Principles for Best Practice in Clinical Audit
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

From the Factory to the Frontlines the Operation Warp Speed Strategy for Distributing a COVID-19 Vaccine
From the Factory to the Frontlines The Operation Warp Speed Strategy for Distributing a COVID-19 Vaccine What This Strategy Aims to Do This report to Congress details a strategy to achieve the principal purpose and objective of Operation Warp Speed (OWS): ensuring that every American who wants to receive a COVID-19 vaccine can receive one, by delivering safe and effective vaccine doses to the American people beginning January 2021. The leadership of OWS has committed to being transparent with Congress, the media, and the American people. OWS has provided regular briefings on topics of interest to Congress and the media and will continue to provide updates and announcements as OWS reaches new milestones. Congress has been a vital partner in the all-of-America response to the COVID-19 pandemic. With support provided through emergency supplemental and flexible discretionary funding, OWS has now made strong progress toward a safe and effective COVID-19 vaccine, with multiple candidates in Phase 3 clinical trials. Simultaneously, OWS and partners are developing a plan for delivering a safe and effective product to Americans as quickly and reliably as possible. Experts from the Department of Health and Human Services (HHS) are leading vaccine development, while experts from the Department of Defense (DoD) are partnering with the Centers for Disease Control and Prevention (CDC) and other parts of HHS to coordinate supply, production, and distribution of vaccines. Successful implementation of the national COVID-19 vaccination program requires precise coordination across federal, state, local, tribal, and territorial governments and among many public and private partners. -

List of Eligible Applicants and Estimated Funding Award Amounts by Category
Attachm nt A OOOTTT222111 ––– 222111 333::: NNNatatatiiiooonnnalalal IIInnniiitttiiiatatatiiivvveee tttooo AAAddddddrrreeessssss CCCOOOVVVIIIDDD---111999 HHHeeealalalttthhh DDDiiissspppararariiitttiiieeesss amamamooonnnggg PPPooopppuuulllatatatiiiooonnnsss atatat HHHiiiggghhh---RRRiiissskkk anananddd UUUnnndddeeerrrssseeerrrvvveeeddd,,, IIInnncccllluuudddiiinnnggg RRRacacaciiialalal anananddd EEEttthhhnnniiiccc MMMiiinnnooorrriiitttyyy PPPooopppuuulllatatatiiiooonnnsss anananddd RRRuuurrralalal CCCooommmmmmuuunnniiitttiiieeesss List of Eligible Applicants and Estimated Funding Award Amounts by Category State Estimated Awards Award ange $17,000,000 - $50,000,000 Award Average $32,000,000 Eligible Applicants Alabama D partm nt of Public H alth (ADPH) Alaska D partm nt of H alth and Social S rvic s - Division of Public H alth Arizona D partm nt of H alth S rvic s Arkansas D partm nt of H alth California D partm nt of Public H alth Colorado D partm nt of Public H alth and Environm nt Conn cticut D partm nt of Public H alth D lawar D partm nt of H alth and Social S rvic s- Division of Public H alth Florida D partm nt of H alth G orgia D partm nt of Public H alth Hawaii Stat D partm nt of H alth Idaho D partm nt of H alth and W lfar Illinois D partm nt of Public H alth Indiana D partm nt of H alth Iowa D partm nt of Public H alth Kansas D partm nt of H alth & Environm nt K ntucky D partm nt for Public H alth Louisiana D partm nt of H alth Main D partm nt of H alth and Human S rvic s Maryland D partm nt of H alth Massachus tts D partm nt of Public -

2011 State Profile — Palau
2011 State Profile — Palau National Survey of Substance Abuse Treatment Services (N-SSATS) The National Survey of Substance Abuse Treatment Services (N-SSATS) is an annual survey of facilities providing substance abuse treatment. It is conducted by the Substance Abuse and Mental Health Services Administration (SAMHSA). N-SSATS is designed to collect data on the location, characteristics, services offered, and number of clients in treatment at alcohol and drug abuse treatment facilities (both public and private) throughout the 50 States, the District of Columbia, and other U.S. jurisdictions. More information on N-SSATS methodology is available at the following URL: http://www.samhsa.gov/data/2k3/NSSATS/NSSATS.pdf In Palau, 1 substance abuse treatment facility was included in the 2011 N-SSATS, reporting that there were 105 clients in substance abuse treatment on March 31, 2011. The survey response rate in Palau was 100.0%. Facility Operation Clients in Treatment on March 31, 2011 Facilities All Clients Clients Under Age 18 No. % No. % No. % Private non-profit 0 0.0 0 0.0 0 0.0 Private for-profit 0 0.0 0 0.0 0 0.0 Local, county, or community government 1 100.0 105 100.0 10 100.0 State government 0 0.0 0 0.0 0 0.0 Federal government 0 0.0 0 0.0 0 0.0 Dept. of Veterans Affairs 0 0.0 0 0.0 0 0.0 Dept. of Defense 0 0.0 0 0.0 0 0.0 Indian Health Service 0 0.0 0 0.0 0 0.0 Other 0 0.0 0 0.0 0 0.0 Tribal government 0 0.0 0 0.0 0 0.0 Total 1 100.0 105 100.0 10 100.0 Primary Focus of Facility Clients in Treatment on March 31, 2011 Facilities All Clients Clients Under Age 18 No. -
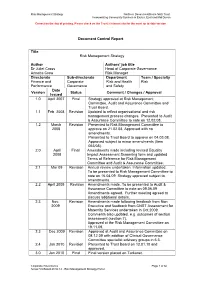
Risk Management Review
Risk Management Strategy Northern Devon Healthcare NHS Trust Incorporating Community Services in Exeter, East and Mid Devon Correct on the day of printing. Please check on the Trust’s internet site for the most up to date version Document Control Report Title Risk Management Strategy Author Authors’ job title Dr Juliet Cross Head of Corporate Governance Annette Crew Risk Manager Directorate Sub-directorate Department Team / Specialty Finance and Corporate Risk and Health Risk Performance Governance and Safety Date Version Status Comment / Changes / Approval Issued 1.0 April 2007 Final Strategy approved at Risk Management Committee, Audit and Assurance Committee and Trust Board. 1.1 Feb. 2008 Revision Updated to reflect organisational and risk management process changes. Presented to Audit & Assurance Committee to note on 12.02.08. 1.2 March Revision Presented to Risk Management Committee to 2008 approve on 21.02.08. Approved with no amendments. Presented to Trust Board to approve on 04.03.08. Approved subject to minor amendments (Item 053/08). 2.0 April Final Amendments made including revised Equality 2008 Impact Assessment Screening form and updated Terms of Reference for Risk Management Committee and Audit & Assurance Committee. 2.1 Mar 09 Revision Annual review undertaken. Information updated. To be presented to Risk Management Committee to note on 16.04.09. Strategy approved subject to amendments. 2.2 April 2009 Revision Amendments made. To be presented to Audit & Assurance Committee to note on 09.06.09 Amendments agreed. Further meeting agreed to discuss additional details. 2.3 Nov. Revision Amendments made following feedback from Non 2009 Executive and feedback from CNST Assessment for Maternity Services undertaken in Oct.2009. -

Deputy Health Officer
County of Monterey 14K54 DEPUTY HEALTH OFFICER DEFINITION Under general direction of the Health Officer, assists the Health Officer in the administration and medical oversight of public health programs for the County; provides health policy consultation on health and preventative medicine issues to the Health Officer, department staff, citizens, public officials, community organizations, agencies and staff; in the absence of the Health Officer, serves as the designated County Health Officer; and performs other related work as required DISTINGUISHING CHARACTERISTICS This single position management level class is responsible to the Health Officer for assisting in providing medical oversight, consultation and/or enforcement of public health regulations for a variety of public health programs and services, including environmental health, vital records, communicable disease control, preventative chronic and acute general medical services, public health nursing, emergency and disaster medical planning, public health education, California Children’s Service, and maternal and child health services. This position provides principal supervision of Vital Records, Health Assessment, Laboratory, and Epidemiology programs. This position is distinguished from the Health Officer in that the Health Officer is appointed by the County Board of Supervisors, directs medical oversight and policy for the County, and possesses the powers, duties, and responsibilities relating to the preservation and protection of public health. The Deputy Health Officer assists in directing the medical oversight and policy for the County, and does not carry full powers, duties and responsibilities relating to public health, but may act in the absence of the Health Officer. The Deputy Health Officer is distinguished from lower level management or physician classes in that the latter directs specific areas of program responsibility or medical practice, whereas the Deputy Health Officer assists in directing the medical oversight for all public health programs EXAMPLES OF DUTIES 1. -

Clinical Audit/Quality Improvement Projects Guidance for Professional
Clinical Audit/Quality Improvement Projects Guidance For Professional Competence Scheme Prepared by Faculty of Public Health Medicine December 2012 1 KEY POINTS ON AUDIT FOR PUBLIC HEALTH . This document is produced by the Faculty of Public Health Medicine Ireland (FPHMI) to support and guide participants of the FPHMI Professional Competence Scheme (PCS) to achieve their requirement of completing one clinical audit / quality improvement project each year. This document is a guide for doctors practising public health medicine and who are either on the Specialist or General Division of the Register . All doctors must participate in professional competence . Each doctor must define his/her scope of practice . All doctors whose practice include both clinical and non‐clinical work should engage in both clinical audit and other quality improvement practices relevant to their scope of practice . Audit can be at individual, team, departmental or national level . Each doctor must actively engage in clinical audit / systematic quality improvement activity that relates directly to their practice. ‘The Medical Council’s Framework for Maintenance of Professional Competence Activities’ sets one clinical audit per year as the minimum target. The time spent on completing the audit is accounted for separately from other Continuing Professional Development (CPD) activities. It is estimated that the completion of one clinical audit will take approximately 12 hours of activity. The main challenges in undertaking audit in public health practice include o Lack of explicit criteria against which to measure audit o Timeframes for measuring outcomes which can be prolonged and thus process measures are more readily measured Can’t seem to format this box which is smaller than the text o Changing public health work programmes in Departments . -

The High Achieving Governmental Health Department in 2020 As the Community Chief Health Strategist
The High Achieving Governmental Health Department in 2020 as the Community Chief Health Strategist Public Health Leadership Forum This paper was prepared by RESOLVE as part of the Public Health Leadership Forum with funding from the Robert Wood Johnson Foundation. John Auerbach, Director of Northeastern University’s Institute on Urban Health Research, also put substantial time and effort into authoring the document with our staff. The concepts put forth are based on several working group session (See Appendix B for members) and are not attributable to any one participant or his/her organization. May 2014 The High Achieving Governmental Health Department in 2020 as the Community Chief Health Strategist Public Health Leadership Forum Background Local and state health departments need to adapt and evolve if governmental public health is to address emerging health demands, minimize current as well as looming pitfalls, and take advantage of new and promising opportunities. To succeed requires a view into the future. This paper provides that vision. And, importantly, it zeroes in on what a high achieving public health department of the future will be doing differently. It does so not with a comprehensive inventory of tasks but rather with a distillation of the most important new skills and activities essential to be high achieving and serve in the role of the community chief health strategist. A working group of public health practitioners and policy experts was convened by RESOLVE as part of the Public Health Leadership Forum with funding from the Robert Wood Johnson Foundation (See Appendix B for a list of members). The working group purposely set a time frame of public health in 2020 – just six years into the future – in order to look far enough ahead to provide a compelling beacon, while staying close enough to the present to emphasize the urgency of taking immediate steps to start the process of change and build the leadership necessary to be successful. -
Onsite Guide
A HIA 3 8T H A N N U A L C O N F E R E N C E ONSITE GUIDE SPONSORED BY Scan to download the AHIA Conference App www.ahia.org TABLE OF CONTENTS AHIA MISSION & VISION AHIA Mission and Vision . 3 & VISION AHIA MISSION TABLE OF CONTENTS TABLE Hotel Floor Plan & Site Map . 4-5 Welcome . 5 Schedule of Events by Day . 6-15 AHIA Board of Directors & Conference MISSION STATEMENT Planning Committee . 17 The Association of Healthcare Internal Auditors provides leadership Exhibit Hall Hours & Social Events Schedule . 18-19 and advocacy to advance the healthcare internal audit profession AHIA Conference Tracks . 20-21 globally by facilitating relevant education, resources, certification 2020 Save the Date . 21 and networking opportunities. Conference Schedule Sunday, September 15 . 22-30 VISION STATEMENT Monday, September 16 . 31-44 To be the premier association for healthcare internal auditing. Tuesday, September 17 . 45-59 Founded in 1981, the Association of Healthcare Internal Auditors Wednesday, September 18 . 61-67 (AHIA) is a network of experienced healthcare internal auditing Sponsors . 68-69 professionals who come together to share tools, knowledge and Exhibitor Hours & Drawing . .. 70 insight on how to assess and evaluate risk within a complex and dynamic healthcare environment. AHIA is an advocate for the Exhibitor Floor Plan . 71 profession, continuing to elevate and champion the strategic Exhibitor Listing . 72-82 importance of healthcare internal auditors with executive CPE Certification . 85 management and the Board. If you have a stake in healthcare governance, risk management and internal controls, AHIA is CHIAP™ Certificants . 86–88 your one-stop resource. -

VDH (VBDPH) Mandated Services
VIRGINIA DEPARTMENT OF HEALTH (VDH) SUMMARY OF MANDATES REQUIRED BY FEDERAL LAW, STATE LAW, CONTRACT OR INTERAGENCY AGREEMENT Revised for Virginia Beach Department of Public Health March 2017 Note: The majority of Public Health Laws in the State of Virginia are found in Title 32 in the State Legislative Information System. Specific chapters of the law are referenced in the table below. 1. OVERARCHING AGENCY MISSION, CONTEXT AND STRUCTURE Mandated Service or Authority (and Obligating Description of Mandate or Authorizing Text Activity Instrument, if any): Establishment of the §§ 32.1-2, 32.1-16 There shall be a State Board of Health and a State Department of State Board of Health Health in the executive department responsible to the Secretary of and the State Health and Human Resources. Department of Health Purpose of the Board §32.1-2 The General Assembly finds that the protection, improvement and and Department preservation of the public health and of the environment are essential to the general welfare of the citizens of the Commonwealth. For this reason, the State Board of Health and the State Health Commissioner, assisted by the State Department of Health, shall administer and provide a comprehensive program of preventive, curative, restorative and environmental health services, educate the citizenry in health and environmental matters, develop and implement health resource plans, collect and preserve vital records and health statistics, assist in research, and abate hazards and nuisances to the health and to the environment, both emergency and otherwise, thereby improving the quality of life in the Commonwealth. Development of §32.1-11 The Board may formulate a program of environmental health, Programs laboratory services, and preventive, curative and restorative medical care services, including home and clinic health services. -

Clinical Audit: a Simple Guide for NHS Boards & Partners
Clinical audit: A simple guide for NHS Boards & partners Authors: Dr. John Bullivant, Director, Good Governance Institute (GGI) Good Governance Andrew Corbett-Nolan, Institute Chair, Institute of Healthcare Management (IHM) Contents Executive summary Executive summary 3 Whilst this guide is specifically about clinical audit, much of what • Delivers a return on investment. is described here is relevant to the way in which NHS Boards can • Improvements are implemented and sustained. 1. Clinical audit: Ten simple rules for NHS Boards 5 monitor clinical quality as a whole within the context of clinical or integrated governance. A PCT has specific responsibilities in relation to clinical audit that 2. Foreword 7 should be managed through the Professional Executive Clinical audit has been endorsed by the Department of Health in Committee (PEC) or an equivalent committee. 3. Clinical audit as part of the modern healthcare system 9 successive strategic documents as a significant way in which the quality of clinical care can be measured and improved. Originally, Boards should use clinical audit to confirm that current practice 4. Definitions and types of clinical quality review 11 clinical audit was developed as a process by which clinicians compares favourably with evidence of good practice and to reviewed their own practice. However, clinical audit is now 5. The importance and relationship of clinical audit to clinical ensure that where this is not the case that changes are made recognised as an effective mechanism for improving the quality that improve the delivery of care. governance, NHS Boards and their partner organisations 15 of care patients receive as a whole. -

Principles of Surgical Audit
Principles of I Surgical Audit How to Set Up a Prospective 1 Surgical Audit Andrew Sinclair and Ben Bridgewater Key points • Clinical audit can be prospective and/or • A clinical department benefits from a clear audit retrospective. plan. • Audit information can be obtained from • Clinical audit improves patient outcome. national, hospital, and surgeon-specific data. Much of the experience we draw on comes from cardiac Introduction surgery, where there is a long history of structured data collection, both in the United States and in the United Clinical audit is one of the “keystones” of clinical govern- Kingdom. This was initially driven by clinicians [1–3,5], ance. A surgical department that subjects itself to regu- but more recently has been influenced by politicians and lar and comprehensive audit should be able to provide the media [6,7]. Cardiac surgery is regarded as an easy data to current and prospective patients about the qual- specialty to audit in view of the high volume and pro- ity of the services it provides, as well as reassurance to portion of a single operation coronary artery bypass those who pay for and regulate health care. Well-organ- graft (CABG) in most surgeons practice set against a ized audit should also enable the clinicians providing small but significant hard measurement end point of services to continually improve the quality of care they mortality (which is typically approximately 2%). deliver. There are many similarities between audit and research, but historically audit has often been seen as the “poor relation.” For audit to be meaningful and useful, it Why conduct prospective audit? must, like research, be methodologically robust and have sufficient “power” to make useful observations; it would There are a number of reasons why clinicians might be easy to gain false reassurance about the quality of care decide to conduct a clinical audit as given in Table 1.1. -
Toolkit to Develop and Strengthen Medical Audit Systems
Toolkit to Develop and Strengthen Medical Audit Systems Practical Guide by Implementers for Implementers December 2017 2017 심사평 메뉴얼북 표지.indd 2 17. 11. 29. 오후 8:26 2017 심사평 메뉴얼북 표지.indd 3 17. 11. 29. 오후 8:26 Toolkit to Develop and Strengthen Medical Audit Systems Practical Guide by Implementers for Implementers December 2017 2017 심사평 메뉴얼북 내지 책.indb 1 17. 11. 29. 오후 8:39 THIS GUIDE WAS PRODUCED by the Joint Learning Network for Universal Health Coverage (JLN), an innovative network of practitioners and policymakers from around the globe who engage in practitioner-to-practitioner learning and collaboratively develop practical tools to help countries work toward universal health coverage. For inquiries about this guide or other related JLN activities, please contact the JLN at [email protected]. This work was funded by a grant from the Rockefeller Foundation and by the Government of South Korea. The views expressed herein are solely those of the authors and do not necessarily reflect the views of the organizations. Note: This is the first release of the Medical Audits Toolkit. The toolkit has been reviewed by the participants of JLN’s Medical Audits collaborative, under which the product was developed. Attempts have been made to have the toolkit reviewed by external experts, such as medical audit professionals. A more rigorous review by external experts, along with feedback from countries will be incorporated to make it a comprehensive guide for use by countries looking to strengthen their medical audit systems. Revised version(s) of the toolkit will be available at www.jointlearningnetwork.org.