Diabetic Ketoacidosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Ketones, Urine
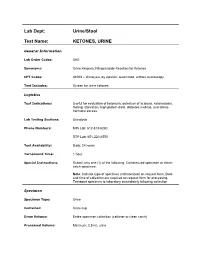
Lab Dept: Urine/Stool Test Name: KETONES, URINE General Information Lab Order Codes: UKE Synonyms: Urine Ketones; Nitroprusside Reaction for Ketones CPT Codes: 81003 – Urinalysis, by dipstick; automated, without microscopy Test Includes: Screen for urine ketones. Logistics Test Indications: Useful for evaluation of ketonuria, detection of acidosis, ketoacidosis, fasting, starvation, high protein diets, diabetes mellitus, and stress- hormone excess. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 hour Special Instructions: Submit only one (1) of the following: Catheterized specimen or clean- catch specimen. Note: Indicate type of specimen (catheterized) on request form. Date and time of collection are required on request form for processing. Transport specimen to laboratory immediately following collection Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire specimen collection (catheter or clean catch) Processed Volume: Minimum: 0.5 mL urine Collection: A specimen collected by catheterization is optimal; however, a clean- catch or mid-stream specimen is also acceptable. Random, voided specimens will be accepted, but are the least desirable and are not recommended if a urine culture is also being requested. Special Processing: N/A Patient Preparation: None Sample Rejection: Less than 0.5 mL urine submitted; mislabeled or unlabeled specimen Interpretive Reference Range: Negative Critical Values: N/A Limitations: Specimens containing -

Diabetic Ketoacidosis and Hyperosmolar BMJ: First Published As 10.1136/Bmj.L1114 on 29 May 2019
STATE OF THE ART REVIEW Diabetic ketoacidosis and hyperosmolar BMJ: first published as 10.1136/bmj.l1114 on 29 May 2019. Downloaded from hyperglycemic syndrome: review of acute decompensated diabetes in adult patients Esra Karslioglu French,1 Amy C Donihi,2 Mary T Korytkowski1 1Division of Endocrinology and Metabolism, Department of ABSTRACT Medicine, University of Pittsburgh, Pittsburgh, PA, USA Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome (HHS) are life threatening 2University of Pittsburgh School of complications that occur in patients with diabetes. In addition to timely identification of the Pharmacy, Pittsburgh, PA, USA Correspondence to: M Korytkowski precipitating cause, the first step in acute management of these disorders includes aggressive [email protected] administration of intravenous fluids with appropriate replacement of electrolytes (primarily Cite this as: BMJ 2019;365:l1114 doi: 10.1136/bmj.l1114 potassium). In patients with diabetic ketoacidosis, this is always followed by administration Series explanation: State of the of insulin, usually via an intravenous insulin infusion that is continued until resolution of Art Reviews are commissioned on the basis of their relevance to ketonemia, but potentially via the subcutaneous route in mild cases. Careful monitoring academics and specialists in the US and internationally. For this reason by experienced physicians is needed during treatment for diabetic ketoacidosis and HHS. they are written predominantly by Common pitfalls in management include premature termination of intravenous insulin US authors therapy and insufficient timing or dosing of subcutaneous insulin before discontinuation of intravenous insulin. This review covers recommendations for acute management of diabetic ketoacidosis and HHS, the complications associated with these disorders, and methods for http://www.bmj.com/ preventing recurrence. -

Glossary of Common Diabetes Terms
Glossary of Common Diabetes Terms A1C: a test that reveals exactly how well your blood sugar (glucose) has been controlled over the previous three months Beta cells: cells found in the pancreas that make insulin Blood glucose: also known as blood sugar, glucose comes from food and is then carried through the blood to deliver energy to cells Blood glucose meter: a small medical device used to check blood glucose levels Blood glucose monitoring: the simple blood test used to check the amount of glucose in the blood; a tiny drop of blood, taken by pricking a finger, is placed on a test strip and inserted in the meter for reading Diabetes: the shortened name for diabetes mellitus, the condition in which the pancreas doesn’t produce enough insulin or your body is unable to use insulin to move glucose into cells of the body Diabetic retinopathy: the eye disease that occurs in someone with diabetes when the small blood vessels of the retina become swollen and leak liquid into the retina, blurring vision; it can sometimes lead to blindness Gestational diabetes: the diabetes some women develop during pregnancy; it typically subsides after the baby is delivered, but many women who have had gestational diabetes may develop type 2 diabetes later in life Glucagon: the hormone that is injected into a person with diabetes to raise their blood glucose level when it’s very low (hypoglycemia) Glucose: blood sugar that gives energy to cells Hyperglycemia: also known as high blood glucose, this condition occurs when your blood glucose level is too high; -

Different Response of Body Weight Change According to Ketonuria After Fasting in the Healthy Obese
ORIGINAL ARTICLE Endocrinology, Nutrition & Metabolism http://dx.doi.org/10.3346/jkms.2012.27.3.250 • J Korean Med Sci 2012; 27: 250-254 Different Response of Body Weight Change According to Ketonuria after Fasting in the Healthy Obese Hyeon-Jeong Kim1, Nam-Seok Joo1, The relationship between obesity and ketonuria is not well-established. We conducted a Kwang-Min Kim1, Duck-Joo Lee1, retrospective observational study to evaluate whether their body weight reduction response and Sang-Man Kim2 differed by the presence of ketonuria after fasting in the healthy obese. We used the data of 42 subjects, who had medical records of initial urinalysis at routine health check-up and 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon; follow-up urinalysis in the out-patient clinic, one week later. All subjects in the initial 2Department of Family Medicine, CHA Biomedical urinalysis showed no ketonuria. However, according to the follow-up urinalysis after three Center, CHA University College of Medicine, Seoul, subsequent meals fasts, the patients were divided into a non-ketonuria group and Korea ketonuria group. We compared the data of conventional low-calorie diet programs for ± Received: 20 August 2011 3 months for both groups. Significantly greater reduction of body weight (-8.6 3.6 kg vs 2 2 Accepted: 17 January 2012 -1.1 ± 2.2 kg, P < 0.001), body mass index (-3.16 ± 1.25 kg/m vs -0.43 ± 0.86 kg/m , P < 0.001) and waist circumference (-6.92 ± 1.22 vs -2.32 ± 1.01, P < 0.001) was Address for Correspondence: observed in the ketonuria group compared to the non-ketonuria group. -

Deficient Diabetic Mice
Diminished Loss of Proteoglycans and Lack of Albuminuria in Protein Kinase C-␣–Deficient Diabetic Mice Jan Menne,1,2 Joon-Keun Park,2 Martin Boehne,2 Marlies Elger,2 Carsten Lindschau,2 Torsten Kirsch,2 Matthias Meier,2 Faikah Gueler,2 Annette Fiebeler,3 Ferdinand H. Bahlmann,2 Michael Leitges,4 and Hermann Haller2 Activation of protein kinase C (PKC) isoforms has been implicated in the pathogenesis of diabetic nephropathy. We showed earlier that PKC-␣ is activated in the kid- iabetes affects Ͼ300 million people worldwide; -neys of hyperglycemic animals. We now used PKC-␣؊/؊ 20–40% will develop overt nephropathy. Diabe mice to test the hypothesis that this PKC isoform tes is the most common cause of end-stage mediates streptozotocin-induced diabetic nephropathy. Drenal disease. The earliest clinical sign of ne- We observed that renal and glomerular hypertrophy was phropathy is microalbuminuria. Microalbuminuria also ؊ ؊ similar in diabetic wild-type and PKC-␣ / mice. How- heralds impending cardiovascular morbidity and mortality ever, the development of albuminuria was almost absent (1–4). Microalbuminuria predicts overt proteinuria, which ؊/؊␣ in the diabetic PKC- mice. The hyperglycemia-in- is now believed to actively promote renal insufficiency (5). duced downregulation of the negatively charged base- Therefore, successful treatment of diabetic patients ment membrane heparan sulfate proteoglycan perlecan -؊ ؊ should aim for the prevention or regression of albumin was completely prevented in the PKC-␣ / mice, com- pared with controls. We then asked whether transform- uria. Hyperglycemia seems to cause microalbuminuria in   diabetic patients (6,7). However, how the metabolic dis- ing growth factor- 1 (TGF- 1) and/or vascular endothelial growth factor (VEGF) is implicated in the turbance causes cellular effects is incompletely under- PKC-␣–mediated changes in the basement membrane. -

Kv-Ada-Jdbc210013 1..3
Diabetes Care Volume 44, June 2021 e1 Performance of the Insulin-Only Luz E. Castellanos,1 Courtney A. Balliro,1 Jordan S. Sherwood,1 Rabab Jafri,1 iLet Bionic Pancreas and the Mallory A. Hillard,1 Evelyn Greaux,1 Rajendranath Selagamsetty,2 Hui Zheng,3 Bihormonal iLet Using Firas H. El-Khatib,2 Edward R. Damiano,2,4 and Dasiglucagon in Adults With Type Steven J. Russell1 1 Diabetes in a Home-Use Setting Diabetes Care 2021;44:e1–e3 | https://doi.org/10.2337/DC20-1086 Reductions in blood glucose levels in with insulin lispro (Eli Lilly) or aspart (Table 1). The mean CGM glucose and people with diabetes are often (Novo Nordisk), the bihormonal iLet for time in range (70–180 mg/dL) were 149 achieved at the expense of increased 7 days with dasiglucagon (4 mg/mL) ±13mg/dLand72±8%,respectively,in hypoglycemia. A novel approach is to and insulin lispro or aspart, or both, us- the insulin-only period, and 139 ± 11 automatically deliver microdose gluca- ing the same glucose target (110 mg/ mg/dL and 79 ± 9%, respectively, in the gon when automation of insulin deliv- dL), in random order. There were no re- bihormonal period. The mean daily car- ery alone is not sufficient to prevent strictions on diet or exercise. The prima- bohydrates consumed to prevent or hypoglycemia. The approach requires a ry outcomes were prespecified iLet treat hypoglycemia were 16 ± 13 g and bihormonal device and a stable form of operational thresholds. The key second- 18 ± 21 g in the insulin-only and bihor- glucagon or glucagon analog. -

Acute Renal Failure in Patients with Type 1 Diabetes Mellitus G
Postgrad Med J: first published as 10.1136/pgmj.70.821.192 on 1 March 1994. Downloaded from Postgrad Med J (1994) 70, 192- 194 C) The Fellowship of Postgraduate Medicine, 1994 Acute renal failure in patients with type 1 diabetes mellitus G. Woodrow, A.M. Brownjohn and J.H. Turney Renal Unit, Leeds General Infirmary, Great George Street, Leeds LSJ 3EX, UK Summary: Acute renal failure (ARF) is a serious condition which still carries a mortality of around 50%. People with diabetes may be at increased risk of developing ARF, either as a complication of diabetic ketoacidosis or hyperosmolar coma, increased incidence of cardiovascular disease, or due to increased susceptibility ofthe kidney to adverse effects in the presence ofunderlying diabetic renal disease. During the period 1956-1992, 1,661 cases of ARF have been treated at Leeds General Infirmary. Of these, we have identified 26 patients also having type 1 diabetes. ARF due to diabetic ketoacidosis is surprisingly uncommon (14 cases out of 23 patients whose notes were reviewed). All cases of ARF complicating ketoacidosis in the last decade have been associated with particularly severe illness requiring intensive care unit support, rather than otherwise 'uncomplicated' ketoacidosis. We discuss the conditions that may result in ARF in patients with diabetes and the particular difficulties that may be encountered in management. Introduction People with diabetes may be at increased risk of Results developing acute renal failure (ARF). Acute pre- copyright. renal failure may occur as a result ofthe severe fluid Of 23 patients with type 1 diabetes complicated by depletion associated with diabetic ketoacidosis and ARF, diabetic ketoacidosis was the main underly- non-ketotic hyperosmolar coma. -

Ideal Conditions for Urine Sample Handling, and Potential in Vitro Artifacts Associated with Urine Storage
Urinalysis Made Easy: The Complete Urinalysis with Images from a Fully Automated Analyzer A. Rick Alleman, DVM, PhD, DABVP, DACVP Lighthouse Veterinary Consultants, LLC Gainesville, FL Ideal conditions for urine sample handling, and potential in vitro artifacts associated with urine storage 1) Potential artifacts associated with refrigeration: a) In vitro crystal formation (especially, calcium oxalate dihydrate) that increases with the duration of storage i) When clinically significant crystalluria is suspected, it is best to confirm the finding with a freshly collected urine sample that has not been refrigerated and which is analyzed within 60 minutes of collection b) A cold urine sample may inhibit enzymatic reactions in the dipstick (e.g. glucose), leading to falsely decreased results. c) The specific gravity of cold urine may be falsely increased, because cold urine is denser than room temperature urine. 2) Potential artifacts associated with prolonged storage at room temperature, and their effects: a) Bacterial overgrowth can cause: i) Increased urine turbidity ii) Altered pH (1) Increased pH, if urease-producing bacteria are present (2) Decreased pH, if bacteria use glucose to form acidic metabolites iii) Decreased concentration of chemicals that may be metabolized by bacteria (e.g. glucose, ketones) iv) Increased number of bacteria in urine sediment v) Altered urine culture results b) Increased urine pH, which may occur due to loss of carbon dioxide or bacterial overgrowth, can cause: i) False positive dipstick protein reaction ii) Degeneration of cells and casts iii) Alter the type and amount of crystals present 3) Other potential artifacts: a) Evaporative loss of volatile substances (e.g. -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening
Kobe J. Med. Sci., Vol. 56, No. 4, pp. E165-E172, 2010 A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening NATSUKO MAKIHARA1, MINEO YAMASAKI1,2, HIROKI MORITA1, and HIDETO YAMADA1* 1Division of Obstetrics and Gynecology, Department of Surgery-related, and 2Division of Integrated Medical Education, Department of Community Medicine and Social Healthcare Science, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan. Received 12 July 2010/ Accepted 20 August 2010 Key Words: dipstick test, pregnancy proteinuria, protein/creatinine ratio, urine specific gravity Proteinuria screening using a semi-quantitative dipstick test of the spot urine in antenatal clinic is known to have high false-positive rates. The aim of this study was to assess availability of a dipstick test combined with the urine specific gravity for the determination of pathological proteinuria. A dipstick test was performed on 582 urine samples obtained from 283 pregnant women comprising 260 with normal blood pressure and 23 with pregnancy-induced hypertension. The urine protein (P) and creatinine (C) concentrations, specific gravity (SG), P/C ratio were determined, and compared with dipstick test results. The P concentration increased along the stepwise augmentations in dipstick test result. Frequencies of the urine samples with 0.265 or more P/C ratio were 0.7% with − dipstick test result, 0.7% with the ± result, 3.3% with the 1+ result, and 88.9% with the ≥2+ result. However, if the urine specific gravity was low, frequencies of the high P/C ratio were 5.0% with ± dipstick test result and 9.3% with the 1+ result. -

KETON.Zemia and KETONURIA in CHILDHOOD. by MURIEL J
Arch Dis Child: first published as 10.1136/adc.1.5.302 on 1 January 1926. Downloaded from KETON.zEMIA AND KETONURIA IN CHILDHOOD. BY MURIEL J. BROWN, M.B., Ch.B., D.P.H., AND GRACE GRAHAMI, AM.D. From the Medical Department, The Royal Hospital for Sick Children, Glasgow. The formation of ketone bodies and their excretion in the urine in albnormall amounts have for many years been problems of much interest to both physiologist and clinician. Much of our present knowledge of the subject has been gained from the study of carbohydrate metabolism in diabetes, where ketonuria in its classical formi is frequently observed. From this it has been established that an excess of ketone bodies occurs in the blood when the fats are incompletely ' combusted ' as a result of abnormal carbohydrate metabolism, and ample justification has been provided for the well-known sta.tement myiade by Rosenfeld(l) in 1895 ' that fat burns only in the fire of carbohydrate.' A good review of our present knowledge of ketone production and its prevention is to be found in Shaffer's recent lecture entitled ' Antiketo- genesis, its Mechanism and Signifiecance. '(2) A fu-ll discussion of the stubject in all its aspects is not within the scope of the present communication, but we may quote that ' there no Shaffer's statement is to-day question that http://adc.bmj.com/ ketosis is due to carbohydrate starvation,' and make special reference also to his remninder that the inhibitory effect of carbohydrate on ketone formation depends, not on the mnere existence of sufficient glucose, as glucose, in the blood (cf. -

End-Stage Renal Disease Increases Rates of Adverse Glucose Events When Treating Diabetic Ketoacidosis Or Hyperosmolar Hyperglycemic State Caitlin M
Clinical Diabetes Papers in Press, published online May 3, 2017 End-Stage Renal Disease Increases Rates of Adverse Glucose Events When Treating Diabetic Ketoacidosis or Hyperosmolar Hyperglycemic State Caitlin M. Schaapveld-Davis,1 Ana L. Negrete,1,2 Joanna Q. Hudson,1–3 Jagannath Saikumar,3 Christopher K. Finch,1,2 Mehmet Kocak,4 Pan Hu,4 and Megan A. Van Berkel,1,2 FEATURE ARTICLE FEATURE ■ IN BRIEF Treatment guidelines for diabetic emergencies are well described in patients with normal to moderately impaired kidney function. However, management of patients with end-stage renal disease (ESRD) is an ongoing challenge. This article describes a retrospective study comparing the rates of adverse glucose events (defined as hypoglycemia or a decrease in glucose >200 mg/dL/hour) between patients with ESRD and those with normal kidney function who were admitted with diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS). These results indicate that current treatment approaches to DKA or HHS in patients with ESRD are suboptimal and require further evaluation. anagement strategies for dia- den, characterized by an exchange of betic ketoacidosis (DKA) and the intracellular potassium ion pool Mhyperosmolar hyperglycemic for the newly increased extracellular state (HHS) are well established in hydrogen ion concentration (1–3). patients with normal kidney function. In contrast, patients with ESRD and Therapy typically includes aggressive DKA or HHS are routinely observed fluid resuscitation, electrolyte replace- to have hyperkalemia resulting from ment, insulin administration, and a combination of transcellular shifts treatment of the precipitating cause and a lack of renal clearance, thus (if identified). However, treatment eliminating the need for electrolyte strategies for these key principles replacement (4).