IDEXX Urine Sediment Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Basic Skills in Interpreting Laboratory Data
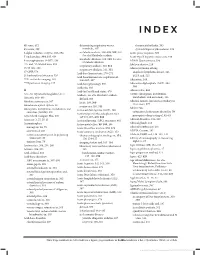
INDEX 4K score, 612 determining respiratory versus rheumatoid arthritis, 505 4Ts score, 399 metabolic, 307 systemic lupus erythematosus, 509 5-alpha reductase enzyme, 593–594 metabolic acidosis, 308–309, 309, 310. Acute phase response, 500 See also Metabolic acidosis 5' nucleotidase, 334, 335, 636 Acute type B hepatitis (minicase), 349 metabolic alkalosis, 309, 310. See also 6-mercaptopurine (6-MP), 138 ADAM Questionnaire, 596 Metabolic alkalosis 13C- and 14C-labeled urea, 353 Addison disease, 219 respiratory acidosis, 310, 311 15/15 rule, 208 Adenocarcinoma of lung respiratory alkalosis, 311, 311 17-OHP, 578 anaplastic lymphoma kinase, 526 Acid-base homeostasis, 270–271 21-hydroxylase deficiency, 526 EGFR and, 525 Acid-base homeostasis, regulation of, 99m Tc-sestamibi imaging, 165 306–307, 307 Adenosine, 164 201 TI perfusion imaging, 165 Acid-base physiology, 306 Adenosine diphosphate (ADP), 394, Acidemia, 303 394 A Acid-fast bacilli and stains, 470 Adenoviridae, 456 A1c. See Glycated hemoglobin (A1c) Acidosis. See also Metabolic acidosis ADME (absorption, distribution, metabolism, and excretion), 136 Abacavir, 468–469 defined, 303 Adnexal tumors, hirsutism secondary to Absolute neutropenia, 387 lactic, 308, 309 (minicase), 577 Absorbance optical system, 28 respiratory, 310, 311 Adolescents Absorption, distribution, metabolism, and Activated clotting time (ACT), 408 excretion (ADME), 136 categories of substances abused by, 70 Activated partial thromboplastin time prerequisite drug testing of, 82–83 Accu Check Compact Plus, 200 (aPTT), -

Bilirubin (Urine) Interpretive Summary
Bilirubin (Urine) Interpretive Summary Description: Bilirubinuria is an indicator of conjugated bilirubin in the urine. Excessive bilirubinuria in a dog or any bilirubinuria in a cat is an indication to evaluate serum bilirubin concentrations. Decreased Bilirubin Common Causes Normal Artifact o Exposure to UV light or room air o Delayed analysis o Centrifugation of urine prior to analysis o Ascorbic acid (Vitamin C) Increased Bilirubin Common Causes Normal dogs (especially males with concentrated urine) Liver disease, bile duct obstruction RBC destruction (hemolysis) o Immune-mediated hemolytic anemia o Zinc or onion toxicity o RBC parasites Uncommon Causes Hemoglobinuria Fever Prolonged anorexia False positive reactions due to medications o Phenothiazines (e.g., chlorpromazine) o Etodolac Related Findings Liver disease, biliary obstruction o Increased serum bilirubin, ALT, ALP, GGT, AST o Increased serum bile acids o Decreased albumin, cholesterol, BUN and glucose in severe cases o Abnormalities in liver and/or biliary tract on abdominal ultrasound RBC destruction o Decreased hematocrit, RBC, hemoglobin o Increased reticulocytes, increased MCV and decreased MCHC, polychromasia o Increased serum bilirubin o Spherocytosis (in dogs), autoagglutination o Hemoglobinuria o Positive Coombs or saline agglutination test may or may not be present with IMHA Generated by VetConnect® PLUS: Bilirubin (Urine) Page 1 of 2 Additional Information Physiology Conjugated bilirubin passes freely through the glomerular filtration barrier and is excreted in urine. Unconjugated bilirubin is bound to albumin and does not normally pass through the glomerular filtration barrier. Therefore, it is not detectable in urine (unless albuminuria or glomerular disease is present). Bilirubinuria usually precedes hyperbilirubinemia and icterus Dogs: Clinically normal dogs (especially males) may have detectable bilirubinuria in concentrated urine due to a low renal threshold for bilirubin. -

Leukocyte Esterase Activity in Vaginal Fluid of Pregnant and Non-Pregnant Women with Vaginitis/Vaginosis and in Controls
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Infect Dis Obstet Gynecol 2003;11:19–26 Leukocyte esterase activity in vaginal fluid of pregnant and non-pregnant women with vaginitis/vaginosis and in controls Per-Anders Mårdh 1, Natalia Novikova 1, Ola Niklasson 1, Zoltan Bekassy 1 and Lennart Skude 2 1Department of Obstetrics and Gynecology, University Hospital, Lund and 2Department of Clinical Chemistry, County Hospital, Halmstad, Sweden Objectives: Todeterminethe leukocyteesterase (LE) activity invaginal lavage fluid ofwomen with acuteand recurrentvulvovaginal candidosis (VVC and RVVC respectively), bacterial vaginosis(BV), and in pregnant and non-pregnantwomen without evidenceof the threeconditions. Also tocompare the resultof LEtestsin women consultingat differentweeks inthe cycle andtrimesters of pregnancy.The LEactivity was correlatedto vaginal pH, numberof inflammatory cells instained vaginal smears,type of predominatingvaginal bacteria andpresence of yeast morphotypes. Methods: Onehundred and thirteen women with ahistoryof RVVC,i.e. with at least fourattacks of the conditionduring the previousyear and who had consultedwith anassumed new attack ofthe condition,were studied.Furthermore, we studied16 women with VVC,15 women with BV,and 27 women attendingfor control of cytological abnormalities, who all presentedwithout evidenceof either vaginitisor vaginosis. Finally, 73 pregnantwomen wereinvestigated. The LEactivity invaginal fluid duringdifferent weeks inthe cycle of 53 of the women was measured. Results: Inthe non-pregnantwomen, anincreased LE activity was foundin 96, 88, 73 and56% of those with RVVC,VVC and BV andin the non-VVC/BVcases,respectively. In 73% of pregnantwomen inthe second trimester,and 76% of thosein the third,the LEtestwas positive.In all groupsof non-pregnantwomen tested, the LEactivity correlatedwith the numberof leukocytesin vaginal smears,but it didnot in those who were pregnant.There was nocorrelation between LE activity andweek incycle. -

Proteinuria and Bilirubinuria As Potential Risk Indicators of Acute Kidney Injury During Running in Outpatient Settings
medicina Article Proteinuria and Bilirubinuria as Potential Risk Indicators of Acute Kidney Injury during Running in Outpatient Settings Daniel Rojas-Valverde 1,2,* , Guillermo Olcina 2,* , Braulio Sánchez-Ureña 3 , José Pino-Ortega 4 , Ismael Martínez-Guardado 2 and Rafael Timón 2,* 1 Centro de Investigación y Diagnóstico en Salud y Deporte (CIDISAD), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia 86-3000, Costa Rica 2 Grupo en Avances en el Entrenamiento Deportivo y Acondicionamiento Físico (GAEDAF), Facultad Ciencias del Deporte, Universidad de Extremadura, 10005 Cáceres, Spain; [email protected] 3 Programa Ciencias del Ejercicio y la Salud (PROCESA), Escuela Ciencias del Movimiento Humano y Calidad de Vida (CIEMHCAVI), Universidad Nacional, Heredia 86-3000, Costa Rica; [email protected] 4 Departmento de Actividad Física y Deporte, Facultad Ciencias del Deporte, 30720 Murcia, Spain; [email protected] * Correspondence: [email protected] (D.R.-V.); [email protected] (G.O.); [email protected] (R.T.); Tel.: +506-8825-0219 (D.R.-V.) Received: 2 September 2020; Accepted: 19 October 2020; Published: 27 October 2020 Abstract: Background and objectives: The purpose of this study was to explore which urinary markers could indicate acute kidney injury (AKI) during prolonged trail running in outpatient settings. Materials and Methods: Twenty-nine experienced trail runners (age 39.1 8.8 years, weight 71.9 11 kg, ± ± height 171.9 8.3 cm) completed a 35 km event (cumulative positive ascend of 1815 m, altitude = 906 to ± 1178 m.a.s.l.) under a temperature of 25.52 1.98 C and humidity of 79.25 7.45%). -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

Ileal Neobladder: an Important Cause of Non-Anion Gap Metabolic Acidosis
The Journal of Emergency Medicine, Vol. 52, No. 5, pp. e179–e182, 2017 Ó 2017 Elsevier Inc. All rights reserved. 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2016.12.036 Clinical Communications: Adult ILEAL NEOBLADDER: AN IMPORTANT CAUSE OF NON-ANION GAP METABOLIC ACIDOSIS Jesse W. St. Clair, MD and Matthew L. Wong, MD, MPH Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts and Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts Reprint Address: Matthew L. Wong, MD, MPH, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Rosenberg Building, 2nd Floor, 1 Deaconess Road, Boston, MA 02446 , Abstract—Background: The differential diagnosis for a disease, or medications such as acetazolamide. non-anion gap metabolic acidosis is probably less well Commonly used mnemonics to remember the differential known than the differential diagnosis for an anion gap for the non-anion gap metabolic acidosis include metabolic acidosis. One etiology of a non-anion gap acidosis ‘‘ABCD’’ for ‘‘Addison’s, Bicarbonate loss, Chloride is the consequence of ileal neobladder urinary diversion (administration), and Drugs,’’ as well as ‘‘HARDUP’’ for the treatment of bladder cancer. Case Report: We pre- for ‘‘Hyperchloremia, Acetazolamide and Addison’s, sent a case of a patient with an ileal neobladder with a severe non-anion gap metabolic acidosis caused by a Renal Tubular Acidosis, Diarrhea, Ureteroenterostomies, urinary tract infection and ureteroenterostomy. Why and Pancreaticoenterostomies’’ (Table 1) (1). Should an Emergency Physician Be Aware of This?: Part Ureteroenterostomies are when the ureter has an of the ileal neobladder surgery includes ureteroenteros- abnormal connection with a segment of intestine. -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening
Kobe J. Med. Sci., Vol. 56, No. 4, pp. E165-E172, 2010 A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening NATSUKO MAKIHARA1, MINEO YAMASAKI1,2, HIROKI MORITA1, and HIDETO YAMADA1* 1Division of Obstetrics and Gynecology, Department of Surgery-related, and 2Division of Integrated Medical Education, Department of Community Medicine and Social Healthcare Science, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan. Received 12 July 2010/ Accepted 20 August 2010 Key Words: dipstick test, pregnancy proteinuria, protein/creatinine ratio, urine specific gravity Proteinuria screening using a semi-quantitative dipstick test of the spot urine in antenatal clinic is known to have high false-positive rates. The aim of this study was to assess availability of a dipstick test combined with the urine specific gravity for the determination of pathological proteinuria. A dipstick test was performed on 582 urine samples obtained from 283 pregnant women comprising 260 with normal blood pressure and 23 with pregnancy-induced hypertension. The urine protein (P) and creatinine (C) concentrations, specific gravity (SG), P/C ratio were determined, and compared with dipstick test results. The P concentration increased along the stepwise augmentations in dipstick test result. Frequencies of the urine samples with 0.265 or more P/C ratio were 0.7% with − dipstick test result, 0.7% with the ± result, 3.3% with the 1+ result, and 88.9% with the ≥2+ result. However, if the urine specific gravity was low, frequencies of the high P/C ratio were 5.0% with ± dipstick test result and 9.3% with the 1+ result. -

Biochemical Profiling of Renal Diseases
INTRODUCTION TO LABORATORY PROFILING Alan H. Rebar, DVM, Ph.D., Diplomate ACVP Purdue University, Discovery Park 610 Purdue Mall, West Lafayette, IN 47907-2040 Biochemical profiling may be defined as the use of multiple blood chemistry determinations to assess the health status of various organ systems simultaneously. Biochemical profiling rapidly has become a major diagnostic aid for the practicing veterinarian for several reasons. First, a more educated clientele has come to expect increased diagnostic sophistication. Secondly, the advent of high-volume clinical pathology laboratories has resulted in low prices that make profiling in veterinary practice feasible and convenient. In addition, improved technology has resulted in the development of procedures that can be used to obtain accurate analyses on microsamples of serum. Such procedures offer obvious advantages to veterinarians, who in the past were hindered by requirements for large sample size. Although biochemical profiling offers exciting potential, it is not a panacea. Since standard chemical screens provide 12 to 30 test results, interpretation of data may be extremely complex. Interpretation is often clouded by the fact that perfectly normal animals may have, indeed, are expected to have, an occasional abnormal test result. It is estimated that in a panel of 12 chemistry tests, approximately 46% of all normal subjects will have at least one abnormal test result. Such abnormalities do not reflect inaccuracies in laboratory test procedures but rather the way in which reference (or normal) values are determined. In order to establish the "normal range" for a given test, the procedure is performed on samples from a large population of clinically normal individuals. -

Specific Gravity, Urine
Lab Dept: Urine/Stool Test Name: SPECIFIC GRAVITY, URINE General Information Lab Order Codes: USG Synonyms: N/A CPT Codes: 81003 – Urinalysis; automated, without microscopy Test Includes: Specific gravity measurement by colorimetric reagent strip. Logistics Test Indications: Useful for evaluating the concentrating and excretory power of the kidney. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 2 - 4 hours Special Instructions: Indicate method of collection on request form (catheterized, clean- catch, or void). Deliver to lab within 30 minutes of collection. Refrigerate specimen if there is a delay in transport of 30 minutes or more. Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire urine collection Processed Volume: Minimum volume: 1 mL Collection: Collect a clean-catch urine specimen as follows: Males: Clean glans with soap and water. Rinse area with wet gauze pads. While holding foreskin retracted, begin voiding. After several mL’s have passed, collect midstream portion without stopping flow of urine. Place the cap on the cup and tighten securely. Refrigerate specimen after collection and promptly forward to the lab. Females: Thoroughly clean urethral area with soap and water. Rinse area with wet gauze pads. While holding labia apart, begin voiding. After several mL’s have passed, collect midstream portion without stopping the flow of urine. Place the cap on the cup and tighten securely. Refrigerate specimen after collection and promptly forward to the lab. Note: Indicate type of specimen (catheterized or void) and time of collection on the label. Special Processing: N/A Patient Preparation: See above Sample Rejection: Less than 1 mL urine; mislabeled or unlabeled specimens Interpretive Reference Range: Age: Specific Gravity: Infant (0 days - 1 year): 1.002 - 1.006 >1 year: 1.001 - 1.030 Critical Values: N/A Limitations: Radiographic dyes in urine increase the specific gravity by hydrometer or refractometer. -

Evaluation of Gross and Microscopic Hematuria
EVALUATION OF GROSS AND MICROSCOPIC HEMATURIA APRIL GARDNER, MSBS, PA - C ASSOCIATE PROGRAM DIRECTOR THE UNIVERSITY OF TOLEDO PA PROGRAM OBJECTIVES • Define the terms gross hematuria and microscopic hematuria. • Identify etiologies of hematuria. • Identify risk factors for a urologic cancer in a patient with gross or microscopic hematuria. • Define the term “full evaluation.” • Identify indications for a full evaluation. • Identify labs and diagnostics to evaluate hematuria. • Identify the appropriate follow-up for patients with hematuria. 2 CASE #1 Ms. T is a healthy 50 year-old female, s/p TAH/BSO 15 years ago for severe endometriosis. She presents today for her annual physical exam required by her employer. She has no new complaints and there is no history of any urologic complaints. Physical exam is completely normal Urine dipstick shows 1+ blood, pH 6.0, negative for ketones, glucose, nitrites and leukocyte esterase Microscopic evaluation shows 8 RBCs, no WBCs, bacteria, yeast, crystals, or casts CASE #1 • Should you prescribe an antibiotic for Ms. T today? • Does she need any further follow-up? • If yes, what would follow-up include? CASE #2 Mr. D is a 38 year-old healthy, monogamous married male with 4 children, presenting for a vasectomy consultation. He denies any complaints, including urologic complaints. He takes no medications. He tells you he ran a marathon 2 days ago and then finished building a deck in his backyard yesterday. Physical exam is completely normal Urine dipstick shows 1+ blood, pH 6.0, negative for protein, ketones, glucose, nitrites and leukocyte esterase Microscopic evaluation shows 3 RBCs, no WBCs, bacteria, yeast, crystals, or casts CASE #2 • Should you prescribe an antibiotic for Mr. -

Storm in a Pee Cup: Hematuria and Proteinuria
Storm in a Pee Cup: Hematuria and Proteinuria Sudha Garimella MD Pediatric Nephrology, Children's Hospital-Upstate Greenville SC Conflict of Interest • I have no financial conflict of interest to disclose concerning this presentation. Objectives • Interpret the current guidelines for screening urinalysis, and when to obtain a urinalysis in the pediatric office. • Interpret the evaluation of asymptomatic/isolated proteinuria and definitions of abnormal ranges. • Explain the evaluation and differential diagnosis of microscopic hematuria. • Explain the evaluation and differential diagnosis of gross hematuria. • Explain and discuss appropriate referral patterns for hematuria. • Racial disparities in nephrology care 1. APOL-1 gene preponderance in African Americans and risk of proteinuria /progression(FSGS) 2. Race based GFR calculations which have caused harm 3. ACEI/ARB usage in AA populations: myths and reality Nephrology Problems in the Office • Hypertension • Proteinuria • Microscopic Hematuria • Abnormal Renal function The Screening Urinalysis • Choosing Wisely: • Don’t order routine screening urine analyses (UA) in healthy, asymptomatic pediatric patients as part of routine well child care. • One study showed that the calculated false positive/transient abnormality rate approaches 84%. • Population that deserves screening UA: • patients who are at high risk for chronic kidney disease (CKD), including but not necessarily limited to patients with a personal history of CKD, acute kidney injury (AKI), congenital anomalies of the urinary tract, acute nephritis, hypertension (HTN), active systemic disease, prematurity, intrauterine growth retardation, or a family history of genetic renal disease. • https://www.choosingwisely.org/societies/american-academy-of-pediatrics-section-on- nephrology-and-the-american-society-of-pediatric-nephrology/ Screening Urinalysis: Components A positive test for leukocyte esterase may be seen in genitourinary inflammation, irritation from instrumentation or catheterization, glomerulonephritis, UTIs and sexually transmitted infections.