Neuroprotective Functions of Alpinia Galanga in Forebrain Ischemia Induced Neuronal Damage and Oxidative Insults in Rat Hippocampus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jayumedsci-2-2-209.Pdf
Journal of Ayurveda Medical Sciences Refereed, Indexed, Peer reviewed, Open access, Quarterly Journal for Rapid Publication of Ayurveda and Other Traditional Medicine Research ISSN: 2456-4990 www.jayumedsci.com J Ayu Med Sci | 2017 | Vol 2 | Issue 2 (Apr – June) ©Journal of Ayurveda Medical Sciences – HRGS’ Ayurveda Journal Faisal et al. J Ayu Med Sci 2017; 2(2): 209-13 HRGS’ Ayurveda Journal Journal of Ayurveda Medical Sciences Peer Reviewed Journal of Ayurveda and other Traditional Medicines ISSN: 2456-4990|www.jayumedsci.com|[email protected] Short Communication Clinical efficacy of Vrukshamla Beeja Taila (Kokum Butter) in the Management of Padadari (Cracked Heels) Faisal Mohammed1, Sreekant Vishnu Joshi2*, Shridhara Bairy Tantrady3 1Department of Dravyaguna Vignanam, SDM College of Ayurveda and Hospital, Kuthpady, Udupi, 574118. 2School of Ayurvedic Science and Research, Rai Technology University, Bangalore Rural District, Bangalore 561204. 3Department of Dravyaguna Vignanam, SDM College of Ayurveda and Hospital, Kuthpady, Udupi, 574118, India. *Correspondence: Mobile: +91-8792509773; Email: [email protected] ABSTRACT Introduction: Padadari (Cracked heels) is one of the commonly existing podiatric diseases in our society, which is basically caused by the habit of excessive walking that is often associated with excessive dryness leading to the cracking or splitting. Kokum butter oil extracted from the seeds of Vrukshamla (Garcinia indica Choisy.) is used by folklore Vaidyas in Western Ghats of India to treat Padadari, but no study has been documented till date regarding its efficacy in the management of the Padadari. The drug is available easily and used extensively in folk practice. Methods: The Vrukshamla beeja taila (VBT) was prepared by traditional seed-kernel boiling method and then given to 23 patients of Padadari, which were selected from out-patient and in-patient departments of SDM Hospital of Ayurveda, Udupi. -

District Census Handbook, Udupi, Part XII-A & B, Series-30
CENSUS OF INDIA 2001 SERIES - 30 KARNATAKA PART XII - A & B : VILLAGE AND TOWN DIRECTORY & PRIMARY CENSUS ABSTRACT DISTRICT CENSUS HANDBOOK UDUPI DIRECTORATE OF CENSUS OPERATIONS, KARNATAKA,BANGALORE MOT -DMrid Stt~'$ 'Silhrurrull ii:s lkorcm1lJ.orll Ime4llf ~ ;a :sJImlllll w!IniirdIn IImIllre iitt ttlhe 'S!DdIiiestt: ({l)if aIIIl1tlbYe ii'SibmInll'S :amrdl giiwe tt:IDWYII!l «\)jf ttlhe~. lTlt iis uiir.dl ttlbmtt: ~ iitt :l!l 1tJruIle Soo1tltil Sea tOIDD.:oxum:. ~ ttIhm: :l!lllle ~ ;mmH lbmti\rrdl iiJm 11498 «lDll rnre «\)jf ~ iislli2ll1lulls \\\VlInDdIn line ~ sallitiiih :are mUlw gIDll)wwu lhmne.. fie ~ ii'S ~ fM "!Ell P'cadrlOO c&e Saonltat M;anU'_ llit ii'S ifino>m ttlInii'S ttlhalt Ulbrese iitt-s ifamooJrs lI:ro!rs:allit IrtOY.ck$., \\WIIniirdIn Ihmw: ~d iitmnlID D:s_.dl$ ~ 1IlIneiiJr ~ mtme_. TIney;:me jjrumt ;a br tOIDlhm!l!lll1l!'£ cammIl .'SlP'lliitt iilm1nol ~ mIDlMliic.. lP~ ~ JlDlRIDjeatitmm; @ mIDdk lriisiilmg \OOlIl1: @fttlhe ~ ttl1niis ii'S ltlhre (QDD]]Y ~ m1Jim:dtii;a ~ ~ mdks m(j)w «(l)j[ AIr_fum Sea IrIOXllllllrdi <allMxmtt: M;m])p.e.. "'Ulme ~ 1IlIJP> m ~ jp)~ if(jj)~. lflIl):(lQ: iisTharrmll ii'S ~ ;a :sqJ_turmre mmiiIke iilm area DWI lIllM mnrOlfIf: ttlhrm_ 15(0) y.anndk; iiIm wMirdhtlIn.. lIlt Jhm; (()1l):Q00JIlIlt ~ D I s T INDIA KARNATAKA DISTRICT UDUPI Km 5 o 5 [0 [5 Km Ul C.D. Block boundary of Udupi is co-terminus o -with laluk boundary , TOTAL AREA OF DISTRICT (IN SQ.KM) __ _______ __ 38.880.00 ..... -. TOTAL POPULATION OF DISTRICT ____________ __ __ 1.112.243 I TOTAL NUMBER OF TOWNS IN" DISTRICT •••• __ ._ .06 :"- TOTAL NU MBER OF VILLAGES [N DISTRICT _____ . -
Trade Marks Journal No: 1947 , 11/05/2020 Class 5
Trade Marks Journal No: 1947 , 11/05/2020 Class 5 2654104 03/01/2014 SAHUL INDIA LTD MANGALAM-B, 2ND FLOOR, 26, HEMANTA BASU SARANI, KOLKATA - 700 001 MANUFACTURER & MERCHANT AN INDIAN COMPANY Used Since :01/01/1999 To be associated with: 861487 KOLKATA PHARMACEUTICAL PREPARATIONS, AYURVEDIC TEA & HERBAL TEA, AYURVEDIC & HERBAL DRINK, AYURVEDIC & HERBAL MEDICINES, AYURVEDIC PREPARATIONS, VETERINARY AND SANITARY PREPARATIONS, DIETETIC SUBSTANCES ADAPTED FOR MEDICAL USE, FOOD OF BABIES, MATERIALS FOR STOPPING TEETH, DENTAL WAX, DISINFECTANTS, PREPARATION FOR DESTROYING VERMIN, MEDICINAL OILS and COD LIVER OIL INCLUDED IN CLASS- 5. THIS IS SUBJECT TO ASSOCIATION WITH REGISTERED/PENDING REGISTRATION NO.861487.. 321 Trade Marks Journal No: 1947 , 11/05/2020 Class 5 REX'S BALM 2687194 26/02/2014 REX (U&A) REMEDIES PRIVATE LIMITED A-5/11, G.T KARNAL ROAD, INDUSTRIAL AREA, DELHI-110 033 MANUFACTURERS, MERCHANTS AND TRADERS Address for service in India/Attorney address: BMJ LAW PARTNER DLF CAPITAL GREENS, PHASE 1, TOWER C, 233, LEVEL 23, SHIVAJI MARG, MOTI NAGAR, NEW DELHI-110015 Used Since :02/02/1995 To be associated with: 1627591, 1627594, 1947647, 2124412, 2124413, 2124414, 2124418 DELHI UNANI AND AYURVEDIC MEDICINES AND MEDICINAL PREPARATIONS 322 Trade Marks Journal No: 1947 , 11/05/2020 Class 5 2813487 22/09/2014 ORGANIC INDIA PVT.LTD. PLOT NO 266 KAMTA CHINHAT FAIZABAD ROAD LUCKNOW 227105 U.P. MERCHANTS & MANUFACTURERS Address for service in India/Attorney address: LALL & SETHI D - 17, SOUTH EXTENSION PART - II, NEW DELHI - 110 049. Used Since :01/06/2014 To be associated with: 2519579 DELHI “pharmaceutical substances, dietetic substances adapted for medical use, ayurvedic herbal supplements”. -

Report of the Joint Committee Constituted in the O.A. No. 254 Of
REPORT OF THE JOINT COMMITTEE CONSTITUTED BY HON’BLE NGT ( SZ) IN THE OA NO. 254 OF 2020 IN THE MATTER OF SMT SUGANDHI SHEKAR VERSUS UNION OF INDIA RELATING TO ESTABLISHMENT OF FISH MEAL (MILL) AND OIL COMPANY IN COASTAL AREA/RIVER BANKS ALONG THE BANKS OF UDHYAVARA RIVER, UDUPI DISTRICT, KARNATAKA. 1.0. PREAMBLE In the OA No 254 of 2020, filed by Smt Sugandhi Shekar Versus Union of India, the Hon’ble National Green Tribunal (SZ), issued an Order dated 14.12.2020 with the following directions: “ 7. Considering the circumstances, in order to ascertain the real state of affairs and also the alleged violation, we feel it appropriate to appoint a Joint Committee comprising of (1) a Senior Officer from Ministry of Environment, Forests and Climate Change (MoEF&CC), Regional Office, Bangalore (2) a Senior Officer from Central Pollution Control Board (CPCB), Regional Office, Bangalore, (3) a Representative Officer of the Karnataka State Coastal Zone Management Authority (KSCZMA) and (4) a Senior Officer from Karnataka State Pollution Control Board (KSPCB) to inspect the area in question and submit a factual as well as action taken report, if there is any violation found. 8. The committee is directed to ascertain as to whether there was any violation of environmental laws in establishing such units in that area, including Coastal Regulation Zone (CRZ) violation, whether necessary permission have been obtained by them for the purpose of starting the units or continuing the units in that area, whether there is any pollution caused on account of functioning of those units and if there is any violation and environmental damage caused on account of their activities including pollution caused to air as well as water then, the committee is directed to assess the environmental compensation apart from taking action for violation in running the units under the respective statues. -

Antifungal and Antioxidant Activities of Organic and Aqueous Extracts of Annona Squamosa Linn. Leaves
journal of food and drug analysis 23 (2015) 795e802 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.jfda-online.com Original Article Antifungal and antioxidant activities of organic and aqueous extracts of Annona squamosa Linn. leaves * Narasimharaju Kalidindi a, , Nagarasanakote Venkataswamy Thimmaiah b, Nagepally Venkataramareddy Jagadeesh c, Ramaiah Nandeep a, Sathyanarayana Swetha a, Bharat Kalidindi d a Department of Pharmacology, Visveswarapura Institute of Pharmaceutical Sciences, Bangalore, Karnataka, India b Department of Pharmacology, KLE College of Pharmacy, Belgaum, Karnataka, India c Department of Pharmacology, SET's College of Pharmacy, Dharwad, Karnataka, India d SDM College of Ayurveda Kuthpady, Udupi, Karnataka, India article info abstract Article history: An increasing demand for natural additives has shifted the attention from synthetic to Received 2 October 2014 natural antioxidants and antifungal agents. This study was carried out to evaluate the Received in revised form antifungal and antioxidant activities of methanol, chloroform, and aqueous extracts of 16 February 2015 Annona squamosa Linn. leaves. The antifungal activities of all extracts of A. squamosa leaves Accepted 5 May 2015 against five different strains of fungi (Alternaria alternata, Candida albicans, Fusarium solani, Available online 26 July 2015 Microsporum canis, and Aspergillus niger) were evaluated by the agar well diffusion method and the minimum inhibitory concentration of each extract was assessed by antifungal suscep- Keywords: tibility using the broth microdilution method. The antioxidant potential of each extract was acetogenins determined by free radicals (1,1-diphenyl-2-picrylhydrazyl, nitric oxide, and hydrogen Annona peroxide) scavenging activity and reducing power property of A. squamosa leaves. Both antifungal organic and aqueous extracts were found to express dose-dependent inhibition against all antioxidant tested fungi strains in both agar well diffusion and broth dilution methods. -

Exploration and Elucidation of Various Medicinal Plants Used in The
Journal of Pharmacognosy and Phytochemistry 2019; 8(1): 1887-1890 E-ISSN: 2278-4136 P-ISSN: 2349-8234 JPP 2019; 8(1): 1887-1890 Exploration and elucidation of various medicinal Received: 26-11-2018 Accepted: 29-12-2018 plants used in the management of dermatological disorders by folklore practitioners of Udupi Faisal Mohammed Assistant Professor, Department of District, Karnataka, India Dravyaguna, Sri Dharmasthala Manjunatheshwara Ayurveda College and Hospital, Kuthpady, Udupi, Karnataka, India Faisal Mohammed and Shetty P Shifa Shetty P Shifa PG Scholar Department of Abstract Dravyaguna, Sri Dharmasthala Introduction: Ayurveda emphasizes to utilize the flora which is available in and around us for medicinal Manjunatheshwara Ayurveda purpose. It also believes everything is medicinal in nature thus suggests to collect the information about College and Hospital, these local medicinal flora from the Vanavaasi (Primitive tribes), Ajapa (Goatherds), Avipa (Shepherds) Kuthpady, Udupi, Karnataka, and Gopa (Cowherds). Traditionally the science of healing is taught from one generation to another, India which is now kept as a secret. Hence an attempt is made in this direction to collect the information from traditional healers who use locally available plants of their place for skin ailments located in coastal region of Karnataka called Udupi. Methodology: The information regarding the plant species, their local name, part used, mode of usage along with dosage of the medicinal plants used by them. The data was collected by randomly selecting 24 informers who were from 16 different villages and data is collected using a Self-prepared questionnaire based interviews. Results and Conclusion: The ethno-medico-botanical survey is documented and it reveals that 27 different plant species belonging to 16 families which were used by the folklore practitioners to successfully prevent and treat various ailments of skin as well as hair. -

Pharmacognostical and Preliminary Phytochemical Characterization of Tender Leaves of Combretum Latifolium Blume - a Folklore Medicinal Plant
INTERNATIONAL AYURVEDIC MEDICAL JOURNAL Research Article ISSN: 2320 5091 Impact Factor: 5.344 PHARMACOGNOSTICAL AND PRELIMINARY PHYTOCHEMICAL CHARACTERIZATION OF TENDER LEAVES OF COMBRETUM LATIFOLIUM BLUME - A FOLKLORE MEDICINAL PLANT Ravikrishna.S1*, Suchitra. N. Prabhu2 1Associate Professor, Department of Agadatantra, Sri Dharmasthala Manjunatheshwara College of Ayurveda and Hospital, Kuthpady, Udupi, Karnataka, India 2Research officer, Department of Pharmacognosy and Phytochemistry, Sri Dharmasthala Manjunatheshwara Centre for Research in Ayurveda and Allied Sciences, Kuthpady, Udupi, Karnataka, India Corresponding Author: [email protected] https://doi.org/10.46607/iamj0708082020 (Published online: August 2020) Open Access © International Ayurvedic Medical Journal, India 2020 Article Received:17/07/2020 - Peer Reviewed:04/08/2020 - Accepted for Publication:04/08/2020 ABSTRACT Objective: The study is undertaken with the intention to document the pharmacognostic characters in order to ascertain identity, quality and authenticity of the crude drug. Further the Phytochemical class predominantly to which the plant belongs will be of great importance contributing to its biological activity and therapeutic use. The tender leaves of Combretum latifolium(C. latifolium)Blume. are used to render the immune system strong. Com- bretum species are extensively used in traditional medicinal system from inflammation to diuretic. The present study is a step to unleash its phytochemical characterization which may be responsible for its biological activity. Pharmacognostic characters will serve the drugs identity and authentication. Materials and methods: Sample of crude plant material were collected around Udupi area and its identity was thus confirmed by botanist. Macro- microscopic study of the preserved specimen in the fixative was conducted in the department of Pharmacognosy and preliminary phytochemical test and HPTLC fingerprint of the leaf extract was carried out as per testing proto- cols. -

World Journal of Pharmaceutical Research Niyathi Et Al
World Journal of Pharmaceutical Research Niyathi et al. World Journal of Pharmaceutical SJIF ImpactResearch Factor 8.084 Volume 8, Issue 13, 550-561. Review Article ISSN 2277– 7105 PHARMACOGNOSTIC, PHYTOCHEMICAL AND HPTLC PROFILE OF THEV DHANTU [PETIOLE OF COLOCASIA ESCULENTA (LINN.) SCHOTT.] Dr. Niyathi*, 1Dr. Chaithra Hebbar, 2Dr. Suma V. Mallya, 3Dr. Mohammed Faisal and 4Suchitra Narayan Prabhu *PG Scholar, Department of Dravyaguna Vigyana, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Kuthpady, Udupi- 574118, Karnataka, India. 1Professor and Head, Department of Agadatantra, Research Head, Folklore Medicine Research Centre, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Kuthpady, Udupi- 574118, Karnataka, India. 2Associate Professor, Department of Dravyaguna Vigyana, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Kuthpady, Udupi- 574118, Karnataka, India. 3Associate Professor, Department of Dravyaguna Vigyana, Sri Dharmasthala Manjunatheshwara College of Ayurveda & Hospital, Kuthpady, Udupi- 574118, Karnataka, India. 4Research Officer, Department of Pharmaceutical Chemistry and Pharmacognosy, S. D. M. Centre for Research in Ayurveda and Allied Sciences, Kuthpady, Udupi- 574118, Karnataka, India. ABSTRACT Article Received on 02 Oct. 2019, Introduction: Ayurveda always emphasizes on utility of local flora in Revised on 22 Oct. 2019, treatment. It also advices to know about the plant completely with Accepted on 12 Nov. 2019, DOI: 10.20959/wjpr201913-16266 respect to its identity, -

In-Vitro Evaluation of Scoparia Dulcis Linn. for Anti – Urolithiatic Activity
The Journal of Phytopharmacology 2018; 7(3): 285-287 Online at: www.phytopharmajournal.com Research Article In-vitro evaluation of Scoparia dulcis Linn. for anti – ISSN 2320-480X urolithiatic activity JPHYTO 2018; 7(3): 285-287 May- June Hima Sasidharan, Suma Venkatesh Mallya*, Prabhu Suchitra, Koppala Narayana Sunil Kumar Received: 27-02-2018 Accepted: 26-04-2018 ABSTRACT © 2018, All rights reserved Introduction: Urolithiasis is a complex process that occurs from series of several physicochemical event Hima Sasidharan PG Scholar, Shree Dharmasthala including super-saturation, nucleation, growth, aggregation and retention within the kidneys. Data from in- Manjunatheshwara College of vitro, in- vivo and clinical trials reveal that phytotherapeutic agents could be useful as either alternative or an Ayurveda, Kuthpady, Udupi, 574118, adjunct therapy in the management of Urolithiasis. Scoparia dulcis (L.) have been reported to possess Karnataka, India antiurolithiatic property by various folk lore practitioners. Methods: The in- vitro antiurolithiatic study of the Suma Venkatesh Mallya whole plant of S. dulcis (L). through titrimetric and turbidity method to check their potential in dissolving Associate Professor, Shree calcium oxalate crystals using Cystone as the standard compound Result: The aqueous extract showed Dharmasthala Manjunatheshwara relatively higher dissolution of 66.96% of stones than the alcoholic extract. The turbidity showed by the College of Ayurveda, Kuthpady, Udupi, alcohol extract and the aqueous extract of test drug -
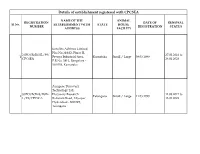
New Institution Registration List.Xlsx
Details of establishment registered with CPCSEA NAME OF THE ANIMAL REGISTRATION DATE OF RENEWAL Sl No. ESTABLISHMENT WITH STATE HOUSE NUMBER REGISTRATION STATUS ADDRESS FACILITY Eurofins Advinus Limited, Plot No.21&22, Phase II, 2/PO/RcBi/SL/99/ 27.02.2018 to 1 Peenya Industrial Area, Karnataka Small / Large 09.03.1999 CPCSEA 26.02.2023 P.B.No. 5813, Bangalore - 560 058, Karnataka Aurigene Discovery Technology Ltd. 3/PO/RcBi-S/RcBi- Discovery Research 14.03.2017 to 2 Telangana Small / Large 11.03.1999 L/99/CPCSEA Bollaram Road, Miyapur 13.03.2022 Hyderabad - 500 049, Telangana INTOX, Institute for Toxicological Studies 6/PO/RcBi/S/99/C 375, Uravade, Pirangut- 31.07.2017 to 3 Maharashtra Small 09.03.1999 PCSEA Uravade Road Tal.Mulshi, 30.07.2022 District-Pune-412 108, Maharashtra National Centre for Cell Sciences (An Autonomous Institution of the 7/GO/ReBi/S/99/C Department of 10.03.2017 to 4 Maharashtra Small 09.03.1999 PCSEA Biotechnology, Government 09.03.2022 of India NCCS Complex, Ganesh Khind, Pune - 411 007, Maharashtra Institute of Nuclear Medicine & Allied Sciences (INMAS) Govt of India, Ministry of Defence, Defence 8/GO/RBi/S/99/CP Research & Development 13.04.2017 to 5 Delhi Small 09.03.1999 CSEA Organisation, Institute of 12.04.2022 Nuclear Medicine & Allied Sciences, Brig. S.K. Mazumdar Road, Delhi – 110 054 Institute of Genomics & Integrative Biology Centre for Biochemical 9/GO/RBiBt/S/99/ Technology 11.04.2017 to 6 Delhi Small 09.03.1999 CPCSEA Council for Scientific & 10.04.2022 Industrial Research Delhi University Campus, Mall Road, Delhi-110 007 All India Institute of Medical 10/GO/ReBiBt/S/99 Sciences 08.09.2017 to 7 Delhi Small 09.03.1999 /CPCSEA (AIIMS), Ansari Nagar 07.09.2022 New Delhi-110 029 Shreya Life Sciences Pvt. -

Karnataka State District Profile 1991
CENSUS OF INDIA 1991 Dr. M. VIJAVANUNNI of the Indian Administrative Service Registrar General & Census Commissioner, India Registrar General of India (In charge of the census of India and vital statistics) Office Address: 2A Mansingh Road New Delhi 110011, India Telephone: (91-11 )338 3761 Fax: (91-11}3383145 Email: [email protected] Internet: http://www.censusindia.net Registrar General of India's publications can be purchased from the following: • The Sales Depot (Phone:338 6583) Office of the Registrar General of India 2-A Mansingh Road New Delhi 110 011, India • Directorates of Census Operations in the capitals of all states and union territories in India • The Controller of Publication Ofd Secretariat Civil Lines Delhi 110054 • Kitab Mahal State ~mporia Complex, Unit No.21 aaba Kharak Singh Marg New Delhi 110001 • Sales outlets of the Controller of Pubtication aU over tndia Census data available on floppy disks can be purchased from the following: • Office of the Registrar General, Jndia Data Processing Division 2nd Floor, 'E' Wing Pushpa Bhawan Madangir Road New Delhi 110062, India Telephone: (91-11)698 1558 Fax: (91-11)6980295 Email: [email protected] © Registrar General of India The contents of this publication may be quoted citing the source dearly PREFACE "To see a world in a grain of sand And a heaven in a wild flower Hold infinity in the palm of your hand And eternity in an hour" Such as described in the above verse would be the graphic outcome of the effort to consolidate the district-level data relating to all the districts of a state or the union territories into a Single tome as is this volume. -

CTRI Trial Data
PDF of Trial CTRI Website URL - http://ctri.nic.in Clinical Trial Details (PDF Generation Date :- Sat, 25 Sep 2021 08:36:33 GMT) CTRI Number CTRI/2016/12/007523 [Registered on: 02/12/2016] - Trial Registered Retrospectively Last Modified On 16/11/2016 Post Graduate Thesis No Type of Trial Interventional Type of Study Drug Ayurveda Study Design Single Arm Trial Public Title of Study Single Blind Clinical Study of Shodhana Karma and an indigenous Drug Combination on Polycystic Ovarian Disease Scientific Title of Single Blind Clinical Study of Shodhana Karma and an indigenous Drug Combination on Polycystic Study Ovarian Disease Secondary IDs if Any Secondary ID Identifier NIL NIL Details of Principal Details of Principal Investigator Investigator or overall Name Dr Mamatha Trial Coordinator (multi-center study) Designation Professor Affiliation SDM College of Ayurveda and Hospital Kuthpady Address Department of Prasuti Tantra and Streeroga SDM College of Ayurveda and Hospital, Kuthpady Udupi District 574118 Karnataka Department of Prasuti Tantra and Streeroga Udupi KARNATAKA 574118 India Phone 08202520332 Fax 08202533970 Email [email protected] Details Contact Details Contact Person (Scientific Query) Person (Scientific Name Dr Mamatha Query) Designation Professor Affiliation SDM College of Ayurveda and Hospital Kuthpady Address Department of Prasuti Tantra and Streeroga SDM College of Ayurveda and Hospital, Kuthpady Udupi District 574118 Karnataka Department of Prasuti Tantra and Streeroga Udupi KARNATAKA 574118 India Phone 08202520332