UNDERSTANDING YOUR MULTIPLE MYELOMA LAB TESTS This Lab Tracker Booklet Explains Common Tests for Patients with Multiple Myeloma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lactoferrin and Its Detection Methods: a Review
nutrients Review Lactoferrin and Its Detection Methods: A Review Yingqi Zhang, Chao Lu and Jin Zhang * Department of Chemical and Biochemical Engineering, University of Western Ontario, London, ON N6A 5B9, Canada; [email protected] (Y.Z.); [email protected] (C.L.) * Correspondence: [email protected] Abstract: Lactoferrin (LF) is one of the major functional proteins in maintaining human health due to its antioxidant, antibacterial, antiviral, and anti-inflammatory activities. Abnormal levels of LF in the human body are related to some serious diseases, such as inflammatory bowel disease, Alzheimer’s disease and dry eye disease. Recent studies indicate that LF can be used as a biomarker for diagnosis of these diseases. Many methods have been developed to detect the level of LF. In this review, the biofunctions of LF and its potential to work as a biomarker are introduced. In addition, the current methods of detecting lactoferrin have been presented and discussed. We hope that this review will inspire efforts in the development of new sensing systems for LF detection. Keywords: lactoferrin; biomarkers; immunoassay; instrumental analysis; sensor 1. Introduction Lactoferrin (known as lactotransferrin, LF), with a molecular weight of about 80 kDa, is a functional glycoprotein, which contains about 690 amino acid residues. It was first isolated from bovine milk by Sorensen in 1939 and was first isolated from human milk by Citation: Zhang, Y.; Lu, C.; Zhang, J. Johanson in 1960 [1,2]. The three-dimensional structure of LF has been unveiled by high Lactoferrin and Its Detection resolution X-ray crystallographic analysis, and it consists of two homologous globular lobes Methods: A Review. -
Mcb 407-Immunology and Immunochemistry-Lecture Note
MCB 407-IMMUNOLOGY AND IMMUNOCHEMISTRY-LECTURE NOTE DR. D. A. OJO BRIEF HISTORICAL REVIEW OF IMMUNOLOGY The mechanism by which antibody are formed has been debated for years. It was proposed that the specificity of an antibody molecule was determined both by its amino acid sequence but by the molding of the peptide chain around the antigenic determinant. This theory lost favour when it became apparent that antibody-forming cells were devoid of antigen and that antibody specificity was a function of amino acid sequence. At present, the CLONAL (proposed by Burnete) SELECTION THEORY is widely accepted. It holds that an immunologically responsive cell can respond to only one antigen or a closely related group of antigens and that this property is inherent in the cell before the antigen is encountered. According to the clonal selection theory, each individual is endowed with a very large pool of lymphocytes, each of which is capable of responding to a different antigen. When the antigen enters the body, it selects the lymphocyte which has the best “fit” by virtue of a surface receptor. The antigen binds to this antibody-like receptor, and the cell is stimulated to proliferate and form a clone of cells. Thus, selected cells quickly differentiate into plasma cells and secrete antibody which is specific for the antigen which served as the original selecting agent (or a closely related group of antigens). The History of Blood Transfusion Man’s centuries-long desire to perform blood transfusion as a therapeutic procedure forms the cornerstone of the modern science of immunohematology. At present time, the use of whole blood is a well-accepted and commonly employed measure without which many modern surgical procedures could not be carried out. -

CD40L TNF-Related Factors BAFF, APRIL, and Lymphocytic Leukemia
Published May 16, 2012, doi:10.4049/jimmunol.1102066 The Journal of Immunology Stromal Endothelial Cells Establish a Bidirectional Crosstalk with Chronic Lymphocytic Leukemia Cells through the TNF-Related Factors BAFF, APRIL, and CD40L Montserrat Cols,* Carolina M. Barra,† Bing He,* Irene Puga,† Weifeng Xu,* April Chiu,‡ Wayne Tam,x Daniel M. Knowles,x Stacey R. Dillon,{ John P. Leonard,‖ Richard R. Furman,‖ Kang Chen,* and Andrea Cerutti*,†,# Chronic lymphocytic leukemia (CLL) is a clonal B cell disorder of unknown origin. Accessory signals from the microenvironment are critical for the survival, expansion, and progression of malignant B cells. We found that the CLL stroma included microvascular endothelial cells (MVECs) expressing BAFF and APRIL, two TNF family members related to the T cell-associated B cell-stimulating molecule CD40L. Constitutive release of soluble BAFF and APRIL increased upon engagement of CD40 on MVECs by CD40L aberrantly expressed on CLL cells. In addition to enhancing MVEC expression of CD40, leukemic CD40L induced cleavases that elicited intracellular processing of pro-BAFF and pro-APRIL proteins in MVECs. The resulting soluble BAFF and APRIL proteins delivered survival, activation, Ig gene remodeling, and differentiation signals by stimulating CLL cells through TACI, BAFF-R, and BCMA receptors. BAFF and APRIL further amplified CLL cell survival by upregulating the expression of leukemic CD40L. Inhibition of TACI, BCMA, and BAFF-R expression on CLL cells; abrogation of CD40 expression in MVECs; or suppression of BAFF and APRIL cleavases in MVECs reduced the survival and diversification of malignant B cells. These data indicate that BAFF, APRIL, and CD40L form a CLL-enhancing bidirectional signaling network linking neoplastic B cells with the microvascular stroma. -

Immunoglobulin G Is a Platelet Alpha Granule-Secreted Protein
Immunoglobulin G is a platelet alpha granule-secreted protein. J N George, … , L K Knieriem, D F Bainton J Clin Invest. 1985;76(5):2020-2025. https://doi.org/10.1172/JCI112203. Research Article It has been known for 27 yr that blood platelets contain IgG, yet its subcellular location and significance have never been clearly determined. In these studies, the location of IgG within human platelets was investigated by immunocytochemical techniques and by the response of platelet IgG to agents that cause platelet secretion. Using frozen thin-sections of platelets and an immunogold probe, IgG was located within the alpha-granules. Thrombin stimulation caused parallel secretion of platelet IgG and two known alpha-granule proteins, platelet factor 4 and beta-thromboglobulin, beginning at 0.02 U/ml and reaching 100% at 0.5 U/ml. Thrombin-induced secretion of all three proteins was inhibited by prostaglandin E1 and dibutyryl-cyclic AMP. Calcium ionophore A23187 also caused parallel secretion of all three proteins, whereas ADP caused virtually no secretion of any of the three. From these data and a review of the literature, we hypothesize that plasma IgG is taken up by megakaryocytes and delivered to the alpha-granules, where it is stored for later secretion by mature platelets. Find the latest version: https://jci.me/112203/pdf Rapid Publication Immunoglobulin G Is a Platelet Alpha Granule-secreted Protein James N. George, Sherry Saucerman, Shirley P. Levine, and Linda K. Knieriem Division ofHematology, Department ofMedicine, University of Texas Health Science Center, and Audie L. Murphy Veterans Hospital, San Antonio, Texas 78284 Dorothy F. -

RANKL As a Novel EMT Marker 858 Cell Research (2008) 18:858-870
npg RANKL as a novel EMT marker 858 Cell Research (2008) 18:858-870. npg © 2008 IBCB, SIBS, CAS All rights reserved 1001-0602/08 $ 30.00 ORIGINAL ARTICLE www.nature.com/cr Receptor activator of NF-κB Ligand (RANKL) expression is associated with epithelial to mesenchymal transition in human prostate cancer cells Valerie A Odero-Marah1, Ruoxiang Wang1, Gina Chu1, Majd Zayzafoon2, Jianchun Xu1, Chunmeng Shi1, Fray F Marshall1, Haiyen E Zhau1, Leland WK Chung1 1Molecular Urology and Therapeutics Program, Department of Urology and Winship Cancer Institute, Emory University School of Medicine, 1365B Clifton Road, NE, Atlanta, GA 30322, USA; 2Department of Pathology, University of Alabamn, Birmingham, AL 35294, USA Epithelial-mesenchymal transition (EMT) in cancer describes the phenotypic and behavioral changes of cancer cells from indolent to virulent forms with increased migratory, invasive and metastatic potential. EMT can be induced by soluble proteins like transforming growth factor β1 (TGFβ1) and transcription factors including Snail and Slug. We uti- lized the ARCaPE/ARCaPM prostate cancer progression model and LNCaP clones stably overexpressing Snail to identify novel markers associated with EMT. Compared to ARCaPE cells, the highly tumorigenic mesenchymal ARCaPM and ARCaPM1 variant cells displayed a higher incidence of bone metastasis after intracardiac administration in SCID mice. ARCaPM and ARCaPM1 expressed mesenchymal stromal markers of vimentin and N-cadherin in addition to elevated levels of Receptor Activator of NF-κB Ligand (RANKL). We observed that both epidermal growth factor (EGF) plus TGFβ1 treatment and Snail overexpression induced EMT in ARCaPE and LNCaP cells, and EMT was associated with increased expression of RANKL protein. -

What Are Immunoglobulins? by Michelle Greer, RN
CLINICAL BRIEF What Are Immunoglobulins? By Michelle Greer, RN THE IMMUNE SYSTEM is a complex the body such as bacteria or a virus, or in antigen, it gives rise to many large cells network of cells, tissues and organs that cases of transplant, another person’s known as plasma cells. Every plasma cell protect the body from bacteria, virus, organ, tissue or cells. Antigens are identi - is essentially a factory for producing an fungi and other foreign organisms. The fied by the immune system by a marker antibody. 1 Antibodies are also known as primary functions of the immune system molecule, which enables the immune immunoglobulins. Antibodies, or immuno- are to recognize self (the body’s own system to differentiate self from nonself. globulins, are glycoproteins made up of healthy cells) from nonself (anything Lymphocytes (natural killer cells, T cells light chains and heavy chains shaped like foreign), keep self healthy and destroy and B cells) are one of the subtypes of a Y (Figure 1). The different areas on and eliminate nonself. Immunoglobulins white blood cells in the immune system. these chains have different functions and take the lead in this process. B cells secrete antibodies that attach to roles in an immune response. antigens to mark them for destruction. A Review of Terminology Antibodies are antigen-specific, meaning Types of Immunoglobulins Understanding a few related terms and one antibody works against a specific There are several types of immunoglob - their function can provide a better appre - type of bacteria, virus or other foreign ulins and each has a different role in an ciation of immunoglobulins and how substance. -
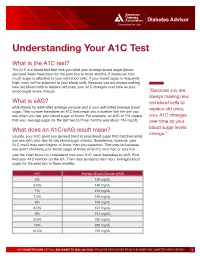
Understanding Your A1C Test
Diabetes Advisor Understanding Your A1C Test What is the A1C test? The A1C is a blood test that tells you what your average blood sugar (blood glucose) levels have been for the past two to three months. It measures how much sugar is attached to your red blood cells. If your blood sugar is frequently high, more will be attached to your blood cells. Because you are always making new red blood cells to replace old ones, your A1C changes over time as your blood sugar levels change. “Because you are always making new What is eAG? red blood cells to eAG stands for estimated average glucose and is your estimated average blood replace old ones, sugar. This number translates an A1C test result into a number like the one you see when you test your blood sugar at home. For example, an A1C of 7% means your A1C changes that your average sugar for the last two to three months was about 154 mg/dL. over time as your What does an A1C/eAG result mean? blood sugar levels change.” Usually, your A1C gives you general trend in your blood sugar that matches what you see with your day-to-day blood sugar checks. Sometimes, however, your A1C result may seem higher or lower than you expected. That may be because you aren’t checking your blood sugar at times when it’s very high or very low. Use the chart below to understand how your A1C result translates to eAG. First find your A1C number on the left. -

Allergens Immunoglobulin E (Ige) Antibodies
Allergens − Immunoglobulin E (IgE) Antibodies Single Allergen IgE Antibody This test is principally useful to confirm the allergen specificity in patients with clinically documented allergic disease. Therefore, requests for these tests should be made after a careful and comprehensive medical history is taken. Utilized in this manner, a single allergen immunoglobulin E (IgE) antibody test is cost-effective. A positive result may indicate that allergic signs and symptoms are caused by exposure to the specific allergen. Multi-allergen IgE Antibodies Profile Tests A number of related allergens are grouped together for ordering convenience. Each is tested individually and reported. Sample volume requirements are the same as if the tests were ordered individually. Panel Tests A pooled allergen reagent is used for each panel; therefore, the panel is reported with a single qualitative class result and concentration. The multi-allergen IgE antibody panel, combined with measurement of IgE in serum, is an appropriate first-order test for allergic disease. Positive results indicate the possibility of allergic disease induced by one or more allergens present in the multi-allergen panel. Negative results may rule out allergy, except in rare cases of allergic disease induced by exposure to a single allergen. Panel testing requires less specimen volume and less cost for ruling out allergic response; however, individual (single) allergen responses cannot be identified. In cases of a positive panel test, follow-up testing must be performed to differentiate between individual allergens in the panel. Note: Only 1 result is generated for each panel. Panels may be ordered with or without concurrent measurement of total IgE. -

Spontaneous Reversal of Acquired Autoimmune Dysfibrinogenemia Probably Due to an Antiidiotypic Antibody Directed to an Interspec
Spontaneous reversal of acquired autoimmune dysfibrinogenemia probably due to an antiidiotypic antibody directed to an interspecies cross-reactive idiotype expressed on antifibrinogen antibodies. A Ruiz-Arguelles J Clin Invest. 1988;82(3):958-963. https://doi.org/10.1172/JCI113704. Research Article A young man with a long history of abnormal bleeding was seen in January 1985. Coagulation tests showed dysfibrinogenemia and an antifibrinogen autoantibody was demonstrable in his serum. This antibody, when purified, was capable of inhibiting the polymerization of normal fibrin monomers, apparently through binding to the alpha fibrinogen chain. 6 mo later the patient was asymptomatic, coagulation tests were normal, and the antifibrinogen autoantibody was barely detectable. At this time, affinity-purified autologous and rabbit antifibrinogen antibodies were capable of absorbing an IgG kappa antibody from the patient's serum, which reacted indistinctly with both autologous and xenogeneic antifibrinogen antibodies in enzyme immunoassays. It has been concluded that the patient's dysfibrinogenemia was the result of an antifibrinogen autoantibody, and that later on an anti-idiotype antibody, which binds an interspecies cross- reactive idiotype expressed on anti-human fibrinogen antibodies, inhibited the production of the antifibrinogen autoantibody which led to the remission of the disorder. Find the latest version: https://jci.me/113704/pdf Spontaneous Reversal of Acquired Autoimmune Dysfibrinogenemia Probably Due to an Antildiotypic Antibody Directed to an Interspecies Cross-reactive Idiotype Expressed on Antifibrinogen Antibodies Alejandro Ruiz-Arguelles Department ofImmunology, Laboratorios Clinicos de Puebla, Puebla, Puebla 72530, Mexico Abstract disorder. This anti-Id antibody was shown to react with xeno- geneic antifibrinogen antibodies, hence, its specificity is an A young man with a long history of abnormal bleeding was interspecies cross-reactive Id (IdX)' most likely encoded by seen in January 1985. -

Serological (Antibody) Testing for Covid-19
SEROLOGICAL (ANTIBODY) TESTING FOR COVID-19 Serological tests detect antibodies in the blood People in the early stages of COVID-19 might generated as part of the immune response test antibody negative despite being highly to a specific infection, such as infection with infectious. Additionally, some tests might give a SARS-CoV-2, the virus that causes COVID-19. false positive result because of past or present Antibody tests are different from tests such as infection with other types of coronaviruses. polymerase chain reaction (PCR) and antigen False positive results are also more likely tests which detect the SARS-CoV-2 virus. when the percentage of the population with Many new serological tests for COVID-19 have the disease is low. The Idaho Division of Public been developed and have an emergency use Health discourages persons who have a positive authorization (EUA) from the U.S. Food and serology test from relaxing the precautions such Drug Administration (FDA). Only antibody tests as social distancing that are recommended for that have an FDA EUA should be used. The all Idahoans to prevent spread of coronavirus, Idaho Division of Public Health discourages and strongly discourages employers form the use of unauthorized serology-based assays relaxing the employee protections for an for diagnosis of COVID-19 or determining if employee solely based upon a positive serology someone is currently infected or had a prior test. infection. The immune response to SARS-CoV-2 (the Serological tests are not recommended for virus that causes COVID-19) infection is not COVID-19 diagnosis in most situations because well understood. -

Guidelines for Writing Examination Items (Questions)
Guidelines for Writing Examination Items (Questions) Enclosed are the content outlines for the Immunology certification examinations. The content outline specifies the breakdown of content and overall structure of the examination and indicates how many test questions are assigned to each topic area from a total of 70 questions. The content outline will guide you in creating new items to match certain topic areas. We would appreciate at least two (2) new items for each major roman numeral on the content outline(s). This means we are asking you to write two items for Roman numeral I, two items for Roman numeral II, and so on for each of the Roman numeral sections of the Content Outline. We would appreciate items submitted in advance, preferably no later than Tuesday, February 25, 2020. • Please use the “Item Writing Template” to create your new items. This is the proper format to be used for all items you submit. Font: Times New Roma. Font Size: 11 • Please identify the Content Outline position for each item (e.g., Chemistry Content Outline, Roman numeral I. “Proteins”, A. “Total Proteins” should be noted as “I.A.”). • New items must be multiple choice with four (4) possible answers. Remember to avoid "double negatives," "not" questions (e.g., "Which of the following is NOT true?"), and those allowing "all (or none) of the above," or "a and b" as a possible answer. • Each new item that you create must be accompanied with a reference [Author, Publication Year, Title, Edition, Page Number(s)] containing the correct answer. IMPORTANT: references must be from an AAB Review Manual, Governmental Regulations, Association or World Health Organization (WHO) Guidelines, or a text or manual published within the last six (6) years. -

Monoclonal Antibody Playbook
Federal Response to COVID-19: Monoclonal Antibody Clinical Implementation Guide Outpatient administration guide for healthcare providers 2 SEPTEMBER 2021 1 Introduction to COVID-19 Monoclonal Antibody Therapy 2 Overview of Emergency Use Authorizations 3 Site and Patient Logistics Site preparation Patient pathways to monoclonal administration 4 Team Roles and Responsibilities Leadership Administrative Clinical Table of 5 Monoclonal Antibody Indications and Administration Indications Contents Preparation Administration Response to adverse events 6 Supplies and Resources Infrastructure Administrative Patient Intake Administration 7 Examples: Sites of Administration and Staffing Patterns 8 Additional Resources 1 1. Introduction to Monoclonal Therapy 2 As of 08/13/21 Summary of COVID-19 Therapeutics 1 • No Illness . Health, no infections • Exposed Asymptomatic Infected . Scope of this Implementation Guide . Not hospitalized, no limitations . Monoclonal Antibodies for post-exposure prophylaxis (Casirivimab + Imdevimab (RGN)) – EUA Issued. • Early Symptomatic . Scope of this Implementation Guide . Not hospitalized, with limitations . Monoclonal Antibodies for treatment (EUA issued): Bamlanivimab + Etesevimab1 (Lilly) Casirivimab + Imdevimab (RGN) Sotrovimab (GSK/Vir) • Hospital Adminission. Treated with Remdesivir (FDA Approved) or Tocilizumab (EUA Issued) . Hospitalized, no acute medical problems . Hospitalized, not on oxygen . Hospitlaized, on oxygen • ICU Admission . Hospitalized, high flow oxygen, non-invasive ventilation