Transketolase Counteracts Oxidative Stress to Drive Cancer Development
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oxidative Pentose Phosphate Pathway Enzyme 6-Phosphogluconate Dehydrogenase Plays a Key Role in Breast Cancer Metabolism
biology Article Oxidative Pentose Phosphate Pathway Enzyme 6-Phosphogluconate Dehydrogenase Plays a Key Role in Breast Cancer Metabolism Ibrahim H. Polat 1,2,3 ,Míriam Tarrado-Castellarnau 1,4 , Rohit Bharat 1, Jordi Perarnau 1 , Adrian Benito 1,5 , Roldán Cortés 1, Philippe Sabatier 2 and Marta Cascante 1,4,* 1 Department of Biochemistry and Molecular Biomedicine and Institute of Biomedicine (IBUB), Faculty of Biology, Universitat de Barcelona, Av Diagonal 643, 08028 Barcelona, Spain; [email protected] (I.H.P.); [email protected] (M.T.-C.); [email protected] (R.B.); [email protected] (J.P.); [email protected] (A.B.); [email protected] (R.C.) 2 Equipe Environnement et Prédiction de la Santé des Populations, Laboratoire TIMC (UMR 5525), CHU de Grenoble, Université Grenoble Alpes, 38700 CEDEX La Tronche, France; [email protected] 3 Department of Medicine, Hematology/Oncology, Goethe-University Frankfurt, 60590 Frankfurt, Germany 4 Centro de Investigación Biomédica en Red de Enfermedades Hepáticas y Digestivas (CIBEREHD), Instituto de Salud Carlos III (ISCIII), 28001 Madrid, Spain 5 Division of Cancer, Department of Surgery and Cancer, Faculty of Medicine, Imperial College London, London W12 0NN, UK * Correspondence: [email protected] Simple Summary: Cancer cells alter their metabolism to maintain their high need for energy, produce Citation: Polat, I.H.; enough macromolecules for biosynthesis, and preserve their redox status. The investigation of Tarrado-Castellarnau, M.; Bharat, R.; cancer cell-specific metabolic alterations has vital importance to identify targets to be exploited for Perarnau, J.; Benito, A.; Cortés, R.; therapeutic development. The pentose phosphate pathway (PPP) is often highly activated in tumor Sabatier, P.; Cascante, M. -

Enzyme Characterisation and Kinetic Modelling of the Pentose Phosphate
1 Enzyme characterisation and kinetic modelling of the pentose 2 phosphate pathway in yeast 1;2 3 Hanan L. Messiha Edward Kent 1;3;4 Naglis Malys 1;2;6 Kathleen M. Carroll 1;5 Neil Swainston 1;4 s 1;4;7;∗ t Pedro Mendes 1;4 n Kieran Smallbone i r P 1Manchester Centre for Integrative Systems Biology e r 2Faculty of Life Sciences 3 P Doctoral Training Centre in Integrative Systems Biology 4School of Computer Science 5School of Chemistry University of Manchester, M13 9PL, UK. 6School of Life Sciences, Gibbet Hill Campus, University of Warwick, Coventry, UK. 7Center for Quantitative Medicine and Department of Cell Biology, University of Connecticut Health Center, 263 Farmington Avenue, Farmington, CT 06030, USA. 4 Abstract 5 We present the quantification and kinetic characterisation of the enzymes of the pentose 6 phosphate pathway in Saccharomyces cerevisiae. The data are combined into a mathematical 7 model that describes the dynamics of this system and allows us to predict changes in metabo- 8 lite concentrations and fluxes in response to perturbations. We use the model to study the 9 response of yeast to a glucose pulse. We then combine the model with an existing glycolysis 10 model to study the effect of oxidative stress on carbohydrate metabolism. The combina- 11 tion of these two models was made possible by the standardised enzyme kinetic experiments 12 carried out in both studies. This work demonstrates the feasibility of constructing larger 13 network-scale models by merging smaller pathway-scale models. ∗To whom correspondence should be addressed at [email protected] PeerJ PrePrints | http://dx.doi.org/10.7287/peerj.preprints.146v4 | CC-BY 3.0 Open Access | received: 10 Apr 2014, published: 10 Apr 2014 1 14 Introduction 15 The pentose phosphate pathway (PPP) is a central and widely conserved metabolic pathway of car- 16 bohydrate metabolism which, in eukaryotic cells, is located in the cytoplasm (see Figure 1). -

Lecture 7 - the Calvin Cycle and the Pentose Phosphate Pathway
Lecture 7 - The Calvin Cycle and the Pentose Phosphate Pathway Chem 454: Regulatory Mechanisms in Biochemistry University of Wisconsin-Eau Claire 1 Introduction The Calvin cycle Text The dark reactions of photosynthesis in green plants Reduces carbon from CO2 to hexose (C6H12O6) Requires ATP for free energy and NADPH as a reducing agent. 2 2 Introduction NADH versus Text NADPH 3 3 Introduction The Pentose Phosphate Pathway Used in all organisms Glucose is oxidized and decarboxylated to produce reduced NADPH Used for the synthesis and degradation of pentoses Shares reactions with the Calvin cycle 4 4 1. The Calvin Cycle Source of carbon is CO2 Text Takes place in the stroma of the chloroplasts Comprises three stages Fixation of CO2 by ribulose 1,5-bisphosphate to form two 3-phosphoglycerate molecules Reduction of 3-phosphoglycerate to produce hexose sugars Regeneration of ribulose 1,5-bisphosphate 5 5 1. Calvin Cycle Three stages 6 6 1.1 Stage I: Fixation Incorporation of CO2 into 3-phosphoglycerate 7 7 1.1 Stage I: Fixation Rubisco: Ribulose 1,5- bisphosphate carboxylase/ oxygenase 8 8 1.1 Stage I: Fixation Active site contains a divalent metal ion 9 9 1.2 Rubisco Oxygenase Activity Rubisco also catalyzes a wasteful oxygenase reaction: 10 10 1.3 State II: Formation of Hexoses Reactions similar to those of gluconeogenesis But they take place in the chloroplasts And use NADPH instead of NADH 11 11 1.3 State III: Regeneration of Ribulose 1,5-Bisphosphosphate Involves a sequence of transketolase and aldolase reactions. 12 12 1.3 State III: -

The Pentose Phosphate Pathway and Its Involvement in Cisplatin Resistance
International Journal of Molecular Sciences Review The Pentose Phosphate Pathway and Its Involvement in Cisplatin Resistance Isabella Giacomini 1, Eugenio Ragazzi 1 , Gianfranco Pasut 2 and Monica Montopoli 1,3,* 1 Department of Pharmaceutical and Pharmacological Sciences, University of Padua, Largo Egidio Meneghetti 2, 35131 Padova, Italy; [email protected] (I.G.); [email protected] (E.R.) 2 Department of Pharmaceutical and Pharmacological Sciences, University of Padua, Via Marzolo 5, 35131 Padova, Italy; [email protected] 3 Veneto Institute of Molecular Medicine, Via Giuseppe Orus 2, 35129 Padova, Italy * Correspondence: [email protected]; Tel.: +39-049-827-5090 Received: 30 December 2019; Accepted: 29 January 2020; Published: 31 January 2020 Abstract: Cisplatin is the first-line treatment for different types of solid tumors, such as ovarian, testicular, bladder, cervical, head and neck, lung, and esophageal cancers. The main problem related to its clinical use is the onset of drug resistance. In the last decades, among the studied molecular mechanisms of cisplatin resistance, metabolic reprogramming has emerged as a possible one. This review focuses on the pentose phosphate pathway (PPP) playing a pivotal role in maintaining the high cell proliferation rate and representing an advantage for cancer cells. In particular, the oxidative branch of PPP plays a role in oxidative stress and seems to be involved in cisplatin resistance. In light of these considerations, it has been demonstrated that overexpression and higher enzymatic activity of different enzymes of both oxidative and non-oxidative branches (such as glucose-6-phosphate dehydrogenase, 6-phosphogluconate dehydrogenase, and transketolase) increase cisplatin resistance, and their silencing or combined treatment with cisplatin could restore cisplatin sensitivity. -

RESPIRATION Pentose Phosphate Pathway Or Hexose Monophosphate Pathway
RESPIRATION Pentose Phosphate Pathway or Hexose Monophosphate Pathway Pentose phosphate pathway or hexose monophosphate pathway (HMP pathway) is the other common pathway to break down glucose to pyruvate and operates in both aerobic and anaerobic conditions. This pathway produces NADPH, which carries chemical energy in the form of reducing power and is used almost universally as the reductant in anabolic (energy utilization) pathways (e.g., fatty acid biosynthesis, cholesterol biosynthesis, nucleotide biosynthesis) and detoxification pathways (e.g., reduction of oxidized glutathione, cytochrome P450 monooxygenases). Also, the pentose phosphate pathway generates pentose sugar ribose and its derivatives, which are necessary for the biosynthesis of nucleic acids (DNA and RNA) as well as ATP, NADH, FAD, and coenzyme A. In this way, though the pentose phosphate pathway may be a source of energy in many microorganisms, it is more often of greater importance in various biosynthetic pathways. Pentose phosphate pathway consists of two phases: the oxidative phase and the non-oxidative phase. Oxidative Phase: The oxidative phase of the pentose phosphate pathway initiates with the conversion of glucose 6- phosphate to 6-Phosphogluconate. NADP+ is the electron acceptor yielding NADPH during this reaction. 6-Phosphogluconate, a six-carbon sugar, is then oxidativelydecarboxylated to yield ribulose 5-phosphate, a five-carbon sugar. NADP+ is again the electron acceptor yielding NADPH. In the final step of oxidative phase, there is isomerisation of ribulose 5-phosphatc to ribose 5- phosphate by phosphopentose isomerase and the conversion of ribulose 5-phosphate into its epimerxylulose 5-phosphate by phosphopentose epimerase for the transketolase reaction in non- oxidative phase. -
Testing for Differentially Expressed Genes and Key Biological Categories in DNA Microarray Analysis
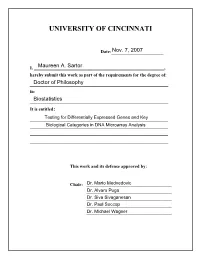
UNIVERSITY OF CINCINNATI Date:___________________ I, _________________________________________________________, hereby submit this work as part of the requirements for the degree of: in: It is entitled: This work and its defense approved by: Chair: _______________________________ _______________________________ _______________________________ _______________________________ _______________________________ Testing for Differentially Expressed Genes and Key Biological Categories in DNA Microarray Analysis A dissertation submitted to the Graduate School of the University of Cincinnati In partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in the Department of Environmental Health of the College of Medicine 2007 By Maureen A. Sartor Masters in Biomathematics, North Carolina State University, August 2000 B.S., Xavier University, Cincinnati, Ohio, 1998 Committee Chair: Dr. Mario Medvedovic ABSTRACT DNA microarrays are a revolutionary technology able to measure the expression levels of thousands of genes simultaneously, providing a snapshot in time of a tissue or cell culture‟s transcriptome. Although microarrays have been in existence for several years now, research is yet ongoing for how to best analyze the data, at least partly due to the combination of small sample sizes (few replicates) with large numbers of genes. Several challenges remain in maximizing the amount of biological information attainable from a microarray experiment. The key components of microarray analysis where these challenges lie are experimental design, preprocessing, statistical inference, identifying expression patterns, and understanding biological relevance. In this dissertation we aim to improve the analysis and interpretation of microarray data by concentrating on two key steps in microarray analysis: obtaining accurate estimates of significance when testing for differentially expressed genes, and identifying key biological functions and cellular pathways affected by the experimental conditions. -

Chemoenzymatic Synthesis of Novel, Structurally Diverse Compounds
Chemoenzymatic synthesis of novel, structurally diverse compounds A Thesis Submitted for the Degree of Doctor of Philosophy to the University of London Lydia G Coward Department of Biochemical Engineering University College London 1 I, Lydia Grace Coward confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. 2 For my fantastic family. 3 Abstract The use of Diels Alder cycloaddition chemistries to access a diverse range of useful cyclic structures is well established throughout literature. However, the value of the product may be enhanced further still by linking this reaction with subsequent (biocatalytic) steps to create novel, structurally demanding, optically pure compounds. This project investigates the linking of Diels Alder (DA) chemistry to the enzyme, transketolase (TK) as a model integration pathway of a chemical syntheses and a biological transformation. The two-step process aims to provide a framework to synthesise small structurally diverse compounds with high enantiomeric excess. The demand for optically pure compounds is becoming a necessity due to the adverse affects frequently introduced by racemic compounds and the cost implications of the material possessing often only 50% active compound. Recombinant wild type Eschericha coli transketolase (EC 2.2.1.1) (WT-TK) was overexpressed in E. coli for the biocatalytic step of this two step synthesis. A substrate walking approach whereby a range of sequentially linked cyclic aldehydes, were applied to wild type transketolase and potential activity detected. Transketolase mutants, previously constructed based on information derived from the structural position within the active site of the dimeric enzyme were subsequently screened for activity with the cycloadduct of the Diels Alder reaction as aldehyde acceptor substrate for TK. -

Transketolase-Like 1 Expression Is Modulated During Colorectal Cancer Progression and Metastasis Formation
Transketolase-Like 1 Expression Is Modulated during Colorectal Cancer Progression and Metastasis Formation Santiago Diaz-Moralli1, Miriam Tarrado-Castellarnau1, Cristina Alenda2, Antoni Castells3, Marta Cascante1* 1 Departament de Bioquimica i Biologia Molecular, Facultat de Biologia, Institut de Biomedicina at Universitat de Barcelona IBUB and IDIBAPS-Hospital Clinic, University of Barcelona, Barcelona, Spain, 2 Pathology Department, Hospital General Universitario de Alicante, Alicante, Spain, 3 Gastroenterology Department, Hospital Clı´nic, IDIBAPS, CIBEREHD, University of Barcelona, Barcelona, Spain Abstract Background: Transketolase-like 1 (TKTL1) induces glucose degradation through anaerobic pathways, even in presence of oxygen, favoring the malignant aerobic glycolytic phenotype characteristic of tumor cells. As TKTL1 appears to be a valid biomarker for cancer prognosis, the aim of the current study was to correlate its expression with tumor stage, probability of tumor recurrence and survival, in a series of colorectal cancer patients. Methodolody/Principal Findings: Tumor tissues from 63 patients diagnosed with colorectal cancer at different stages of progression were analyzed for TKTL1 by immunohistochemistry. Staining was quantified by computational image analysis, and correlations between enzyme expression, local growth, lymph-node involvement and metastasis were assessed. The highest values for TKTL1 expression were detected in the group of stage III tumors, which showed significant differences from the other groups (Kruskal-Wallis test, P = 0.000008). Deeper analyses of T, N and M classifications revealed a weak correlation between local tumor growth and enzyme expression (Mann-Whitney test, P = 0.029), a significant association of the enzyme expression with lymph-node involvement (Mann-Whitney test, P = 0.0014) and a significant decrease in TKTL1 expression associated with metastasis (Mann-Whitney test, P = 0.0004). -

PENTOSE PHOSPHATE PATHWAY — Restricted for Students Enrolled in MCB102, UC Berkeley, Spring 2008 ONLY
Metabolism Lecture 5 — PENTOSE PHOSPHATE PATHWAY — Restricted for students enrolled in MCB102, UC Berkeley, Spring 2008 ONLY Bryan Krantz: University of California, Berkeley MCB 102, Spring 2008, Metabolism Lecture 5 Reading: Ch. 14 of Principles of Biochemistry, “Glycolysis, Gluconeogenesis, & Pentose Phosphate Pathway.” PENTOSE PHOSPHATE PATHWAY This pathway produces ribose from glucose, and it also generates 2 NADPH. Two Phases: [1] Oxidative Phase & [2] Non-oxidative Phase + + Glucose 6-Phosphate + 2 NADP + H2O Ribose 5-Phosphate + 2 NADPH + CO2 + 2H ● What are pentoses? Why do we need them? ◦ DNA & RNA ◦ Cofactors in enzymes ● Where do we get them? Diet and from glucose (and other sugars) via the Pentose Phosphate Pathway. ● Is the Pentose Phosphate Pathway just about making ribose sugars from glucose? (1) Important for biosynthetic pathways using NADPH, and (2) a high cytosolic reducing potential from NADPH is sometimes required to advert oxidative damage by radicals, e.g., ● - ● O2 and H—O Metabolism Lecture 5 — PENTOSE PHOSPHATE PATHWAY — Restricted for students enrolled in MCB102, UC Berkeley, Spring 2008 ONLY Two Phases of the Pentose Pathway Metabolism Lecture 5 — PENTOSE PHOSPHATE PATHWAY — Restricted for students enrolled in MCB102, UC Berkeley, Spring 2008 ONLY NADPH vs. NADH Metabolism Lecture 5 — PENTOSE PHOSPHATE PATHWAY — Restricted for students enrolled in MCB102, UC Berkeley, Spring 2008 ONLY Oxidative Phase: Glucose-6-P Ribose-5-P Glucose 6-phosphate dehydrogenase. First enzymatic step in oxidative phase, converting NADP+ to NADPH. Glucose 6-phosphate + NADP+ 6-Phosphoglucono-δ-lactone + NADPH + H+ Mechanism. Oxidation reaction of C1 position. Hydride transfer to the NADP+, forming a lactone, which is an intra-molecular ester. -

Genomic and Expression Profiling of Human Spermatocytic Seminomas: Primary Spermatocyte As Tumorigenic Precursor and DMRT1 As Candidate Chromosome 9 Gene
Research Article Genomic and Expression Profiling of Human Spermatocytic Seminomas: Primary Spermatocyte as Tumorigenic Precursor and DMRT1 as Candidate Chromosome 9 Gene Leendert H.J. Looijenga,1 Remko Hersmus,1 Ad J.M. Gillis,1 Rolph Pfundt,4 Hans J. Stoop,1 Ruud J.H.L.M. van Gurp,1 Joris Veltman,1 H. Berna Beverloo,2 Ellen van Drunen,2 Ad Geurts van Kessel,4 Renee Reijo Pera,5 Dominik T. Schneider,6 Brenda Summersgill,7 Janet Shipley,7 Alan McIntyre,7 Peter van der Spek,3 Eric Schoenmakers,4 and J. Wolter Oosterhuis1 1Department of Pathology, Josephine Nefkens Institute; Departments of 2Clinical Genetics and 3Bioinformatics, Erasmus Medical Center/ University Medical Center, Rotterdam, the Netherlands; 4Department of Human Genetics, Radboud University Medical Center, Nijmegen, the Netherlands; 5Howard Hughes Medical Institute, Whitehead Institute and Department of Biology, Massachusetts Institute of Technology, Cambridge, Massachusetts; 6Clinic of Paediatric Oncology, Haematology and Immunology, Heinrich-Heine University, Du¨sseldorf, Germany; 7Molecular Cytogenetics, Section of Molecular Carcinogenesis, The Institute of Cancer Research, Sutton, Surrey, United Kingdom Abstract histochemistry, DMRT1 (a male-specific transcriptional regulator) was identified as a likely candidate gene for Spermatocytic seminomas are solid tumors found solely in the involvement in the development of spermatocytic seminomas. testis of predominantly elderly individuals. We investigated these tumors using a genome-wide analysis for structural and (Cancer Res 2006; 66(1): 290-302) numerical chromosomal changes through conventional kar- yotyping, spectral karyotyping, and array comparative Introduction genomic hybridization using a 32 K genomic tiling-path Spermatocytic seminomas are benign testicular tumors that resolution BAC platform (confirmed by in situ hybridization). -

Pentose Phosphate Pathway
Metabolism: Pentose phosphate pathway Hand-out for the CBT – version May 2012 1. Which of the following compounds are products of the pentose phosphate pathway? o NADPH o glycerate 3-phosphate o CO2 o ribulose 5-phosphate o sedoheptulose 7-phosphate 2. The first four reactions of the pentose phosphate pathway form the oxidative phase. The following questions deal with these reactions. A. What are the names of these compounds? B. During which reactions are CO2 and NADPH produced? C. What reaction is catalyzed by phosphopentose isomerase? D. Which compound can be a group acceptor in the transketolase reaction? 3. The following questions are about glucose 6-phosphate dehydrogenase. A. Is 6-phosphogluconate one of its products? B. Is it regulated by the availability of NAD+? C. Does is contain thiamine pyrophosphate as a cofactor? D. A committed step is an effectively irreversible enzymatic reaction that occurs in metabolic reactions during the biosynthesis of some molecules. Does glucose 6-phosphate dehydrogenase catalyse the committed step in the pentose phosphate pathway? E. Is it important in the metabolism of glutathione in erythrocytes? 4. The pentose phosphate pathway has a nonoxidative branch. What reactions does it include? 5. The liver synthesizes fatty acids and lipids for export to other tissues. What activity do you expect the pentose phosphate pathway to have in the liver? o Low, because this synthesis needs ATP and pentoses as a source o Low, because no reductive force is needed o High, because this is reductive biosynthesis o High, because the conversion of sugars is required 6. A. -

Expression Analysis of the Imprinted Gene Transketolase-Like 1 in Mouse and Human Amy F
University of Connecticut OpenCommons@UConn Master's Theses University of Connecticut Graduate School 5-7-2011 Expression Analysis of the Imprinted Gene Transketolase-like 1 in Mouse and Human Amy F. Friss University of Connecticut - Storrs, [email protected] Recommended Citation Friss, Amy F., "Expression Analysis of the Imprinted Gene Transketolase-like 1 in Mouse and Human" (2011). Master's Theses. 90. https://opencommons.uconn.edu/gs_theses/90 This work is brought to you for free and open access by the University of Connecticut Graduate School at OpenCommons@UConn. It has been accepted for inclusion in Master's Theses by an authorized administrator of OpenCommons@UConn. For more information, please contact [email protected]. Expression Analysis of the Imprinted Gene Transketolase-like 1 in Mouse and Human Amy Frances Friss University of Connecticut Abstract Genomic imprinting is an epigenetic phenomenon resulting in differential gene expression based on parental origin. Recently, transketolase-like 1 (TKTL1) has been identified as an X-linked imprinted gene. TKTL1 functions in the nonoxidative branch of the pentose phosphate pathway (PPP), which maintains glutathione in a reduced state through the generation of NADPH. Previous studies on transaldolase, the other critical enzyme in the nonoxidative branch of the PPP, suggest that TKTL1 may affect the cell’s ability to reduce glutathione. This study provides evidence that TKTL1 overexpression inhibits glutathione reduction. Intriguingly, aberrant glutathione levels are associated with autism. Additionally, studies involving Turner syndrome females found that differences in social behavior could distinguish females expressing the maternal X chromosome from those expressing the paternal X chromosome.