Medicaid List of Covered Drugs (Formulary)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minutes of the CHMP Meeting 14-17 September 2020
13 January 2021 EMA/CHMP/625456/2020 Corr.1 Human Medicines Division Committee for medicinal products for human use (CHMP) Minutes for the meeting on 14-17 September 2020 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in these minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, these minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). 1 Addition of the list of participants Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

Acebutolol Hydrochloride Eq 200 Mg Base, Capsule, Oral, 100 0.4612 B Eq 400 Mg Base, Capsule, Oral, 100 0.6713 B
TRANSMITTAL NO. 37 - FEDERAL UPPER LIMIT DRUG LIST NOVEMBER 20, 2001 The following list of multiple source drugs meets the criteria set forth in 42 CFR 447.332 and Section 1927(e) of the Social Security Act, as amended by OBRA 1993. Payment for multiple source drugs identified and listed below must not exceed, in the aggregate, payment levels determined by applying to each drug entity a reasonable dispensing fee (established by the State and specified in the State plan), plus an amount based on the limit per unit which CMS has determined to be equal to 150 percent applied to the lowest price listed (in package sizes of 100 units, unless otherwise noted) in any of the published compendia of cost information of drugs. The listing is based on data current as of April 2001 from First Data Bank (Blue Book), Medi- Span, and the Red Book. This list does not reference the commonly known brand names. However, the brand names are included in the electronic FUL listing provided to the state agencies. The FUL price list and electronic listing are available at http://www.cms.hhs.gov/Reimbursement/05_FederalUpperLimits.asp. In accordance with current policy, Federal financial participation will not be provided for any drug on the FUL listing for which the FDA has issued a notice of an opportunity for a hearing as a result of the Drug Efficacy Study and Implementation (DESI) program, and which has been found to be a less than effective or is identical, related or similar (IRS) to the DESI drug. The DESI drug is identified by the Food and Drug Administration or reported by the drug manufacturer for purposes of the Medicaid drug rebate program. -

Crohn's & Colitis Program, Patient Information Guide
Inflammatory Bowel Disease Program Patient Information Guide Page # Contents ..........................................................................................................................................1 Welcome! Welcome Letter ....................................................................................................................3 Important Things to Know Up Front ....................................................................................4 Meet Your Crohn’s & Colitis Team .....................................................................................6 How to Contact Us Crohn’s & Colitis Clinic Schedule .....................................................................................11 Physician and Nurse Contact Information..........................................................................12 Appointment Scheduling and Other Contact Information..................................................13 The Basics of Inflammatory Bowel Disease (IBD) Basic Information about Inflammatory Bowel Disease (IBD) ...........................................14 Frequently Asked Questions about Inflammatory Bowel Disease (IBD) ..........................18 Testing in IBD Colonoscopy and Flexible Sigmoidoscopy ........................................................................20 Upper Endoscopy ...............................................................................................................21 Capsule Endoscopy and Deep Enteroscopy .......................................................................22 -

Updated: May 20, 2021 Prior Authorization Drugs (NEW ADDITIONS HIGHLIGHTED)
Updated: May 20, 2021 Prior Authorization Drugs (NEW ADDITIONS HIGHLIGHTED) A Abatacept (ORENCIA) Abemaciclib (VERZENIO) Abiraterone Acetate (ZYTIGA) Abiraterone Acetate (+ GENERIC FORMULATIONS) AbobotulinumtoxinA (DYSPORT) Abraxane (ABRAXANE) Acalabrutinib (CALQUENCE) Actemra (ACTEMRA) Adalimumab (AMGEVITA) Adalimumab (HADLIMA) Adalimumab (HULIO) Adalimumab (HUMIRA) Adalimumab (HYRIMOZ) Adalimumab (IDACIO) Adcetris (ADCETRIS) Adcirca (ADCIRCA) Adempas (ADEMPAS) Afatinib (GIOTRIF) Afinitor (AFINITOR) Aflibercept (EYLEA) Aflibercept (ZALTRAP) Afstyla (AFSTYLA) Agalsidase Alfa (REPLAGAL) Agalsidase Beta (FABRAZYM) Aimovig (AIMOVIG) Ajovy (FREMANEZUMAB) Aldesleukin (PROLEUKIN) Aldurazyme (ALDURAZYME) Alecensaro (ALECENSARO) Alectinib (ALECENSARO) Alefacept (AMEVIVE) Alemtuzumab (MABCAMPATH) Alemtuzumab (LEMTRADA) Alglucosidase Alfa (MYOZYME) Alimta (ALIMTA) Alirocumab (PRALUENT) Alpha-1-Proteinase Inhibitor (PROLASTIN - C) Alpha-1-Proteinase Inhibitor (ZEMAIRA) Alpelisib (PIQRAY) Alunbrig (ALUNBRIG) Ambrisentan (VOLIBRIS) Ambrisentan (Generic Formulations) Amevive (AMEVIVE) Amgevita (ADALIMUMAB) Amifampridine Phosphate (FIRDAPSE) Amifampridine Phosphate (RUZURGI) Anakinra (KINERET) Apalutamide (ERLEADA) Apomorphine (KYNMOBI) Apremilast (OTEZLA) Page 1 of 17 Updated: May 20, 2021 Arsenic Trioxide (TRISENOX) Arsenic Trioxide (Generic Formulations) Arzerra (ARZERRA) Asfotase Alfa (STRENSIQ) Asparaginase (ERWINASE) Asunaprevir (SUNVEPRA) Atezolizumab (TECENTRIQ) Atriance (ATRIANCE) Aubagio (AUBAGIO) Avastin (AVASTIN) Avelumab (BAVENCIO) Avonex -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Pharmacokinetic Drug–Drug Interactions Among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients
International Journal of Molecular Sciences Review Pharmacokinetic Drug–Drug Interactions among Antiepileptic Drugs, Including CBD, Drugs Used to Treat COVID-19 and Nutrients Marta Kara´zniewicz-Łada 1 , Anna K. Główka 2 , Aniceta A. Mikulska 1 and Franciszek K. Główka 1,* 1 Department of Physical Pharmacy and Pharmacokinetics, Poznan University of Medical Sciences, 60-781 Pozna´n,Poland; [email protected] (M.K.-Ł.); [email protected] (A.A.M.) 2 Department of Bromatology, Poznan University of Medical Sciences, 60-354 Pozna´n,Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-(0)61-854-64-37 Abstract: Anti-epileptic drugs (AEDs) are an important group of drugs of several generations, rang- ing from the oldest phenobarbital (1912) to the most recent cenobamate (2019). Cannabidiol (CBD) is increasingly used to treat epilepsy. The outbreak of the SARS-CoV-2 pandemic in 2019 created new challenges in the effective treatment of epilepsy in COVID-19 patients. The purpose of this review is to present data from the last few years on drug–drug interactions among of AEDs, as well as AEDs with other drugs, nutrients and food. Literature data was collected mainly in PubMed, as well as google base. The most important pharmacokinetic parameters of the chosen 29 AEDs, mechanism of action and clinical application, as well as their biotransformation, are presented. We pay a special attention to the new potential interactions of the applied first-generation AEDs (carba- Citation: Kara´zniewicz-Łada,M.; mazepine, oxcarbazepine, phenytoin, phenobarbital and primidone), on decreased concentration Główka, A.K.; Mikulska, A.A.; of some medications (atazanavir and remdesivir), or their compositions (darunavir/cobicistat and Główka, F.K. -

Migraine Specialty Care Program Tm
MIGRAINE SPECIALTY CARE PROGRAM TM Phone: 833-796-6470 • Fax: 844-841-3401 Community Led Specialty Pharmacy Care 1 PATIENT INFORMATION: 2 PRESCRIBER INFORMATION: Name: ___________________________________________________ Name: ___________________________________________________ Address: _________________________________________________ Address: _________________________________________________ City: _________________________ State: ____ Zip: ____________ City: _________________________ State: ____ Zip: ____________ Phone: ___________________ Alt. Phone: ____________________ Phone: _____________________ Fax: _______________________ Email: ____________________________________________________ NPI: ________________________ DEA: _______________________ DOB: ___________ Gender: M F Caregiver: _____________ Tax I.D.: __________________________________________________ Height: ________ Weight: ________ Allergies: ________________ Office Contact: __________________ Phone: __________________ 3 STATEMENT OF MEDICAL NECESSITY: (Please Attach All Medical Documentation) Prior Failed Indicate Drug Name v10.0_060821 Length of Symptoms: ___________________________ ICD-10: _________________________ Treatments: and Length of Treatment: Other diagnosis _______________ Number of Migraine Days per month: ________________ Preventative: Headache Days per month: _________________ Migraine Hours per day: __________________ ACE-I/ARBs ___________________ Patient has been evaluated and does not have medication overuse headache? No Yes Antiepileptics ___________________ -

Inflammatory Bowel Disease Agents
Therapeutic Class Overview Inflammatory Bowel Disease Agents INTRODUCTION • Inflammatory bowel disease (IBD) is a spectrum of chronic idiopathic inflammatory intestinal conditions that cause gastrointestinal symptoms including diarrhea, abdominal pain, bleeding, fatigue, and weight loss. The exact cause of IBD is unknown; however, proposed etiologies involve a combination of infectious, genetic, and lifestyle factors (Bernstein et al 2015, Peppercorn 2019[a], Peppercorn 2020[c]). • Complications of IBD include hemorrhage, rectal fissures, fistulas, peri-rectal and intra-abdominal abscesses, and colon cancer. Possible extra-intestinal complications include hepatobiliary complications, anemia, arthritis and arthralgias, uveitis, skin lesions, and mood and anxiety disorders (Bernstein et al 2015). • Ulcerative colitis (UC) and Crohn’s disease (CD) are 2 forms of IBD that differ in pathophysiology and presentation; as a result of these differences, the approach to the treatment of each condition often differs (Peppercorn 2019[a]). • UC is characterized by recurrent episodes of inflammation of the mucosal layer of the colon. The inflammation, limited to the mucosa, commonly involves the rectum and may extend in a proximal and continuous fashion to affect other parts of the colon. The hallmark clinical symptom is an inflamed rectum with symptoms of urgency, bleeding, and tenesmus (Peppercorn 2020[c], Rubin et al 2019). • CD can involve any part of the gastrointestinal tract and is characterized by transmural inflammation and “skip areas.” Transmural inflammation may lead to fibrosis, strictures, sinus tracts, and fistulae (Peppercorn 2019[b]). • The immune system is known to play a critical role in the underlying pathogenesis of IBD. It is suggested that abnormal responses of both innate and adaptive immunity mechanisms induce aberrant intestinal tract inflammation in IBD patients (Geremia et al 2014). -

Anticholinergic Drugs Improve Symptoms but Increase Dry Mouth in Adults with Overactive Bladder Syndrome
Source of funding: Evid Based Nurs: first published as 10.1136/ebn.6.2.49 on 1 April 2003. Downloaded from Review: anticholinergic drugs improve symptoms but Health Research Council of Aotearoa increase dry mouth in adults with overactive bladder New Zealand. syndrome For correspondence: Jean Hay-Smith, Hay-Smith J, Herbison P,Ellis G, et al. Anticholinergic drugs versus placebo for overactive bladder syndrome in adults. Dunedin School of Cochrane Database Syst Rev 2002;(3):CD003781 (latest version May 29 2002). Medicine, University of Otago, Dunedin, New QUESTION: What are the effects of anticholinergic drugs in adults with overactive Zealand. jean.hay-smith@ bladder syndrome? otago.ac.nz Data sources Parallel arm studies of anticholinergic drugs v placebo for overactive bladder syndrome in Studies were identified by searching the Cochrane adults at 12 days to 12 weeks* Incontinence Group trials register (to January 2002) Weighted event rates and reference lists of relevant papers. Anticholinergic Study selection Outcomes drugs Placebo RBI (95% CI) NNT (CI) Randomised or quasi-randomised controlled trials in Self reported cure or adults with symptomatic diagnosis of overactive bladder improvement (8 studies) 63% 45% 41% (29 to 54) 6 (5 to 8) syndrome, urodynamic diagnosis of detrusor overactiv- RRI (CI) NNH (CI) ity, or both, that compared an anticholinergic drug Dry mouth (20 studies) 36% 15% 138 (70 to 232) 5 (4 to 7) (given to decrease symptoms of overactive bladder) with Outcomes Weighted mean difference (CI) placebo or no treatment. Studies of darifenacin, emepronium bromide or carrageenate, dicyclomine Number of leakage episodes in 24 hours (9 − chloride, oxybutynin chloride, propiverine, propanthe- studies) 0.56 (–0.73 to –0.39) Number of micturitions in 24 hours (8 studies) −0.59 (–0.83 to –0.36) line bromide, tolterodine, and trospium chloride were Maximum cystometric volume (ml) (12 studies) 54.3 (43.0 to 65.7) included. -

761094Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 761094Orig1s000 CLINICAL REVIEW(S) Medical Officer’s Review of BLA 761094 Review #2 BLA 761094 Submission Date: July 19, 2018 Receipt Date: July 19, 2018 Review Date: July 23, 2018 Applicant: Dompé farmaceutici S.p.A. Via Santa Lucia 6-20122 Milan, Italy Applicant’s Representative: Lamberto Dionigi. Regulatory Affairs & Drug Safety Director 39-02-5838-3559 Drug: OXERVATE (cenegermin – bkbj) ophthalmic solution, 20 mcg/mL Submitted: Reference is made to the meeting Teleconference of 15-July-2018, in which the FDA has requested to provide information available at Dompé on the use of Oxervate in the pediatric population. Pediatric patients exposed to Oxervate: Dompé confirms that Oxervate is not yet approved in Europe for use in children and no clinical studies have been conducted in this population. As far as the company is aware, four (4) Neurotrophic Keratitis (NK) pediatric patients, aged from 2 to 12 years of age, have been exposed to Oxervate. A 6-year-old child with severe NK secondary to Stuve-Wiedmann syndrome was treated with Oxervate under “Temporary Authorization for Use” (ATU) in France. Dompé reports that the corneal ulcer was completely healed at the end of the treatment. There were signs of corneal sensitivity recovery by month 8 post-treatment. A 9-year-old child with NK was treated with Oxervate under ATU in France. Dompé reports that the lesion improved, but did not completely heal with the treatment. There is no other follow-up information available. A 12-year-old child with severe NK was treated with Oxervate under Expanded Access in the US. -
Changes to the Highmark Drug Formularies
AUGUST 2020 JULY/AUGUST 2020 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the update to the Highmark Drug Formularies and pharmaceutical management procedures for July/August 2020. The formularies and pharmaceutical management procedures are updated on a bimonthly basis, and the following changes reflect the decisions made in June 2020 by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Progressive Formulary and the Highmark Progressive Healthcare Reform Formulary C. Changes to the Highmark Healthcare Reform Essential Formulary D. Changes to the Highmark Core Formulary E. Changes to the Highmark National Select Formulary F. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Programs Section II. Highmark Medicare Part D Formularies A. Changes to the Highmark Medicare Part D 5-Tier Incentive Formulary B. Changes to the Highmark Medicare Part D 5-Tier Closed Formulary C. Additions to the Specialty Tier D. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Quantity Level Limit (QLL) Program As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy Program/Formularies link from the menu on the left. -
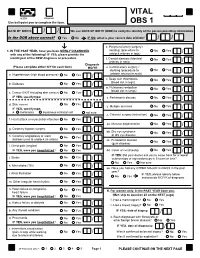
VITAL Jan 2019 Follow-Up
VITAL 6308 Request Use ball-point pen to complete the form. OBS 1 DATE OF BIRTH: / / We use DATE OF BIRTH (DOB) to verify the identity of the person providing information. Is the DOB above correct? Yes No IF NO, what is your correct date of birth? / / s. Peripheral artery surgery / 1. IN THE PAST YEAR, have you been NEWLY DIAGNOSED stenting (procedure to No Yes / with any of the following? IF YES, please provide the unblock arteries in legs) month/year of the NEW diagnosis or procedure. t. Carotid stenosis (blocked No Yes Answer NO/YES on each line. arteries in neck) / Diagnosis (Please complete either N/Y for each item) MO/YR u. Carotid artery surgery / stenting (procedure to No Yes / a. Hypertension (high blood pressure) No Yes / unblock arteries in neck) v. Deep vein thrombosis No Yes (blood clot in legs) / b. Diabetes No Yes / w. Pulmonary embolism No Yes (blood clot in lungs) / c. Cancer (NOT including skin cancer) No Yes / IF YES, specify type: _______________________ x. Parkinson's disease No Yes / d. Skin cancer No Yes / y. Multiple sclerosis No Yes IF YES, specify type: / e. melanoma squamous or basal cell not sure z. Cataract surgery (extraction) No Yes / f. Heart attack or myocardial infarction No Yes / aa. Macular degeneration No Yes / g. Coronary bypass surgery No Yes / bb. Dry eye syndrome No Yes or dry eye disease / h. Coronary angioplasty or stent No Yes (balloon used to unblock an artery) / cc. Periodontal disease No Yes (gum disease) / i. Chest pain (angina) No Yes / IF YES, were you hospitalized? No Yes dd.