Cutaneous B-Cell Neoplasms Mimicking Granulomatous Rosacea Or Rhinophyma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Training Available: in 2012, Lorenzo Kunze, M.E
2013 Derma-Lo - offers the 2013 Thermo-Lo - offers the reduction of: sun/age spot, milia, reduction of: sun/age spot, milia, telangiectasia / epidermal spider telangiectasia / epidermal spider veins, cherry hemangiomas, veins, cherry hemangiomas and Thermolysis (AC) and Electrolysis Thermolysis (AC) hair removal. (DC) hair removal. Also: active acne, acne scarring, sebaceous hyperplasia, and skin tags. Training Available: In 2012, Lorenzo Kunze, M.E. Includes: Hydro-Lo - treatment IN DENVER ONCE A MONTH developed Chromos, Inc. - which of fine lines and wrinkles, TRAINING AVAILABLE AT in Greek, can be interpreted as enlarged pore reduction, boosts YOUR LOCATION ASK ABOUT “color” or “light” – in essence, the penetration of product into COST without light we have no color. the skin and tightens loose skin. “Dedicated to Excellence” Also: select your choice of (1 of Continuing to provide a professional & positive attitude in the medical 2) LED’s – both are non invasive and aesthetic field. hand-held light probes: BLUE for CHROMOS, Inc. the treatment of acne or Lorenzo Kunze, M.E. Chromos strives to be a guiding INFRARED to increase collagen [email protected] “light” that assists medical and and elastin, Rosacea, increased www.DermaLo.com aesthetic professionals in finding healing properties, minor muscle www.Thermo-Lo.com and pursuing proper education and moderate joint pain. 888-499-8991 / 303-994-7236 and accurate knowledge. Lorenzo Kunze, M.E. Lorenzo is a true visionary - 40 years in the medical and aesthetic field Medical Electrologist / medical educator 1st non-medical professional to provide electrolysis treatments in an OR Treated over 20,000 patients - last 16 years 1st in the U.S. -

Dermatology DDX Deck, 2Nd Edition 65
63. Herpes simplex (cold sores, fever blisters) PREMALIGNANT AND MALIGNANT NON- 64. Varicella (chicken pox) MELANOMA SKIN TUMORS Dermatology DDX Deck, 2nd Edition 65. Herpes zoster (shingles) 126. Basal cell carcinoma 66. Hand, foot, and mouth disease 127. Actinic keratosis TOPICAL THERAPY 128. Squamous cell carcinoma 1. Basic principles of treatment FUNGAL INFECTIONS 129. Bowen disease 2. Topical corticosteroids 67. Candidiasis (moniliasis) 130. Leukoplakia 68. Candidal balanitis 131. Cutaneous T-cell lymphoma ECZEMA 69. Candidiasis (diaper dermatitis) 132. Paget disease of the breast 3. Acute eczematous inflammation 70. Candidiasis of large skin folds (candidal 133. Extramammary Paget disease 4. Rhus dermatitis (poison ivy, poison oak, intertrigo) 134. Cutaneous metastasis poison sumac) 71. Tinea versicolor 5. Subacute eczematous inflammation 72. Tinea of the nails NEVI AND MALIGNANT MELANOMA 6. Chronic eczematous inflammation 73. Angular cheilitis 135. Nevi, melanocytic nevi, moles 7. Lichen simplex chronicus 74. Cutaneous fungal infections (tinea) 136. Atypical mole syndrome (dysplastic nevus 8. Hand eczema 75. Tinea of the foot syndrome) 9. Asteatotic eczema 76. Tinea of the groin 137. Malignant melanoma, lentigo maligna 10. Chapped, fissured feet 77. Tinea of the body 138. Melanoma mimics 11. Allergic contact dermatitis 78. Tinea of the hand 139. Congenital melanocytic nevi 12. Irritant contact dermatitis 79. Tinea incognito 13. Fingertip eczema 80. Tinea of the scalp VASCULAR TUMORS AND MALFORMATIONS 14. Keratolysis exfoliativa 81. Tinea of the beard 140. Hemangiomas of infancy 15. Nummular eczema 141. Vascular malformations 16. Pompholyx EXANTHEMS AND DRUG REACTIONS 142. Cherry angioma 17. Prurigo nodularis 82. Non-specific viral rash 143. Angiokeratoma 18. Stasis dermatitis 83. -

Fusion of Multiple Heterogeneous Networks for Predicting Circrna
www.nature.com/scientificreports OPEN Fusion of multiple heterogeneous networks for predicting circRNA- disease associations Received: 22 January 2019 Lei Deng1, Wei Zhang1, Yechuan Shi1 & Yongjun Tang2 Accepted: 18 June 2019 Circular RNAs (circRNAs) are a newly identifed type of non-coding RNA (ncRNA) that plays crucial roles Published: xx xx xxxx in many cellular processes and human diseases, and are potential disease biomarkers and therapeutic targets in human diseases. However, experimentally verifed circRNA-disease associations are very rare. Hence, developing an accurate and efcient method to predict the association between circRNA and disease may be benefcial to disease prevention, diagnosis, and treatment. Here, we propose a computational method named KATZCPDA, which is based on the KATZ method and the integrations among circRNAs, proteins, and diseases to predict circRNA-disease associations. KATZCPDA not only verifes existing circRNA-disease associations but also predicts unknown associations. As demonstrated by leave-one-out and 10-fold cross-validation, KATZCPDA achieves AUC values of 0.959 and 0.958, respectively. The performance of KATZCPDA was substantially higher than those of previously developed network-based methods. To further demonstrate the efectiveness of KATZCPDA, we apply KATZCPDA to predict the associated circRNAs of Colorectal cancer, glioma, breast cancer, and Tuberculosis. The results illustrated that the predicted circRNA-disease associations could rank the top 10 of the experimentally verifed associations. Circular RNA (circRNA) is a class of non-coding RNA recently discovered. Unlike linear RNA, circRNA forms a continuous cycle of covalent closures and is highly represented in the eukaryotic transcriptome. Previous research has found thousands of prototype circRNAs in human, mouse and nematode cells1–4. -

Rosacea: an Update
REVIEW JONELLE K. MCDONNELL, MD KENNETH J. TOMECKI, MD Department of Dermatology, Cleveland Clinic Department of Dermatology, Cleveland Clinic Rosacea: An update • ABSTRACT | >1 OSACEA is a chronic and recurrent LAM inflammatory skin disease characterized Rosacea is a common inflammatory skin disease affecting by erythema, papules, pustules, telangiectasia, the central face of adults. Its etiology is unknown. Early and occasionally sebaceous hyperplasia, which diagnosis and appropriate treatment, usually with topical or primarily affects the central face. The disease systemic antibiotics or both, minimizes symptoms and helps evolves in stages and affects middle-aged to prevent complications. adults. Early diagnosis and thoughtful manage- ment help to control the disease and to mini- • KEY POINTS mize the patient's discomfort and emotional distress. Historically, rosacea has been a mis- Rosacea has a spectrum of cutaneous clinical findings: understood disorder, often attributed to alco- facial erythema, papules, pustules, telangiectasia, and holism and acne.1 rhinophyma. • INCIDENCE Common triggers are sunlight, stress, exposure to extreme Rosacea is a common and chronic disease that heat or cold, alcohol, hot beverages, and spicy foods. affects approximately 13 million Americans, or about 1 in 20 people. Because rosacea fre- Rosacea can resemble other diseases, including acne, quently affects people of northern European seborrheic dermatitis, systemic lupus erythematosus, and heritage, it is often called the "curse of the sarcoidosis. Celts."2 In contrast, it is rarely seen in dark- skinned individuals.3 In most patients, the Ocular involvement occurs in more than 50% of patients onset occurs between the ages of 30 and 50. with rosacea. The early stages affect women more often than men at a ratio of 3 to 1, but men more often Oral tetracycline and topical metronidazole are the develop disfiguring rhinophyma. -

Disease Discovery Classification of Lymphoid Neoplasms
From www.bloodjournal.org by on December 4, 2008. For personal use only. 2008 112: 4384-4399 doi:10.1182/blood-2008-07-077982 Classification of lymphoid neoplasms: the microscope as a tool for disease discovery Elaine S. Jaffe, Nancy Lee Harris, Harald Stein and Peter G. Isaacson Updated information and services can be found at: http://bloodjournal.hematologylibrary.org/cgi/content/full/112/12/4384 Articles on similar topics may be found in the following Blood collections: Neoplasia (4200 articles) Free Research Articles (544 articles) ASH 50th Anniversary Reviews (32 articles) Clinical Trials and Observations (2473 articles) Information about reproducing this article in parts or in its entirety may be found online at: http://bloodjournal.hematologylibrary.org/misc/rights.dtl#repub_requests Information about ordering reprints may be found online at: http://bloodjournal.hematologylibrary.org/misc/rights.dtl#reprints Information about subscriptions and ASH membership may be found online at: http://bloodjournal.hematologylibrary.org/subscriptions/index.dtl Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published semimonthly by the American Society of Hematology, 1900 M St, NW, Suite 200, Washington DC 20036. Copyright 2007 by The American Society of Hematology; all rights reserved. From www.bloodjournal.org by on December 4, 2008. For personal use only. ASH 50th anniversary review Classification of lymphoid neoplasms: the microscope as a tool for disease discovery Elaine S. Jaffe,1 Nancy Lee Harris,2 Harald Stein,3 and Peter -
C&P Service Clinician's Guide
C&P Service Clinician’s Guide CLINICIAN’S GUIDE MARCH 2002 1 C&P Service Clinician’s Guide Table of Contents Table of Contents 2 PREFACE 4 Chapter 1 – INTRODUCTION TO COMPENSATION AND PENSION 5 Worksheet – Aid and Attendance or Housebound Examination 16 Worksheet – General Medical Examination 18 Chapter 2 – DISEASES OF THE SKIN INCLUDING SCARS 22 Worksheet – Skin Diseases (Other Than Scars) 28 Worksheet – Scars 29 Chapter 3 – BIRTH DEFECTS IN CHILDREN OF VIETNAM VETERANS 30 SECTION I: Children with spina bifida who are the children of Vietnam veterans 30 SECTION II: Children with birth defects who are the children of women Vietnam veterans 32 Chapter 4 – EYE 34 Worksheet – Eye Examination 39 Chapter 5 – EAR, MOUTH, NOSE AND THROAT 42 Worksheet – Audio 57 Worksheet – Dental and Oral 59 Worksheet – Ear Disease 60 Worksheet – Mouth, Lips and Tongue 62 Worksheet – Nose, Sinus, Larynx, and Pharynx 63 Worksheet – Sense of Smell and Taste 64 Chapter 6 – RESPIRATORY 65 Worksheet – Respiratory (Obstructive, Restrictive, and Interstitial) 71 Worksheet – Respiratory Diseases, Miscellaneous 73 Worksheet – Pulmonary Tuberculosis and Mycobacterial Diseases 75 Chapter 7 – CARDIOVASCULAR SYSTEM 77 Worksheet – Arrhythmias 88 Worksheet – Arteries, Veins, and Miscellaneous 90 Worksheet – Heart 93 Worksheet – Hypertension 95 1 C&P Service Clinician’s Guide Chapter 8 – DISEASES OF THE DIGESTIVE SYSTEM 96 SECTION I: ESOPHAGUS 96 SECTION II: STOMACH 101 SECTION III: INTESTINE 103 SECTION IV: RECTUM AND ANUS 107 SECTION V: ALIMENTARY APPENDAGES 110 Worksheet -

Skin Conditions and Related Need for Medical Care Among Persons 1=74 Years United States, 1971-1974
Data from the Series 11 NATIONAL HEALTH SURVEY Number 212 Skin Conditions and Related Need for Medical Care Among Persons 1=74 Years United States, 1971-1974 DHEW Publication No. (PHS) 79-1660 U.S, DEPARTMENT OF HEALTH, EDUCATION, AND WELFARE Public Health Service Office of the Assistant Secretary for Health National Center for Health Statistics Hyattsville, Md. November 1978 NATIONAL CENTIER FOR HEALTH STATISTICS DOROTHY P. RICE, Director ROBERT A. ISRAEL, Deputy Director JACOB J. FELDAMN, Ph.D., Associate Director for Amdy.sis GAIL F. FISHER, Ph.D., Associate Director for the Cooperative Health Statistics System ELIJAH L. WHITE, Associate Director for Data Systems JAMES T. BAIRD, JR., Ph.D., Associate Director for International Statistics ROBERT C. HUBER, Associate Director for Managewzent MONROE G. SIRKEN, Ph.D., Associate Director for Mathematical Statistics PETER L. HURLEY, Associate Director for Operations JAMES M. ROBEY, Ph.D., Associate Director for Program Development PAUL E. LEAVERTON, Ph.D., Associate Director for Research ALICE HAYWOOD,, Information Officer DIVISION OF HEALTH EXAMINATION STATISTICS MICHAEL A. W. HATTWICK, M.D., Director JEAN ROEERTS, Chiej, Medical Statistics Branch ROBERT S. MURPHY, Chiej Survey Planning and Development Branch DIVISION OF OPERATIONS HENRY MILLER, ChieJ Health -Examination Field Operations Branch COOPERATION OF THE U.S. BUREAU OF THE CENSUS Under the legislation establishing the National Health Survey, the Public Health Service is authorized to use, insofar as possible, the sesw?icesor facilities of other Federal, State, or private agencies. In accordance with specifications established by the National Center for Health Statis- tics, the U.S. Bureau of the Census participated in the design and selection of the sample and carried out the household interview stage of :the data collection and certain parts of the statis- tical processing. -

Pathological Investigation of Rosacea with Particular Regard Of
CORE Metadata, citation and similar papers at core.ac.uk Provided by White Rose E-theses Online A Clinico-Pathological Investigation of Rosacea with Particular Regard to Systemic Diseases Dr. Mustafa Hassan Marai Submitted in accordance with the requirements for the degree of Doctor of Medicine The University of Leeds School of Medicine May 2015 “I can confirm that the work submitted is my own and that appropriate credit has been given where reference has been made to the work of others” “This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement” May 2015 The University of Leeds Dr. Mustafa Hassan Marai “The right of Dr Mustafa Hassan Marai to be identified as Author of this work has been asserted by him in accordance with the Copyright, Designs and Patents Act 1988” Acknowledgement Firstly, I would like to thank all the patients who participate in my rosacea study, giving their time and providing me with all of the important information about their disease. This is helped me to collect all of my study data which resulted in my important outcome of my study. Secondly, I would like to thank my supervisor Dr Mark Goodfield, consultant Dermatologist, for his continuous support and help through out my research study. His flexibility, understanding and his quick response to my enquiries always helped me to relive my stress and give me more strength to solve the difficulties during my research. Also, I would like to thank Dr Elizabeth Hensor, Data Analyst at Leeds Institute of Molecular Medicine, Section of Musculoskeletal Medicine, University of Leeds for her understanding the purpose of my study and her help in analysing my study data. -

Daily Scientific Programme Saturday 15 June, 2019
15 JUNE DAILY SCIENTIFIC PROGRAMME SATURDAY SATURDAY 15 JUNE, 2019 SATURDAY 15 JUNE, 2019 AMBER 1 07:00-08:00 07:00 Cutaneous Lymphomas: therapeutic update Nicola Pimpinelli (ITALY) GRUPPO SIDeMaST ALLERGIE CUTANEE: 07:10 Laser in capillary malformations Acrylates: Old and new allergens IS Francesca Negosanti (ITALY) CO-CHAIRS: Colombina Vincenzi (ITALY), Paolo Pigatto (ITALY) 07:20 Nevi treatments with lasers Davide Brunelli (ITALY) 07:00 Introduction Paolo Pigatto (ITALY) 07:30 Lasers in Rhinophyma Giovanni Cannarozzo (ITALY) 07:05 Contact allergy to electrocardiogram electrodes caused by acrylic acid without sensitivity to 07:40 Lasers in Neurofibromatosis methacrylates and ethyl cyanoacrylate Giuseppe Lodi (ITALY), Mario Sannino (ITALY) Paolo Romita (ITALY), Caterina Foti (ITALY) 07:50 Discussion 07:15 2-HEMA as screening tool in the detection of (Meth) Acrylates allergy: the Italian experience AMBER 5+6 07:00-08:00 Katharina Hansel (GERMANY), Luca Stingeni (ITALY) GRUPPO SIDeMaST DERMATOLOGIA 07:25 Hands contact dermatitis to (Meth) Acrylates in IS CHIRURGICA: Case reports in Dermatologic dental technicians Surgery Antonio Cristaudo (ITALY) CO-CHAIRS: Klaus Eisendle (ITALY), Mario Puviani (ITALY) 07:35 Contact stomatitis to (Meth) Acrylate in odontoiatric patients 07:00 Squamocellular carcinoma in albino africans Paolo Pigatto (ITALY), Gianpaolo Guzzi (ITALY) Massimo Gravante (ITALY) 07:45 Discussion 07:08 Reconstruction of full thickness nasal alar defect in a patient with sebaceous carcinoma Daniele Dusi (ITALY) AMBER 2 07:00-08:00 -
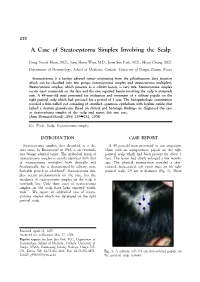
A Case of Steatocystoma Simplex Involving the Scalp
230 A Case of Steatocystoma Simplex Involving the Scalp Dong Nyeok Hyun, M.D., Jong Hoon Won, M.D., Joon Soo Park, M.D., Hyun Chung, M.D. Department of Dermatology, School of Medicine, Catholic University of Daegu, Daegu, Korea Steatocystoma is a benign adnexal tumor originating from the pilosebaceous duct junction which can be classified into two groups (steatocystoma simplex and steatocystoma multiplex). Steatocystoma simplex, which presents as a solitary lesion, is very rare. Steatocystoma simplex occurs most commonly on the face and the case reported herein involving the scalp is extremely rare. A 49-year-old man presented for evaluation and treatment of a solitary papule on the right parietal scalp which had persisted for a period of 1 year. The histopathologic examination revealed a thin-walled cyst consisting of stratified squamous epithelium with hyaline cuticle that lacked a stratum granulosum. Based on clinical and histologic findings, we diagnosed this case as steatocystoma simplex of the scalp and report this rare case. (Ann Dermatol (Seoul) 20(4) 230∼232, 2008) Key Words: Scalp, Steatocystoma simplex INTRODUCTION CASE REPORT Steatocystoma simplex, first described as a dis- A 49-year-old man presented to our outpatient tinct entity by Brownstein1 in 1982, is an extremely clinic with an asymptomatic papule on the right rare benign adnexal tumor. The individual lesion of parietal scalp which had been present for about 1 steatocystoma simplex is usually identical with that year. The lesion had slowly enlarged a few months of steatocystoma multiplex, both clinically and ago. The physical examination revealed a skin- histologically, but is characterized by solitary, non- colored, deep-seated, soft cystic mass on his right heritable growth in adulthood1. -

UC Davis Dermatology Online Journal
UC Davis Dermatology Online Journal Title Penicillamine-associated cutis laxa and milia en plaque - case report and review of cutaneous changes associated with penicillamine Permalink https://escholarship.org/uc/item/47p4d8zv Journal Dermatology Online Journal, 22(5) Authors Vajdi, Tina Lee, Wiggin Wu Paravar, Taraneh Publication Date 2016 DOI 10.5070/D3225030951 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 22 Number 5 May 2016 Photo Vignette Penicillamine-associated cutis laxa and milia en plaque - case report and review of cutaneous changes associated with penicillamine Tina Vajdi1, Wiggin Wu Lee2, Taraneh Paravar2 Dermatology Online Journal 22 (5): 12 1University of California, San Diego School of Medicine 2Department of Dermatology, University of California, San Diego Correspondence: Taraneh Paravar, MD Assistant Clinical Professor Department of Dermatology University of California, San Diego 8899 University Center Lane, Suite 350 San Diego, California 92122, USA Tel. (858) 657-8322 E-mail: [email protected] Abstract Penicillamine-induced skin changes are rare and include: hypersensitivity reactions, autoimmune reactions, and cutaneous elastoses. We report a case of a 73-year-old man with cystinuria taking penicillamine for over 50 years who presented with penicillamine-induced cutis laxa and milia en plaque. A brief review of penicillamine induced skin changes, specifically cutis laxa and milia en plaque, is presented. Key Words: penicillamine, elastic tissue, cystinuria, cutis laxa, milia en plaque Introduction Penicillamine is a chelating agent commonly used to treat cystinuria and Wilson disease. Cystinuria is a genetic disorder in which patients lack the cysteine amino acid transporter. -

A Retrospective Chart Review Examining the Clinical Utility of Family Health History
Sarah Lawrence College DigitalCommons@SarahLawrence The Joan H. Marks Graduate Program in Human Genetics Theses Human Genetics 5-2017 A Retrospective Chart Review Examining the Clinical Utility of Family Health History Katherine Dao Sarah Lawrence College Julia Russo Sarah Lawrence College Follow this and additional works at: https://digitalcommons.slc.edu/genetics_etd Part of the Genetics Commons Recommended Citation Dao, Katherine and Russo, Julia, "A Retrospective Chart Review Examining the Clinical Utility of Family Health History" (2017). Human Genetics Theses. 33. https://digitalcommons.slc.edu/genetics_etd/33 This Thesis - Open Access is brought to you for free and open access by the The Joan H. Marks Graduate Program in Human Genetics at DigitalCommons@SarahLawrence. It has been accepted for inclusion in Human Genetics Theses by an authorized administrator of DigitalCommons@SarahLawrence. For more information, please contact [email protected]. Katherine Dao and Julia Russo A Retrospective Chart Review Examining the Clinical Utility of Family Health History Authors: Katherine Dao, Julia Russo, Jennifer L. Garbarini, Sheila C. Johal, Shannon Wieloch Submitted in partial completion of the Master of Science Degree at Sarah Lawrence College, May 2017 1/34 Katherine Dao and Julia Russo Abstract Family health history (FHH) is a simple and cost-effective clinical tool widely used by genetic professionals. Although the value of FHH for assessing personal and familial health and reproductive risk within a prenatal population has been demonstrated in past studies, its utility within a genetic carrier screening population has not been evaluated. The purpose of this study was to examine the utility of FHH as a clinical screening tool and explore the general outcomes of full FHH evaluations within an expanded carrier screening (ECS) population.