Animal Science, Faculty of Veterinary Science, Universidad de Concepcion, Chillan, Chile Correspondence should be addressed to L Rodríguez-Álvarez; Email: [email protected] Abstract Extracellular vesicles (EVs) secreted by blastocysts may be clinically relevant, as indicator of embryo viability on in vitro fertilization. We tested if the characteristics of EVs secreted during blastulation are related to embryo viability. Morulae were individually cultured in SOF media depleted of EVs until day 7.5 post IVF. Viable embryos were determined by a system of extended in vitro culture of bovine embryos until day 11 (post-hatching development). Afterward, a retrospective classification of blastocyst and culture media was performed based on blastulation time (early blastulation (EB) or late blastulation (LB)) and post-hatching development at day 11 (viable (V) or non-viable embryo (NV)). A total of 254 blastocysts and their culture media were classified in four groups (V-EB, NV-EB, V-LB, NV-LB). Group V-EB had a larger blastocyst diameter (170.8 μm), higher proportion of good-quality blastocysts (77%) and larger mean size of population of EVs (122.9 nm), although the highest concentration of EVs (5.75 × 109 particles/mL) were in group NV-EB. Furthermore, small RNA sequencing detected two biotypes, miRNA (86–91%) and snoRNA (9–14%), with a total of 182 and 32 respectively. In differential expression analysis of miRNAs between V versus NV blastocysts, there were 12 miRNAs upregulated and 15 miRNAs downregulated.