Ghrelin Regulates Glucose and Glutamate Transporters In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Compromised Glutamate Transport in Human Glioma Cells: Reduction
The Journal of Neuroscience, December 15, 1999, 19(24):10767–10777 Compromised Glutamate Transport in Human Glioma Cells: Reduction–Mislocalization of Sodium-Dependent Glutamate Transporters and Enhanced Activity of Cystine–Glutamate Exchange Zu-Cheng Ye,1 Jeffrey D. Rothstein,2 and Harald Sontheimer1 1Department of Neurobiology, The University of Alabama at Birmingham, Birmingham, Alabama 35294, and 2Department of Neurology, Johns Hopkins University, Baltimore, Maryland 21287 1 Elevated levels of extracellular glutamate ([Glu]o ) can induce 50% of glutamate transport was Na -independent and medi- 2 seizures and cause excitotoxic neuronal cell death. This is ated by a cystine–glutamate exchanger (system xc ). Extracel- normally prevented by astrocytic glutamate uptake. Neoplastic lular L-cystine dose-dependently induced glutamate release transformation of human astrocytes causes malignant gliomas, from glioma cells. Glutamate release was enhanced by extra- which are often associated with seizures and neuronal necrosis. cellular glutamine and inhibited by (S)-4-carboxyphenylglycine, Here, we show that Na 1-dependent glutamate uptake in gli- which blocked cystine–glutamate exchange. These data sug- oma cell lines derived from human tumors (STTG-1, D-54MG, gest that the unusual release of glutamate from glioma cells is D-65MG, U-373MG, U-251MG, U-138MG, and CH-235MG) is caused by reduction–mislocalization of Na 1-dependent gluta- up to 100-fold lower than in astrocytes. Immunohistochemistry mate transporters in conjunction with upregulation of cystine– and subcellular fractionation show very low expression levels of glutamate exchange. The resulting glutamate release from gli- the astrocytic glutamate transporter GLT-1 but normal expres- oma cells may contribute to tumor-associated necrosis and sion levels of another glial glutamate transporter, GLAST. -

The Vesicular Glutamate Transporter (VGLUT): Heterologous Expression, Proteoliposome, Computational and Mass Spectral Studies
University of Montana ScholarWorks at University of Montana Graduate Student Theses, Dissertations, & Professional Papers Graduate School 2008 The vesicular glutamate transporter (VGLUT): heterologous expression, proteoliposome, computational and mass spectral studies Chih-Kai Chao The University of Montana Follow this and additional works at: https://scholarworks.umt.edu/etd Let us know how access to this document benefits ou.y Recommended Citation Chao, Chih-Kai, "The vesicular glutamate transporter (VGLUT): heterologous expression, proteoliposome, computational and mass spectral studies" (2008). Graduate Student Theses, Dissertations, & Professional Papers. 1107. https://scholarworks.umt.edu/etd/1107 This Dissertation is brought to you for free and open access by the Graduate School at ScholarWorks at University of Montana. It has been accepted for inclusion in Graduate Student Theses, Dissertations, & Professional Papers by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. THE VESICULAR GLUTAMATE TRANSPORTER (VGLUT): HETEROLOGOUS EXPRESSION, PROTEOLIPOSOME, COMPUTATIONAL AND MASS SPECTRAL STUDIES By Chih-Kai Chao Master of Science in Pharmaceutical Sciences, National Taiwan University, Taiwan, 1997 Bachelor of Science in Pharmacy, China Medical College, Taiwan, 1991 Dissertation presented in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Pharmacology/Pharmaceutical Sciences The University of Montana Missoula, MT Autumn 2008 Approved by: Dr. Perry J. Brown, Associate Provost Graduate Education Dr. Charles M. Thompson, Chair Department of Biomedical and Pharmaceutical Sciences Dr. Mark L. Grimes Department of Biological Sciences Dr. Diana I. Lurie Department of Biomedical and Pharmaceutical Sciences Dr. Keith K. Parker Department of Biomedical and Pharmaceutical Sciences Dr. David J. -
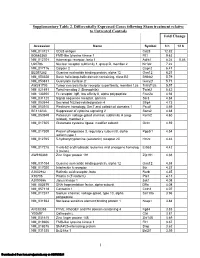
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -

Amino Acid Transporters As Tetraspanin TM4SF5 Binding Partners Jae Woo Jung1,Jieonkim2,Eunmikim2 and Jung Weon Lee 1,2
Jung et al. Experimental & Molecular Medicine (2020) 52:7–14 https://doi.org/10.1038/s12276-019-0363-7 Experimental & Molecular Medicine REVIEW ARTICLE Open Access Amino acid transporters as tetraspanin TM4SF5 binding partners Jae Woo Jung1,JiEonKim2,EunmiKim2 and Jung Weon Lee 1,2 Abstract Transmembrane 4 L6 family member 5 (TM4SF5) is a tetraspanin that has four transmembrane domains and can be N- glycosylated and palmitoylated. These posttranslational modifications of TM4SF5 enable homophilic or heterophilic binding to diverse membrane proteins and receptors, including growth factor receptors, integrins, and tetraspanins. As a member of the tetraspanin family, TM4SF5 promotes protein-protein complexes for the spatiotemporal regulation of the expression, stability, binding, and signaling activity of its binding partners. Chronic diseases such as liver diseases involve bidirectional communication between extracellular and intracellular spaces, resulting in immune-related metabolic effects during the development of pathological phenotypes. It has recently been shown that, during the development of fibrosis and cancer, TM4SF5 forms protein-protein complexes with amino acid transporters, which can lead to the regulation of cystine uptake from the extracellular space to the cytosol and arginine export from the lysosomal lumen to the cytosol. Furthermore, using proteomic analyses, we found that diverse amino acid transporters were precipitated with TM4SF5, although these binding partners need to be confirmed by other approaches and in functionally relevant studies. This review discusses the scope of the pathological relevance of TM4SF5 and its binding to certain amino acid transporters. 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; Introduction on the plasma membrane and the mitochondria, lyso- Importing and exporting biological matter in and out of some, and other intracellular organelles. -

Elucidating the Roles of TCAP-1 on Glucose Transport and Muscle Physiology
Elucidating the roles of TCAP-1 on glucose transport and muscle physiology by Yani Chen A thesis submitted in conformity with the requirements for the degree of Masters of Science in Cell and Systems Biology Department of Cell and Systems Biology University of Toronto © Copyright by Yani Chen (2014) Elucidating the roles of TCAP-1 on glucose transport and muscle physiology Yani Chen For the degree of Masters of Science in Cell and Systems Biology (2014) Department of Cell and Systems Biology University of Toronto Abstract Teneurin C-terminal associated peptide (TCAP)-1 is a cleavable bioactive peptide on the carboxy terminus of teneurin proteins. Previous findings indicate that the primary role of TCAP-1 may be to regulate metabolic optimization in the brain by increasing the efficiency of glucose transport and energy utilization. The findings show that TCAP-1 administration in rats results in a 20-30% decrease in plasma glucose levels and an increase in 18F-2-deoxyglucose uptake into the cortex. In vitro, TCAP-1 also induces 3H-deoxyglucose transport into hypothalamic neurons via an insulin-independent manner. This is correlated with an increase in membrane GLUT3 immunoreactivity. A previously deduced pathway by which TCAP-1 signals in vitro was used to establish a link between the MEK-ERK1/2 pathway and glucose uptake as well as a connection between the MEK-ERK1/2 and AMPK pathways. Immunoreactivity studies indicate that the TCAP-1 system exists in muscle and may play a part in skeletal muscle metabolism and physiology. ii Acknowledgements Throughout the duration of my graduate studies, I have been blessed to have experienced so many opportunities to learn, mature as a person, and interact with so many wonderful people. -

Neuronal Regulation of Glutamate Transporter Subtype Expression in Astrocytes
The Journal of Neuroscience, February 1, 1997, 17(3):932–940 Neuronal Regulation of Glutamate Transporter Subtype Expression in Astrocytes Raymond A. Swanson,1 Jialing Liu,1 Johann W. Miller,1 Jeffrey D. Rothstein,2 Kevin Farrell,1 Becky A. Stein,1 and Maria C. Longuemare1 1Department of Neurology, University of California, San Francisco and Veterans Affairs Medical Center, San Francisco, California 94121, and 2Deparment of Neuroscience, The Johns Hopkins Medical Center, Baltimore, Maryland 21287 GLT-1, GLAST, and EAAC1 are high-affinity, Na1-dependent cytes expressing only GLAST, the dBcAMP-treated cultures glutamate transporters identified in rat forebrain. The expres- expressing both GLAST and GLT-1 showed an increase in sion of these transporter subtypes was characterized in three glutamate uptake Vmax, but no change in the glutamate Km and preparations: undifferentiated rat cortical astrocyte cultures, no increased sensitivity to inhibition by dihydrokainate. astrocytes cocultured with cortical neurons, and astrocyte cul- Pyrrolidine-2,4-dicarboxylic acid and threo-b-hydroxyaspartic tures differentiated with dibutyryl cyclic AMP (dBcAMP). The acid caused relatively less inhibition of transport in cultures undifferentiated astrocyte monocultures expressed only the expressing both GLAST and GLT-1, suggesting a weaker effect GLAST subtype. Astrocytes cocultured with neurons devel- at GLT-1 than at GLAST. These studies show that astrocyte oped a stellate morphology and expressed both GLAST and expression of glutamate transporter subtypes is influenced by GLT-1; neurons expressed only the EAAC1 transporter, and neurons, and that dBcAMP can partially mimic this influence. rare microglia in these cultures expressed GLT-1. Treatment of Manipulation of transporter expression in astrocyte cultures astrocyte cultures with dBcAMP induced expression of GLT-1 may permit identification of factors regulating the expression and increased expression of GLAST. -

Glutamate Mediates Acute Glucose Transport Inhibition in Hippocampal Neurons
The Journal of Neuroscience, October 27, 2004 • 24(43):9669–9673 • 9669 Brief Communication Glutamate Mediates Acute Glucose Transport Inhibition in Hippocampal Neurons Omar H. Porras, Anitsi Loaiza, and L. Felipe Barros Centro de Estudios Cientı´ficos, Casilla 1469, Valdivia, Chile Although it is known that brain activity is fueled by glucose, the identity of the cell type that preferentially metabolizes the sugar remains elusive. To address this question, glucose uptake was studied simultaneously in cultured hippocampal neurons and neighboring astro- cytes using a real-time assay based on confocal epifluorescence microscopy and fluorescent glucose analogs. Glutamate, although stimulating glucose transport in astrocytes, strongly inhibited glucose transport in neurons, producing in few seconds a 12-fold increase in the ratio of astrocytic-to-neuronal uptake rate. Neuronal transport inhibition was reversible on removal of the neurotransmitter and displayed an IC50 of 5 M, suggesting its occurrence at physiological glutamate concentrations. The phenomenon was abolished by CNQX and mimicked by AMPA, demonstrating a role for the cognate subset of ionotropic glutamate receptors. Transport inhibition required extracellular sodium and calcium and was mimicked by veratridine but not by membrane depolarization with high K ϩ or by calcium overloading with ionomycin. Therefore, glutamate inhibits glucose transport via AMPA receptor-mediated sodium entry, whereas calcium entry plays a permissive role. This phenomenon suggests that glutamate redistributes glucose toward astrocytes and away from neurons and represents a novel molecular mechanism that may be important for functional imaging of the brain using positron emission tomography. Key words: glucose; glutamate; neuron; membrane transport; 2-NBDG; 6-NBDG; AMPA Introduction tretti, 1994), which, together with the activation of astrocytic Energy consumption in the mammalian brain is supplied by the glycogen degradation (Shulman et al., 2001), may explain the oxidation of glucose. -

Functional Comparisons of Three Glutamate Transporter Subtypes Cloned from Human Motor Cortex
The Journal of Neuroscience, September 1994, 14(g): 5559-5569 Functional Comparisons of Three Glutamate Transporter Subtypes Cloned from Human Motor Cortex Jeffrey L. Arriza, Wendy A. Fairman, Jacques I. Wadiche, Geoffrey H. Murdoch, Michael P. Kavanaugh, and Susan G. Amara The Vellum Institute for Advanced Biomedical Research, Oregon Health Sciences University, Portland, Oregon 97201 Reuptake plays an important role in regulating synaptic and peripheral tissues(Christensen, 1990) and in the nervous system extracellular concentrations of glutamate. Three glutamate (Kanner and Schuldiner, 1987; Nicholls and Attwell, 1990). transporters expressed in human motor cortex, termed Transport serves a special function in the brain by mediating EAATl , EAATP, and EAAT3 (for excitatory amino acid trans- the reuptake of glutamate releasedat excitatory synapses.Glu- porter), have been characterized by their molecular cloning tamate can be reaccumulated from the synaptic cleft by the and functional expression. Each EAAT subtype mRNA was presynaptic nerve terminal (Eliasof and Werblin, 1993) or by found in all human brain regions analyzed. The most prom- glial uptake of transmitter diffusing from the cleft (Nicholls and inent regional variation in message content was in cerebel- Attwell, 1990; Schwartz and Tachibana, 1990; Barbour et al., lum where EAATl expression predominated. EAATl and 199 1). The activities of neuronal and glial transporters influence EAAT3 mRNAs were also expressed in various non-nervous the temporal and spatial dynamics of the chemical signal in tissues, whereas expression of EAATS was largely restricted other neurotransmitter systems(Hille, 1992; Bruns et al., 1993; to brain. The kinetic parameters and pharmacological char- Isaacsonet al., 1993), but such effects have not yet been dem- acteristics of transport mediated by each EAAT subtype onstrated at glutamatergic synapses(Hestrin et al., 1990; Sar- were determined in transfected mammalian cells by radio- antis et al., 1993). -

Drosophila Glia: Models for Human Neurodevelopmental and Neurodegenerative Disorders
International Journal of Molecular Sciences Review Drosophila Glia: Models for Human Neurodevelopmental and Neurodegenerative Disorders Taejoon Kim, Bokyeong Song and Im-Soon Lee * Department of Biological Sciences, Center for CHANS, Konkuk University, Seoul 05029, Korea; [email protected] (T.K.); [email protected] (B.S.) * Correspondence: [email protected] Received: 31 May 2020; Accepted: 7 July 2020; Published: 9 July 2020 Abstract: Glial cells are key players in the proper formation and maintenance of the nervous system, thus contributing to neuronal health and disease in humans. However, little is known about the molecular pathways that govern glia–neuron communications in the diseased brain. Drosophila provides a useful in vivo model to explore the conserved molecular details of glial cell biology and their contributions to brain function and disease susceptibility. Herein, we review recent studies that explore glial functions in normal neuronal development, along with Drosophila models that seek to identify the pathological implications of glial defects in the context of various central nervous system disorders. Keywords: glia; glial defects; Drosophila models; CNS disorders 1. Introduction Glial cells perform many important functions that are essential for the proper development and maintenance of the nervous system [1]. During development, glia maintain neuronal cell numbers and engulf unnecessary cells and projections, correctly shaping neural circuits. In comparison, glial cells in the adult brain provide metabolic sustenance and critical immune support. Thus, the dysfunction of glial activity contributes to various central nervous system (CNS) disorders in humans at different stages of life [2]. Accordingly, the need for research regarding the initiation as well as the progression of disorders associated with glial cell dysfunction is increasing. -

Regulated Transport of the Glucose Transporter Glut4
REVIEWS REGULATED TRANSPORT OF THE GLUCOSE TRANSPORTER GLUT4 Nia J. Bryant, Roland Govers and David E. James In muscle and fat cells, insulin stimulates the delivery of the glucose transporter GLUT4 from an intracellular location to the cell surface, where it facilitates the reduction of plasma glucose levels. Understanding the molecular mechanisms that mediate this translocation event involves integrating our knowledge of two fundamental processes — the signal transduction pathways that are triggered when insulin binds to its receptor and the membrane transport events that need to be modified to divert GLUT4 from intracellular storage to an active plasma membrane shuttle service. FACILITATIVE SUGAR Glucose is a fundamental source of energy for all glucose-transport system, the activity of which can be TRANSPORTER eukaryotic cells. In humans, although all cells use glu- rapidly upregulated to allow these tissues to increase A polytopic membrane protein cose for their energy needs, the main consumer under their rate of glucose transport by 10–40-fold within that transports sugars down a basal conditions is the brain, which accounts for as minutes of exposure to a particular stimulus (reviewed concentration gradient in an energy-independent manner. much as 80% of whole-body consumption. The energy in REF.1). This system is crucial during exercise, when is provided by the breakdown of endogenous glycogen the metabolic demands of skeletal muscle can increase TYPE II DIABETES stores that are primarily in the liver. These whole-body more than 100-fold, and during the absorptive period Also known as non-insulin- energy stores are replenished from glucose in the diet, (after a meal), to facilitate the rapid insulin-dependent dependent diabetes or maturity onset diabetes. -

Leptin Regulates Glutamate and Glucose Transporters in Hypothalamic Astrocytes
Leptin regulates glutamate and glucose transporters in hypothalamic astrocytes Esther Fuente-Martín, … , Tamas L. Horvath, Julie A. Chowen J Clin Invest. 2012;122(11):3900-3913. https://doi.org/10.1172/JCI64102. Research Article Metabolism Glial cells perform critical functions that alter the metabolism and activity of neurons, and there is increasing interest in their role in appetite and energy balance. Leptin, a key regulator of appetite and metabolism, has previously been reported to influence glial structural proteins and morphology. Here, we demonstrate that metabolic status and leptin also modify astrocyte-specific glutamate and glucose transporters, indicating that metabolic signals influence synaptic efficacy and glucose uptake and, ultimately, neuronal function. We found that basal and glucose-stimulated electrical activity of hypothalamic proopiomelanocortin (POMC) neurons in mice were altered in the offspring of mothers fed a high-fat diet. In adulthood, increased body weight and fasting also altered the expression of glucose and glutamate transporters. These results demonstrate that whole-organism metabolism alters hypothalamic glial cell activity and suggest that these cells play an important role in the pathology of obesity. Find the latest version: https://jci.me/64102/pdf Research article Leptin regulates glutamate and glucose transporters in hypothalamic astrocytes Esther Fuente-Martín,1,2,3 Cristina García-Cáceres,1,2,3 Miriam Granado,1,2,3 María L. de Ceballos,4 Miguel Ángel Sánchez-Garrido,3,5 Beatrix Sarman,6 Zhong-Wu Liu,6 Marcelo O. Dietrich,6 Manuel Tena-Sempere,3,5 Pilar Argente-Arizón,1,2,3 Francisca Díaz,1,3 Jesús Argente,1,2,3 Tamas L. -

Metabolite Transporters As Regulators of Immunity
H OH metabolites OH Review Metabolite Transporters as Regulators of Immunity Hauke J. Weiss * and Stefano Angiari School of Biochemistry and Immunology, Trinity Biomedical Sciences Institute, Trinity College Dublin, Dublin 2, Ireland; [email protected] * Correspondence: [email protected] Received: 4 September 2020; Accepted: 16 October 2020; Published: 19 October 2020 Abstract: In the past decade, the rise of immunometabolism has fundamentally reshaped the face of immunology. As the functions and properties of many (immuno)metabolites have now been well described, their exchange among cells and their environment have only recently sparked the interest of immunologists. While many metabolites bind specific receptors to induce signaling cascades, some are actively exchanged between cells to communicate, or induce metabolic reprograming. In this review, we give an overview about how active metabolite transport impacts immune cell function and shapes immunological responses. We present some examples of how specific transporters feed into metabolic pathways and initiate intracellular signaling events in immune cells. In particular, we focus on the role of metabolite transporters in the activation and effector functions of T cells and macrophages, as prototype adaptive and innate immune cell populations. Keywords: cell metabolism; immunity; metabolite transporter; solute carrier; T cells; macrophages 1. Metabolites and Their Transporters: Key Players in Immunity Active metabolite transport is key for the survival of every cell. In immune cells, availability of extracellular metabolites also shapes immune responses and cellular interactions. Metabolite transporters indeed largely dictate immune cell activity by providing, or restricting, access to nutrients, and thereby determining the cellular metabolic profile [1]. For example, while glucose and amino acids (AAs) are largely imported as part of pro-inflammatory responses, fatty acid (FA) uptake has been found to drive pro-resolving, anti-inflammatory phenotypes [2].