Dermatofibrosarcoma Protuberans
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mixed Hepatoblastoma in the Adult: Case Report and Review of the Literature
J Clin Pathol: first published as 10.1136/jcp.33.11.1058 on 1 November 1980. Downloaded from J Clin Pathol 1980;33:1058-1063 Mixed hepatoblastoma in the adult: case report and review of the literature RP HONAN AND MT HAQQANI From the Department of Pathology, Walton Hospital, Rice Lane, Liverpool L9 JAE, UK SUMMARY A case of mixed hepatoblastoma in a woman is described. A survey of the English literature reveals 13 cases acceptable as mixed hepatoblastoma; these have been described and published under a variety of names. Difficulties in nomenclature and the histology of these cases are discussed. Diagnosis depends on the identification of both malignant mesenchymal and malignant epithelial elements. The former include myxoid connective tissue resembling primitive mesenchyme and areas resembling adult fibrosarcoma. Mature fibrous tissue with calcification and bone for- mation may be seen. Epithelial areas show tissue resembling fetal liver, poorly differentiated epithelial cells, and/or areas of adenocarcinoma. The current view on histogenesis is also given. Most hepatoblastomas occur in children under the mixedtumour,6carcino-osteochondromyxosarcoma,5 copyright. age of 2 years.' Hepatoblastoma in adults is ex- and rhabdomyosarcohepatoma.7 tremely rare, and the prognosis is much worse than in the mixed hepatoblastoma of childhood. Case report The literature of mixed hepatoblastoma in adults has until recently been confused, and the true inci- CLINICAL PRESENTATION dence of the tumour obscured, owing to the various A Chinese woman aged 27 had been resident in names used by different authors to describe their England for eight years. She gave a history of cases. The commonest pseudonym is 'mixed malig- 18 months' intermittent right-sided chest pain http://jcp.bmj.com/ nant tumour',2-4 an ambivalent term which merely and upper abdominal discomfort. -

Radiation-Associated Synovial Sarcoma
Radiation-Associated Synovial Sarcoma: Clinicopathologic and Molecular Analysis of Two Cases Jean-François Egger, M.D., Jean-Michel Coindre, M.D., Jean Benhattar, Ph.D., Philippe Coucke, M.D., Louis Guillou, M.D. University Institute of Pathology (J-FE, JB, LG) and Department of Radiooncology, University Hospital (PC), Lausanne, Switzerland; Bergonié Institute and University of Bordeaux II (J-MC), Bordeaux, France region, or viscera (1, 2). SS bears the t(X;18) (SYT- Development of a soft-tissue sarcoma is an infre- SSX) reciprocal translocation that seems to be spe- quent but well-known long-term complication of cific for this tumor type and can be routinely de- radiotherapy. Malignant fibrous histiocytomas, ex- tected in paraffin-embedded tissue using the traskeletal osteosarcomas, fibrosarcomas, malig- reverse transcriptase–polymerase chain reaction nant peripheral nerve sheath tumors, and angiosar- (RT-PCR; 3–6). Radiation-associated sarcomas are comas are most frequently encountered. Radiation- an infrequent but well-known long-term complica- associated synovial sarcomas are exceptional. We tion of radiotherapy (7–16). They occur in about report the clinicopathologic, immunohistochemi- 1/1000 patients who have undergone radiation cal, and molecular features of two radiation- therapy (7–11). Radiation-associated sarcomas are associated synovial sarcomas. One tumor developed defined as sarcomas arising in a previously irradi- in a 42-year-old female 17 years after external irra- ated field after a latency period of Ն2 years (12). diation was given for breast carcinoma; the other They usually show a more aggressive clinical course occurred in a 34-year-old female who was irradiated associated with shortened patient survival as com- at the age of 7 years for a nonneoplastic condition of pared with sporadic sarcomas (9–12, 14). -

Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010)
DOI: 10.2478/v10163-012-0008-6 ACTA CHIRURGICA LATVIENSIS • 2011 (11) ORIGINAL ARTICLE Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010) Ivanda Franckeviča*,**, Regīna Kleina*, Ivars Melderis** *Riga Stradins University, Riga, Latvia **Children’s Clinical University Hospital, Riga, Latvia Summary Introduction. Paediatric renal tumours represent 7% of all childhood malignancies. The variable appearances of the tumours and their rarity make them especially challenging group of lesions for the paediatric pathologist. In Latvia diagnostics and treatment of childhood malignancies is concentrated in Children’s Clinical University Hospital. Microscopic evaluation of them is realised in Pathology office of this hospital. Aim of the study is to analyze morphologic spectrum of children kidney tumours in Latvia and to characterise them from modern positions with wide range of immunohistochemical markers using morphological material of Pathology bureau of Children’s Clinical University Hospital. Materials and methods. We have analyzed surgically removed primary renal tumours in Children Clinical University Hospital from the year 1997 till 2010. Samples were fixed in 10% formalin fluid, imbedded in paraffin and haematoxylin-eosin stained slides were re-examined. Immunohistochemical re-investigation was made in 65.91% of cases. For differential diagnostic purposes were used antibodies for the detection of bcl-2, CD34, EMA, actin, desmin, vimentin, CKAE1/AE3, CK7, Ki67, LCA, WT1, CD99, NSE, chromogranin, synaptophyzin, S100, myoglobin, miogenin, MyoD1 (DakoCytomation) and INI1 protein (Santa Cruz Biotechnology). Results. During the revised period there were diagnosed 44 renal tumours. Accordingly of morphological examination data neoplasms were divided: 1) nephroblastoma – 75%, 2) clear cell sarcoma – 2.27%, 3) rhabdoid tumour – 4.55%, 4) angiomyolipoma – 4.55%, 5) embrional rhabdomyosarcoma – 2.27%, 6) mesoblastic nephroma – 4.55%, 7) multicystic nephroma – 4.55%, 8) angiosarcoma – 2.27%. -

Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report
The Korean Journal of Pathology 2004; 38: 276-9 Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report - Ok-Jun Lee∙David Y. Pi∙ Dermatofibrosarcoma protuberans (DFSP) typically presents during the early or mid-adult life, Daniel H. Jo∙Kyung-Ja Cho and the most common site of origin is the skin on the trunk and proximal extremities. DFSP of Sang Yoon Kim1∙Jae Y. Ro the parotid gland is extremely rare and only one case has been reported in the literature. We present here a case of a 30-year-old woman with DFSP occurring in the parotid gland, and we Departments of Pathology and discuss the differential diagnosis. The patient is alive and doing well one year after her operation. 1Otolaryngology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea Received : January 27, 2004 Accepted : July 5, 2004 Corresponding Author Jae Y. Ro, M.D. Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, 388-1 Pungnap-dong, Songpa-gu, Seoul 138-736, Korea Tel: 02-3010-4550 Fax: 02-472-7898 E-mail: [email protected] Key Words : Dermatofibrosarcoma Protuberans-Parotid Gland Epithelial tumors make up the majority of salivary gland neo- CASE REPORT plasms, while mesenchymal tumors of this organ are uncommon. Dermatofibrosarcoma protuberans (DFSP) of the salivary gland A 30-year-old woman came to the Otolaryngology Clinic at is exremely rare and only one case has been reported in the parotid the Asan Medical Center with a 2-year history of a slowly enlarg- gland.1 ing mass inferior to the left angle of the mandible. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

P05: Incidence Rates of Neoplasms by Anatomic Site (Systemic
TDMS No. 88123 - 07 P05: INCIDENCE RATES OF NEOPLASMS BY ANATOMIC SITE (SYSTEMIC Date Report Reqsted: 05/04/2006 LESIONS ABRIDGED) (a) Test Type: CHRONIC FORMAMIDE Time Report Reqsted: 11:47:08 Route: GAVAGE CAS Number: 75-12-7 First Dose M/F: 10/04/01 / 10/03/01 Species/Strain: MICE/B6C3F1 Pathologist: RYAN, M. - Blackshear, P. Lab: BAT F1_M3 C Number: C88123B Lock Date: 05/24/2004 Cage Range: ALL Date Range: ALL Reasons For Removal: ALL Removal Date Range: ALL Treatment Groups: Include ALL TDMS No. 88123 - 07 P05: INCIDENCE RATES OF NEOPLASMS BY ANATOMIC SITE (SYSTEMIC Date Report Reqsted: 05/04/2006 LESIONS ABRIDGED) (a) Test Type: CHRONIC FORMAMIDE Time Report Reqsted: 11:47:08 Route: GAVAGE CAS Number: 75-12-7 First Dose M/F: 10/04/01 / 10/03/01 Species/Strain: MICE/B6C3F1 Pathologist: RYAN, M. - Blackshear, P. Lab: BAT B6C3F1 MICE MALE 0 MG/KG 20 MG/KG 40 MG/KG 80 MG/KG Disposition Summary Animals Initially in Study 50 50 50 50 Early Deaths Moribund Sacrifice 4 8 6 14 Natural Death 7 8 3 Survivors Terminal Sacrifice 39 42 36 33 Animals Examined Microscopically 50 50 50 50 ALIMENTARY SYSTEM Esophagus (50) (50) (50) (50) Periesophageal Tissue, 1 (2%) Hepatocholangiocarcinoma, Metastatic, Liver Gallbladder (45) (48) (45) (46) Intestine Large, Cecum (50) (50) (50) (50) Intestine Large, Colon (50) (50) (50) (50) Intestine Large, Rectum (50) (50) (50) (50) Intestine Small, Duodenum (50) (50) (50) (50) Carcinoma, Metastatic, Pancreas 1 (2%) Intestine Small, Ileum (50) (50) (50) (50) Epithelium, Carcinoma 1 (2%) Intestine Small, Jejunum -
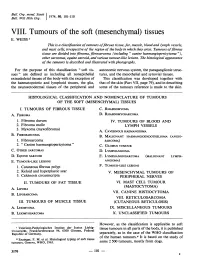
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -
The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -

A Case of Adult Hepatoblastoma
DOI: https://doi.org/10.22516/25007440.339 Case report A case of adult hepatoblastoma Rafael Pila-Pérez, MD,1 Jaider Luis Saurith-Monterrosa, MD,1* Pedro Rosales-Torres, MD,1 Rafael Pila-Peláez, MD,1 Javier Alberto Artola-González, MD.1 1. Manuel Ascunce Domenech Hospital in Abstract Camaguey, Cuba Background: In contrast to childhood hepatoblastoma, adult hepatoblastoma (HBA) is a rare and not-fully- understood liver tumor with a poor prognosis. To date, about 50 cases have been adequately reported in the *Correspondence: Jaider Luis Saurith-Monterrosa, MD, medical literature. Objective: We present the case of a patient who was discharged from our hospital with a [email protected] diagnosis of hepatocellular carcinoma approximately 3 months before returning. Clinical case: A 60-year-old male patient with a history of alcoholism and heavy smoking was admitted to our hospital for abdominal pain. ......................................... Received: 13/01/19 Physical examination revealed a palpable tumor in the right hypochondrium region. This patient had been Accepted: 18/02/19 discharged approximately 3 months previously with a diagnosis of hepatocellular carcinoma in the course of liver cirrhosis. The patient died, and the autopsy revealed an HBA. Conclusions: Adult hepatoblastoma is an infrequent tumor with a severe prognosis. Many cases are asymptomatic until the time of diagnosis, and the tumor is usually very large. Liver enzymes, alpha-fetus protein, and imaging studies lead to a diagnosis of hepatocellular carcinoma which is a common tumor in adults. Histological study confirms the diagnosis. Due to the poor prognosis for HBA in contrast to better prospects for treatment of hepatoblastoma in children, it is logical to use pediatric treatment in adults. -

Immunohistochemical Expression of Wilms' Tumor 1 Protein In
applied sciences Review Immunohistochemical Expression of Wilms’ Tumor 1 Protein in Human Tissues: From Ontogenesis to Neoplastic Tissues Lucia Salvatorelli 1,*, Giovanna Calabrese 2 , Rosalba Parenti 2 , Giada Maria Vecchio 1, Lidia Puzzo 1, Rosario Caltabiano 1 , Giuseppe Musumeci 3 and Gaetano Magro 1 1 Department of Medical and Surgical Sciences and Advanced Technologies, G.F. Ingrassia, Azienda Ospedaliero-Universitaria “Policlinico-Vittorio Emanuele”, Anatomic Pathology Section, School of Medicine, University of Catania, 95123 Catania, Italy; [email protected] (G.M.V.); [email protected] (L.P.); [email protected] (R.C.); [email protected] (G.M.) 2 Department of Biomedical and Biotechnological Sciences, Physiology Section, University of Catania, 95123 Catania, Italy; [email protected] (G.C.); [email protected] (R.P.) 3 Department of Biomedical and Biotechnological Sciences, Human Anatomy and Histology Section, School of Medicine, University of Catania, 95123 Catania, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-095-3702138; Fax: +39-095-3782023 Received: 4 October 2019; Accepted: 10 December 2019; Published: 19 December 2019 Abstract: The human Wilms’ tumor gene (WT1) was originally isolated in a Wilms’ tumor of the kidney as a tumor suppressor gene. Numerous isoforms of WT1, by combination of alternative translational start sites, alternative RNA splicing and RNA editing, have been well documented. During human ontogenesis, according to the antibodies used, anti-C or N-terminus WT1 protein, nuclear expression can be frequently obtained in numerous tissues, including metanephric and mesonephric glomeruli, and mesothelial and sub-mesothelial cells, while cytoplasmic staining is usually found in developing smooth and skeletal cells, myocardium, glial cells, neuroblasts, adrenal cortical cells and the endothelial cells of blood vessels. -

Subcutaneous Dermatofibroma
Ann Dermatol Vol. 23, No. 2, 2011 DOI: 10.5021/ad.2011.23.2.254 CASE REPORT Subcutaneous Dermatofibroma Kyu Dong Jung, M.D., Dong-Youn Lee, M.D., Joo-Heung Lee, M.D., Jun-Mo Yang, M.D., Eil-Soo Lee, M.D. Department of Dermatology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea Dermatofibroma (DF) is usually confined to the dermis and CASE REPORT the overlying epidermis is usually hyperplastic. Although DF with deep subcutaneous extension is commonly en- A 41-year-old male presented to our dermatology out- countered, purely subcutaneous DF is uncommon. In this patient clinic, with an apparently asymptomatic palpable review, we describe a case of a 41-year-old male patient who subcutaneous skin lesion on the left thigh, appearing 3 presented with a painless, subcutaneous, hard papule on the months prior to his visit to our clinic. There was no left thigh. After the skin had been incised the lesion was previous history of medication use or trauma and no totally removed, and histopathology revealed a subcu- family history of skin disease. The lesion was a hard, taneous dermatofibroma. (Ann Dermatol 23(2) 254∼257, solitary, discrete, subcutaneous papule. The lesion had not 2011) been increasing in size over the last 3 months. The hard subcutaneous papule popped out when an incision for -Keywords- biopsy was made into the skin above the lesion. Histologic Dermatofibroma, Fibrous histiocytoma, Subcutaneous findings showed a well-circumscribed, subcutaneous papule composed of fibrohistiocytic proliferation (Fig. 1A). Storiform arrangement of spindle cells, trapping normal INTRODUCTION collagen bundles at the periphery of the lesion were consistent with subcutaneous DF (Fig. -

Feline Fibrosarcoma and Sarcoid
Feline Fibrosarcoma and Sarcoid 803-808-7387 www.gracepets.com These notes are provided to help you understand the diagnosis or possible diagnosis of cancer in your pet. For general information on cancer in pets ask for our handout “What is Cancer”. Your veterinarian may suggest certain tests to help confirm or eliminate diagnosis, and to help assess treatment options and likely outcomes. Because individual situations and responses vary, and because cancers often behave unpredictably, science can only give us a guide. However, information and understanding for tumors in animals is improving all the time. We understand that this can be a very worrying time. We apologize for the need to use some technical language. If you have any questions please do not hesitate to ask us. What is this tumor? Fibrosarcoma is a tumor originating from the fibroblasts of the skin and subcutaneous connective tissue. The tumors vary in growth rate. They often recur locally although spread to other parts of the body (metastasis) is rare. The feline sarcoid is a subtype of tumor that is caused by a papilloma (wart) virus. What do we know about the cause? The reason why a particular pet may develop this, or any cancer, is not straightforward. Cancer is often seemingly the culmination of a series of circumstances that come together for the unfortunate individual. Cross Section of Skin & Hair Follicle Feline sarcoma retroviruses (recombinant forms of feline leukemia virus - FeLV) may initiate fibrosarcoma development in young cats and where there are multiple tumors in cats of more than five years of age.