Pediatric Soft Tissue Sarcomas David M
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mixed Hepatoblastoma in the Adult: Case Report and Review of the Literature
J Clin Pathol: first published as 10.1136/jcp.33.11.1058 on 1 November 1980. Downloaded from J Clin Pathol 1980;33:1058-1063 Mixed hepatoblastoma in the adult: case report and review of the literature RP HONAN AND MT HAQQANI From the Department of Pathology, Walton Hospital, Rice Lane, Liverpool L9 JAE, UK SUMMARY A case of mixed hepatoblastoma in a woman is described. A survey of the English literature reveals 13 cases acceptable as mixed hepatoblastoma; these have been described and published under a variety of names. Difficulties in nomenclature and the histology of these cases are discussed. Diagnosis depends on the identification of both malignant mesenchymal and malignant epithelial elements. The former include myxoid connective tissue resembling primitive mesenchyme and areas resembling adult fibrosarcoma. Mature fibrous tissue with calcification and bone for- mation may be seen. Epithelial areas show tissue resembling fetal liver, poorly differentiated epithelial cells, and/or areas of adenocarcinoma. The current view on histogenesis is also given. Most hepatoblastomas occur in children under the mixedtumour,6carcino-osteochondromyxosarcoma,5 copyright. age of 2 years.' Hepatoblastoma in adults is ex- and rhabdomyosarcohepatoma.7 tremely rare, and the prognosis is much worse than in the mixed hepatoblastoma of childhood. Case report The literature of mixed hepatoblastoma in adults has until recently been confused, and the true inci- CLINICAL PRESENTATION dence of the tumour obscured, owing to the various A Chinese woman aged 27 had been resident in names used by different authors to describe their England for eight years. She gave a history of cases. The commonest pseudonym is 'mixed malig- 18 months' intermittent right-sided chest pain http://jcp.bmj.com/ nant tumour',2-4 an ambivalent term which merely and upper abdominal discomfort. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

Radiation-Associated Synovial Sarcoma
Radiation-Associated Synovial Sarcoma: Clinicopathologic and Molecular Analysis of Two Cases Jean-François Egger, M.D., Jean-Michel Coindre, M.D., Jean Benhattar, Ph.D., Philippe Coucke, M.D., Louis Guillou, M.D. University Institute of Pathology (J-FE, JB, LG) and Department of Radiooncology, University Hospital (PC), Lausanne, Switzerland; Bergonié Institute and University of Bordeaux II (J-MC), Bordeaux, France region, or viscera (1, 2). SS bears the t(X;18) (SYT- Development of a soft-tissue sarcoma is an infre- SSX) reciprocal translocation that seems to be spe- quent but well-known long-term complication of cific for this tumor type and can be routinely de- radiotherapy. Malignant fibrous histiocytomas, ex- tected in paraffin-embedded tissue using the traskeletal osteosarcomas, fibrosarcomas, malig- reverse transcriptase–polymerase chain reaction nant peripheral nerve sheath tumors, and angiosar- (RT-PCR; 3–6). Radiation-associated sarcomas are comas are most frequently encountered. Radiation- an infrequent but well-known long-term complica- associated synovial sarcomas are exceptional. We tion of radiotherapy (7–16). They occur in about report the clinicopathologic, immunohistochemi- 1/1000 patients who have undergone radiation cal, and molecular features of two radiation- therapy (7–11). Radiation-associated sarcomas are associated synovial sarcomas. One tumor developed defined as sarcomas arising in a previously irradi- in a 42-year-old female 17 years after external irra- ated field after a latency period of Ն2 years (12). diation was given for breast carcinoma; the other They usually show a more aggressive clinical course occurred in a 34-year-old female who was irradiated associated with shortened patient survival as com- at the age of 7 years for a nonneoplastic condition of pared with sporadic sarcomas (9–12, 14). -

Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010)
DOI: 10.2478/v10163-012-0008-6 ACTA CHIRURGICA LATVIENSIS • 2011 (11) ORIGINAL ARTICLE Morphological and Immunohistochemical Characteristics of Surgically Removed Paediatric Renal Tumours in Latvia (1997–2010) Ivanda Franckeviča*,**, Regīna Kleina*, Ivars Melderis** *Riga Stradins University, Riga, Latvia **Children’s Clinical University Hospital, Riga, Latvia Summary Introduction. Paediatric renal tumours represent 7% of all childhood malignancies. The variable appearances of the tumours and their rarity make them especially challenging group of lesions for the paediatric pathologist. In Latvia diagnostics and treatment of childhood malignancies is concentrated in Children’s Clinical University Hospital. Microscopic evaluation of them is realised in Pathology office of this hospital. Aim of the study is to analyze morphologic spectrum of children kidney tumours in Latvia and to characterise them from modern positions with wide range of immunohistochemical markers using morphological material of Pathology bureau of Children’s Clinical University Hospital. Materials and methods. We have analyzed surgically removed primary renal tumours in Children Clinical University Hospital from the year 1997 till 2010. Samples were fixed in 10% formalin fluid, imbedded in paraffin and haematoxylin-eosin stained slides were re-examined. Immunohistochemical re-investigation was made in 65.91% of cases. For differential diagnostic purposes were used antibodies for the detection of bcl-2, CD34, EMA, actin, desmin, vimentin, CKAE1/AE3, CK7, Ki67, LCA, WT1, CD99, NSE, chromogranin, synaptophyzin, S100, myoglobin, miogenin, MyoD1 (DakoCytomation) and INI1 protein (Santa Cruz Biotechnology). Results. During the revised period there were diagnosed 44 renal tumours. Accordingly of morphological examination data neoplasms were divided: 1) nephroblastoma – 75%, 2) clear cell sarcoma – 2.27%, 3) rhabdoid tumour – 4.55%, 4) angiomyolipoma – 4.55%, 5) embrional rhabdomyosarcoma – 2.27%, 6) mesoblastic nephroma – 4.55%, 7) multicystic nephroma – 4.55%, 8) angiosarcoma – 2.27%. -

Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report
The Korean Journal of Pathology 2004; 38: 276-9 Dermatofibrosarcoma Protuberans of the Parotid Gland -A Case Report - Ok-Jun Lee∙David Y. Pi∙ Dermatofibrosarcoma protuberans (DFSP) typically presents during the early or mid-adult life, Daniel H. Jo∙Kyung-Ja Cho and the most common site of origin is the skin on the trunk and proximal extremities. DFSP of Sang Yoon Kim1∙Jae Y. Ro the parotid gland is extremely rare and only one case has been reported in the literature. We present here a case of a 30-year-old woman with DFSP occurring in the parotid gland, and we Departments of Pathology and discuss the differential diagnosis. The patient is alive and doing well one year after her operation. 1Otolaryngology, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea Received : January 27, 2004 Accepted : July 5, 2004 Corresponding Author Jae Y. Ro, M.D. Department of Pathology, University of Ulsan College of Medicine, Asan Medical Center, 388-1 Pungnap-dong, Songpa-gu, Seoul 138-736, Korea Tel: 02-3010-4550 Fax: 02-472-7898 E-mail: [email protected] Key Words : Dermatofibrosarcoma Protuberans-Parotid Gland Epithelial tumors make up the majority of salivary gland neo- CASE REPORT plasms, while mesenchymal tumors of this organ are uncommon. Dermatofibrosarcoma protuberans (DFSP) of the salivary gland A 30-year-old woman came to the Otolaryngology Clinic at is exremely rare and only one case has been reported in the parotid the Asan Medical Center with a 2-year history of a slowly enlarg- gland.1 ing mass inferior to the left angle of the mandible. -

About Soft Tissue Sarcoma Overview and Types
cancer.org | 1.800.227.2345 About Soft Tissue Sarcoma Overview and Types If you've been diagnosed with soft tissue sarcoma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is a Soft Tissue Sarcoma? Research and Statistics See the latest estimates for new cases of soft tissue sarcoma and deaths in the US and what research is currently being done. ● Key Statistics for Soft Tissue Sarcomas ● What's New in Soft Tissue Sarcoma Research? What Is a Soft Tissue Sarcoma? Cancer starts when cells start to grow out of control. Cells in nearly any part of the body can become cancer and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 There are many types of soft tissue tumors, and not all of them are cancerous. Many benign tumors are found in soft tissues. The word benign means they're not cancer. These tumors can't spread to other parts of the body. Some soft tissue tumors behave 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 in ways between a cancer and a non-cancer. These are called intermediate soft tissue tumors. When the word sarcoma is part of the name of a disease, it means the tumor is malignant (cancer).A sarcoma is a type of cancer that starts in tissues like bone or muscle. Bone and soft tissue sarcomas are the main types of sarcoma. Soft tissue sarcomas can develop in soft tissues like fat, muscle, nerves, fibrous tissues, blood vessels, or deep skin tissues. -

P05: Incidence Rates of Neoplasms by Anatomic Site (Systemic
TDMS No. 88123 - 07 P05: INCIDENCE RATES OF NEOPLASMS BY ANATOMIC SITE (SYSTEMIC Date Report Reqsted: 05/04/2006 LESIONS ABRIDGED) (a) Test Type: CHRONIC FORMAMIDE Time Report Reqsted: 11:47:08 Route: GAVAGE CAS Number: 75-12-7 First Dose M/F: 10/04/01 / 10/03/01 Species/Strain: MICE/B6C3F1 Pathologist: RYAN, M. - Blackshear, P. Lab: BAT F1_M3 C Number: C88123B Lock Date: 05/24/2004 Cage Range: ALL Date Range: ALL Reasons For Removal: ALL Removal Date Range: ALL Treatment Groups: Include ALL TDMS No. 88123 - 07 P05: INCIDENCE RATES OF NEOPLASMS BY ANATOMIC SITE (SYSTEMIC Date Report Reqsted: 05/04/2006 LESIONS ABRIDGED) (a) Test Type: CHRONIC FORMAMIDE Time Report Reqsted: 11:47:08 Route: GAVAGE CAS Number: 75-12-7 First Dose M/F: 10/04/01 / 10/03/01 Species/Strain: MICE/B6C3F1 Pathologist: RYAN, M. - Blackshear, P. Lab: BAT B6C3F1 MICE MALE 0 MG/KG 20 MG/KG 40 MG/KG 80 MG/KG Disposition Summary Animals Initially in Study 50 50 50 50 Early Deaths Moribund Sacrifice 4 8 6 14 Natural Death 7 8 3 Survivors Terminal Sacrifice 39 42 36 33 Animals Examined Microscopically 50 50 50 50 ALIMENTARY SYSTEM Esophagus (50) (50) (50) (50) Periesophageal Tissue, 1 (2%) Hepatocholangiocarcinoma, Metastatic, Liver Gallbladder (45) (48) (45) (46) Intestine Large, Cecum (50) (50) (50) (50) Intestine Large, Colon (50) (50) (50) (50) Intestine Large, Rectum (50) (50) (50) (50) Intestine Small, Duodenum (50) (50) (50) (50) Carcinoma, Metastatic, Pancreas 1 (2%) Intestine Small, Ileum (50) (50) (50) (50) Epithelium, Carcinoma 1 (2%) Intestine Small, Jejunum -
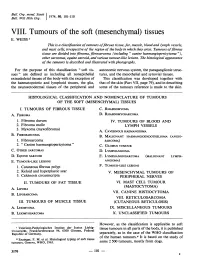
Mesenchymal) Tissues E
Bull. Org. mond. San 11974,) 50, 101-110 Bull. Wid Hith Org.j VIII. Tumours of the soft (mesenchymal) tissues E. WEISS 1 This is a classification oftumours offibrous tissue, fat, muscle, blood and lymph vessels, and mast cells, irrespective of the region of the body in which they arise. Tumours offibrous tissue are divided into fibroma, fibrosarcoma (including " canine haemangiopericytoma "), other sarcomas, equine sarcoid, and various tumour-like lesions. The histological appearance of the tamours is described and illustrated with photographs. For the purpose of this classification " soft tis- autonomic nervous system, the paraganglionic struc- sues" are defined as including all nonepithelial tures, and the mesothelial and synovial tissues. extraskeletal tissues of the body with the exception of This classification was developed together with the haematopoietic and lymphoid tissues, the glia, that of the skin (Part VII, page 79), and in describing the neuroectodermal tissues of the peripheral and some of the tumours reference is made to the skin. HISTOLOGICAL CLASSIFICATION AND NOMENCLATURE OF TUMOURS OF THE SOFT (MESENCHYMAL) TISSUES I. TUMOURS OF FIBROUS TISSUE C. RHABDOMYOMA A. FIBROMA D. RHABDOMYOSARCOMA 1. Fibroma durum IV. TUMOURS OF BLOOD AND 2. Fibroma molle LYMPH VESSELS 3. Myxoma (myxofibroma) A. CAVERNOUS HAEMANGIOMA B. FIBROSARCOMA B. MALIGNANT HAEMANGIOENDOTHELIOMA (ANGIO- 1. Fibrosarcoma SARCOMA) 2. " Canine haemangiopericytoma" C. GLOMUS TUMOUR C. OTHER SARCOMAS D. LYMPHANGIOMA D. EQUINE SARCOID E. LYMPHANGIOSARCOMA (MALIGNANT LYMPH- E. TUMOUR-LIKE LESIONS ANGIOMA) 1. Cutaneous fibrous polyp F. TUMOUR-LIKE LESIONS 2. Keloid and hyperplastic scar V. MESENCHYMAL TUMOURS OF 3. Calcinosis circumscripta PERIPHERAL NERVES II. TUMOURS OF FAT TISSUE VI. -

Undifferentiated Pleomorphic Sarcoma: Diagnosis of Exclusion
Published online: 2019-04-16 Case Report Undifferentiated pleomorphic sarcoma: Diagnosis of exclusion ABSTRACT Malignant soft‑tissue tumors which were designated as malignant fibrous histiocytoma are regrouped by the WHO (in 2002) under the new entity termed as “undifferentiated pleomorphic sarcoma.”[1] It accounts for less than 5% of all adult soft‑tissue sarcomas. Here, we report the lesion in a 70‑year‑old man who presented with high‑grade undifferentiated pleomorphic sarcoma in the lower extremity. Keywords: Adult soft‑tissue sarcomas, malignant fibrous histiocytoma, soft‑tissue sarcoma of lower extremity, undifferentiated pleomorphic sarcoma INTRODUCTION On gross inspection, soft‑tissue mass measured 12 cm × 5 cm × 4 cm, with tumor mass of about Undifferentiated pleomorphic sarcomas are aggressive 3 cm × 2 cm × 1 cm dimensions. tumors, commonly seen in adults. However histopathological pattern is very much variable in these soft tissue Cut section was gray brown with areas of necrosis in it malignant neoplasms. We detected this case where [Figure 1]. proper clinico‑histomorphological analysis coupled with immunohistochemistry (IHC) helped us to arrive at a Histopathological examination revealed a malignant tumor diagnosis. with pleomorphic bizarre cells. At places, spindled and tadpole like contour cells were seen. Many histiocytic giant CASE REPORT cells were also noted in the sections [Figure 2, 3]. The surgical margins were free of the tumor. A 70‑year‑old male presented with swelling over the posterior aspect of the left thigh. Swelling was gradually increasing Based on these microscopic findings and the site involved, in size. differentials of pleomorphic rhabdomyosarcoma and an undifferentiated pleomorphic sarcoma were kept. -
The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -

Pediatric Sarcomas
Pediatric Sarcomas a, b Regan F. Williams, MD *, Israel Fernandez-Pineda, MD , a Ankush Gosain, MD, PhD KEYWORDS Rhabdomyosarcoma Osteosarcoma Ewing’s sarcoma Nonrhabdomyosarcoma soft tissue sarcoma KEY POINTS Pediatric sarcomas are best treated with a multidisciplinary team to include surgery, radi- ation, and oncology. Rhabdomyosarcomas (RMS) often occur in young children, whereas nonrhabdomyosar- comas occur in infants and teenagers. All patients with RMS receive chemotherapy. Low-grade osteosarcomas and low risk nonrhabdomyosarcomas are treated with surgery alone. Pediatric sarcomas are a heterogeneous group of tumors and account for approxi- mately 10% of childhood solid tumors.1 Treatment is focused on multimodality ther- apy, which has improved the prognosis over the past 2 decades. Current regimens focus on decreasing treatment for low-risk patients to decrease the long-term side ef- fects of chemotherapy and radiation while maximizing therapy for patients with met- astatic disease in an attempt to improve survival. Pediatric sarcomas can be divided into soft tissue sarcomas and osseous tumors. Soft tissue sarcomas are further delineated into rhabdomyosarcoma (RMS), which affect young children and nonrhabdomyosarcoma, which are most common in adolescents. The most common bone sarcomas are osteosarcoma (OS) and Ewing sarcoma (ES). RHABDOMYOSARCOMA Epidemiology RMS is the most common soft tissue sarcoma in children and adolescents, accounting for nearly 250 cases of childhood cancer in the United States each year.2 RMS is a The authors have nothing to disclose. a Department of Surgery, University of Tennessee Health Science Center, 49 North Dunlap Avenue, Second Floor, Memphis, TN 38105, USA; b Department of Surgery, St Jude Children’s Research Hospital, MS133, Room B3019, 262 Danny Thomas Place, Memphis, TN 38105-3678, USA * Corresponding author. -

A Case of Dedifferentiated Leiomyosarcoma of the Uterus Kanae Nosaka1,2, Hiroaki Komatsu3, Tetsuro Oishi3, Yasushi Horie2, Tasuku Harada3 and Yoshihisa Umekita1*
Nosaka et al. Int J Pathol Clin Res 2016, 2:049 Volume 2 | Issue 4 International Journal of ISSN: 2469-5807 Pathology and Clinical Research Case Report: Open Access A Case of Dedifferentiated Leiomyosarcoma of the Uterus Kanae Nosaka1,2, Hiroaki Komatsu3, Tetsuro Oishi3, Yasushi Horie2, Tasuku Harada3 and Yoshihisa Umekita1* 1Division of Organ Pathology, Department of Pathology, Tottori University, Japan 2Division of Anatomic Pathology, Tottori University Hospital, Japan 3Division of Reproductive - Perinatal Medicine and Gynecologic Oncology, Department of surgery, Tottori University, Japan *Corresponding author: Yoshihisa Umekita, MD, PhD, Division of Organ Pathology, Department of Pathology, Faculty of Medicine, Tottori University, 86 Nishicho, Yonago, Tottori 683-8503, Japan, E-mail: [email protected] Abstract Case Report Dedifferentiation of leiomyosarcoma is a rare phenomenon that Clinical history associates pleomorphic histology and loss of smooth muscle differentiation. Although the leiomyosarcoma is well known A 63-year-old multiparous female presented with bloody vaginal sarcoma in the uterus, and the dedifferentiated leiomyosarcoma discharge lasting for 2 months. She had no particular medical history is well recognized in the soft parts, there are only a few reports except for the uterine leioimyoma discovered 13 years before. Her of dedifferentiation of leiomyosarcoma in the uterus. Herein we cervical cytology was negative while endometrial cytology detected present a case of dedifferentiated uterine leiomyosarcoma and atypical cells. There was no elevation of tumor markers (CEA and discuss its relation to the undifferentiated uterine sarcoma. CA19-9) in her serum. Hysteroscopy revealed a smooth-surfaced Keywords massive tumor occupying the uterine cavity. Abdominal MRI revealed 7.7 × 9.4 × 12.4 cm of round mass in the anterior uterine Uterine leiomyosarcoma, Dedifferentiation, Undifferentiated uterine corpus.