A Case of Pediatric Ectopia Lentis: Systemic of Etiologies for This Condition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Infantile Aphakia and Successful Fitting of Pediatric Contact Lenses; a Case Presentation Authors: Virji N, Patel A, Libassi D
Infantile aphakia and successful fitting of pediatric contact lenses; a case presentation Authors: Virji N, Patel A, Libassi D An eleven month old male presents with bilateral aphakia secondary to congenital cataracts. The patient is currently successfully wearing B&L Silsoft Pediatric contact lenses, with good prognosis for vision in both eyes. I. Case History -Patient demographics: African American male, DOB 8/18/2009 -Chief complaint: patient presents with bilateral aphakia secondary to bilateral congenital cataract extraction -Ocular, medical history: S/P CE with anterior vitrectomy OD 09/22/2009, followed by OS 09/29/09. (+) squinting, rubs eyes, light sensitivity -Medications: none -Other salient information: patient has been seen by SUNY Contact Lens clinic since 2 months old, 10/14/2009 II. Pertinent findings -Clinical: Keratometry readings 41.00/41.25 @ 005 OD, 38.50/41.00 @ 046 Axial length, immeasurable Horizontal corneal diameter 8mm OD/OS Fundus exam WNL OU -Others: surgical dates: successful CE OU, September 2009 III. Differential diagnosis -Primary/leading: Idiopathic -Others: Posterior lenticonus, persistent hyperplastic primary vitreous, anterior segment dysgenesis, and posterior pole tumors, trauma, intrauterine infection (rubella), maternal hypoglycemia, trisomy (eg, Down, Edward, and Patau syndromes), myotonic dystrophy, infectious diseases (eg, toxoplasmosis, rubella, cytomegalovirus, and herpes simplex [TORCH]), and prematurity. (5) IV. Diagnosis and discussion -Elaborate on the condition: Bilateral infantile cataracts are one of the major treatable causes of visual impairment in children. (2) Hubel and Weisel’s research on the critical period of visual development determined that if infantile cataracts are removed within the critical period and appropriate correction is worn, vision is greatly improved. -
Intraocular Lenses and Spectacle Correction
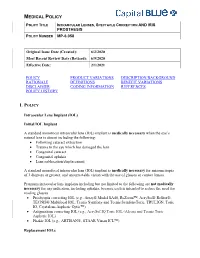
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

Megalocornea Jeffrey Welder and Thomas a Oetting, MS, MD September 18, 2010
Megalocornea Jeffrey Welder and Thomas A Oetting, MS, MD September 18, 2010 Chief Complaint: Visual disturbance when changing positions. History of Present Illness: A 60-year-old man with a history of simple megalocornea presented to the Iowa City Veterans Administration Healthcare System eye clinic reporting visual disturbance while changing head position for several months. He noticed that his vision worsened with his head bent down. He previously had cataract surgery with an iris-sutured IOL due to the large size of his eye, which did not allow for placement of an anterior chamber intraocular lens (ACIOL) or scleral-fixated lens. Past Medical History: Megalocornea Medications: None Family History: No known history of megalocornea Social History: None contributory Ocular Exam: • Visual Acuity (with correction): • OD 20/100 (cause unknown) • OS 20/20 (with upright head position) • IOP: 18mmHg OD, 17mmHg OS • External Exam: normal OU • Pupils: No anisocoria and no relative afferent pupillary defect • Motility: Full OU. • Slit lamp exam: megalocornea (>13 mm in diameter) and with anterior mosaic dystrophy. Iris-sutured posterior chamber IOLs (PCIOLs), stable OD, but pseudophacodonesis OS with loose inferior suture evident. • Dilated funduscopic exam: Normal OU Clinical Course: The patient’s iris-sutured IOL had become loose (tilted and de-centered) in his large anterior chamber, despite several sutures that had been placed in the past, resulting now in visual disturbance with movement. FDA and IRB approval was obtained to place an Artisan iris-clip IOL (Ophtec®). He was taken to the OR where his existing IOL was removed using Duet forceps and scissors. The Artisan IOL was placed using enclavation iris forceps. -

Recessive Buphthalmos in the Rabbit' Rochon-Duvigneaud
RECESSIVE BUPHTHALMOS IN THE RABBIT’ BERTRAM L. HANNA,2 PAUL B. SAWIN3 AND L. BENJAMIN SHEPPARD4 Received September 8, 1961 BUPHTHALMOS (hydrophthalmos, congenital infantile glaucoma) in rabbits has been of interest to European geneticists but has attracted little attention in the United States despite its recurrent appearance in laboratory and commercial breeding stocks. This condition is of particular interest to the field of expen- mental ophthalmology because of its similarity to congenital glaucoma in hu- mans. The earliest report of rabbit buphthalmos appears to be that of SCHLOESSER (1886), who presented the detailed histopathology of the left eye of a brown rab- bit which developed an acute glaucoma following irritation of both corneas to induce traumatic cataract. Other single case reports are by PICHLER(1910), ROCHON-DUVIGNEAUD(1921) and BECKH(1935), although in the last case the buphthalmos may have been secondary to a yaws infection. VOGT(1919), re- ported the occurrence of buphthalmos bilaterally in three siblings purchased at nine months of age. A mating between two of these produced a litter of three, all of which developed high grade buphthalmos. NACHTSHEIM(1937) and GERI (1954, 1955) studied the inheritance of buphthalmos and concluded that it is transmitted as an autosomal recessive trait. FRANCESCHETTI(1930) noted a de- ficiency of affected offspring from matings of heterozygous carrier parents. GERI (1955) found 12.5 percent affected offspring from carrier matings and suggested that the deficiency results from fetal death of buphthalmic animals. MCMASTER (1960) reported a mating of two animals with bilateral buphthalmos which pro- duced a litter of seven, only four of which were affected. -

Insertion of Aqueous Shunt in Pedicatric Glaucoma
1/29/2018 Challenges of Insertion of Aqueous shunt in paediatric glaucoma Ahmed Elkarmouty MD, FRCS Moorfields Eye Hospital London, UK Classification • Primary Childhood Glaucoma • A- Primary Congenital Glaucoma (PCG) 1: 10,000–18,000 • B- Juvenile Open Angle Glaucoma (JOAG) (5-35 ys,)1 : 50,000. • Secondary Childhood Glaucoma • A- Glaucoma associated with non-acquired ocular anomalies • B- Glaucoma associated with non- acquired systemic disease or syndrome • C- Glaucoma associated with acquired condition • D- Glaucoma following Cataract surgery 1 1/29/2018 Glaucoma associated with non- acquired ocular anomalies • Conditions with predominantly ocular anomalies present at birth which may or may not be associated with systemic signs • Axenfeld Reiger anomaly • Peters anomaly • Ectropion Uvae • Congenital iris hypolplasia • Aniridia • Oculodermal melanocytosis • Posterior polymorphous dystrophy • Microphthalmos • Microcornea • Ectopia Lentis ( et pupillae) • Persistent foetus vasculopathy Glaucoma associated with non- acquired systemic disease or syndrome predominantly associated with known syndrome, systemic anomalies present at birth which may be associated with ocular signs • Down Syndrome • Connective tissue disorder: Marfan syndrome, Weill- Marchesiani syndrome, Stickler syndrome • Metabolic disorder : Homocystenuria, lowe syndrome, Mucoploysacchroidoses • Phacomatoses: Neurofibromatoses, Sturge Weber, Klipple-Trenaunay- weber syndrome, Rubenstein Taybi • Congenital Rubella 2 1/29/2018 Glaucoma associated with acquired condition Conditions -

Solved/Unsolved
Supplementary Materials: Supplementary table 1. Demographic details for the 54 individual patients (solved/unsolved) and their clinical features including cataract type, details of ocular co-morbidities, systemic features and whether cataract was the presenting feature (non-isolated cataract patients only). Abbreviations: yes (Y), no (N), not applicable (N/A). Age at Famil Ag M/ Age at Cataract Cataract Cataract Systemic Consanguinit Patient ID Gene Confirmed genetic diagnosis Ethnicity diagnosi Ocular co-morbidities FH y ID e F surgery type RE type LE presenting sign features y s (days) Aniridia, nystagmus, 23 years Posterior Posterior 1-1 1 PAX6 Aniridia White British 25 F - glaucoma, foveal N N N Y 4 months subcapsular subcapsular hypoplasia Cleft palate, epilepsy, high Aphakia Aphakia Macular atrophy, myopia, 7 years 9 7 years 8 arched palate, 2-1 2 COL11A1 Stickler syndrome, type II Not Stated 34 F (post- (post- lens subluxation, vitreous N N N months months flattened surgical) surgical) anomaly maxilla, short stature (5'2ft) Anterior segment dysgenesis, pupillary abnormalities including 12 years Posterior Posterior ectopic pupils, ectropion 3-1 3 CPAMD8 Anterior segment dysgenesis 8 Other, Any other 27 F - N N Y N 5 months subcapsular subcapsular UVAE and irodensis, nystagmus, dysplastic optic discs, large corneal diameters Gyrate atrophy of choroid and 23 years 29 years 1 Posterior Posterior Retinal dystrophy, Bipolar 4-1 4 OAT White British 42 F N N N retina 7 months month subcapsular subcapsular exotropia disorder 1 year 6 1 year -

Feasibility and Outcome of Descemet Membrane Endothelial Keratoplasty in Complex Anterior Segment and Vitreous Disease
CLINICAL SCIENCE Feasibility and Outcome of Descemet Membrane Endothelial Keratoplasty in Complex Anterior Segment and Vitreous Disease Julia M. Weller, MD, Theofilos Tourtas, MD, and Friedrich E. Kruse, MD escemet membrane endothelial keratoplasty (DMEK), Purpose: Descemet membrane endothelial keratoplasty (DMEK) is Da technique for posterior lamellar keratoplasty, involves becoming the method of choice for treating Fuchs endothelial a graft consisting only of the thin Descemet membrane with dystrophy and pseudophakic bullous keratopathy. We investigated adherent corneal endothelial cells. Introduced in 2006 by whether DMEK can serve as a routine procedure in endothelial Melles et al,1 DMEK is becoming more popular as several decompensation even in complex preoperative situations. studies show its superiority to Descemet stripping automated Methods: Of a total of 1184 DMEK surgeries, 24 consecutive eyes endothelial keratoplasty (DSAEK), regarding visual function 2,3 with endothelial decompensation and complex preoperative situa- and the time of visual rehabilitation after DMEK. However, tions were retrospectively analyzed and divided into 5 groups: group because DMEK grafts are thinner than DSAEK grafts, it is fi 1: irido-corneo-endothelial syndrome (n = 3), group 2: aphakia, more dif cult to handle them and typically takes surgeons subluxated posterior chamber intraocular lens or anterior chamber longer to learn. intraocular lens (n = 6), group 3: DMEK after trabeculectomy (n = In difficult situations, most surgeons prefer DSAEK or 4), group 4: DMEK with simultaneous intravitreal injection (n = 6), penetrating keratoplasty to DMEK because of its possible and group 5: DMEK after vitrectomy (n = 5). Main outcome intraoperative complications. For example, if corneal edema 4 parameters were best-corrected visual acuity, central corneal thick- is advanced, Ham et al recommend performing DSAEK first ness, endothelial cell density, rebubbling rate, and graft failure rate. -

Glaucoma-Related Adverse Events in the Infant Aphakia Treatment Study 1-Year Results
CLINICAL SCIENCES ONLINE FIRST Glaucoma-Related Adverse Events in the Infant Aphakia Treatment Study 1-Year Results Allen D. Beck, MD; Sharon F. Freedman, MD; Michael J. Lynn, MS; Erick Bothun, MD; Daniel E. Neely, MD; Scott R. Lambert, MD; for the Infant Aphakia Treatment Study Group Objectives: To report the incidence of glaucoma and glau- sistent fetal vasculature and 1.6 times higher for each coma suspects in the IATS, and to evaluate risk factors for month of age younger at cataract surgery. the development of a glaucoma-related adverse event in patients in the IATS in the first year of follow-up. Conclusions: Modern surgical techniques do not elimi- nate the early development of glaucoma following con- Methods: A total of 114 infants between 1 and 6 months genital cataract surgery with or without an intraocular of age with a unilateral congenital cataract were as- lens implant. Younger patients with or without persis- signed to undergo cataract surgery either with or with- tent fetal vasculature seem more likely to develop a glau- out an intraocular lens implant. Standardized defini- coma-related adverse event in the first year of follow- tions of glaucoma and glaucoma suspect were created and up. Vigilance for the early development of glaucoma is used in the IATS. needed following congenital cataract surgery, especially when surgery is performed during early infancy or for a Results: Of these 114 patients, 10 (9%) developed glau- child with persistent fetal vasculature. Five-year fol- coma and 4 (4%) had glaucoma suspect, for a total of 14 low-up data for the IATS will likely reveal more glaucoma- patients (12%) with a glaucoma-related adverse event in related adverse events. -

Visual Management of Aphakia with Concomitant Severe Corneal Irregularity by Mini-Scleral Design Contact Lenses
HOSTED BY Available online at www.sciencedirect.com ScienceDirect Journal of Current Ophthalmology 28 (2016) 27e31 http://www.journals.elsevier.com/journal-of-current-ophthalmology Original research Visual management of aphakia with concomitant severe corneal irregularity by mini-scleral design contact lenses Fateme Alipur, Seyedeh Simindokht Hosseini* Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran Received 30 October 2015; accepted 28 January 2016 Available online 30 March 2016 Abstract Purpose: To evaluate visual results, comfort of use, safety, and efficacy of mini scleral contact lenses in optical management in patients with traumatic aphakia and severe concomitant irido-corneal injury. Methods: In a case series, eight eyes with post traumatic aphakia and severe concomitant irido-corneal injury that were evaluated at the Contact Lens Clinic of Farabi Eye Hospital, Tehran, Iran for contact lens fitting and could not be corrected with conventional corneal RGP contact lenses were fitted with miniscleral contact lenses. Uncorrected visual acuity (UCVA), best spectacle corrected visual acuity (BSCVA), and BCVA (Best corrected visual acuity) with miniscleral lens were recorded. Slit lamp examination, comfortable daily wearing time, and any contact lens-related complication were documented in each follow-up visit. Results: The mean UCVA and BSCVA of the cases was >2.7 and 0.41 LogMAR, respectively (BSCVA could not be assessed in one case due to severe corneal irregularity). The mean final BCVA with the miniscleral lens was 0.05 LogMAR (range from 0.4 to À0.04 LogMAR). The mean follow-up period was 14.6 months. The mean comfortable daily wearing time (CDWT) was 11.6 h, ranging from 8 to 16 h. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

Abnormalities Affecting the Eye As a Whole 2 8 Congenital Corneal
I Editors vi Contributors vii , About the Series viii Preface ix ) Acknowledgments x -t -t Abnormalities Affecting the Eye as a Whole 2 Judith B. Lavrich Anophthalmia 2 Microphthalmia 8 Nanophthaha 12 Typical Coloboma 14 8 Congenital Corneal Opacity 18 Bruce SchnalI and Michael J. Bartiss Sderocornea 18 Birth Trauma: Tears in Descemet's Membrane 20 Ulcer or Lnfection 22 Mucopolysaccharidosis 24 Peters' Anomaly 26 Congenital Hereditary Endothelial Dystrophy 28 Corneal Dermoid 30 Anterior Staphyloma 32 Wilson's Disease (HepatolenticularDegeneration) 34 Herpes Simplex Infection 36 Herpes Simplex Virus Epithelial Dendrite or Ulceration 38 Herpes SimplexVirus Corneal Stromal Disease 40 Herpes Zoster Ophthalmicus 42 Chickenpox 44 Limbal Vernal Keratoconjunctivitis 46 C-3 Glaucoma 48 A& Levin and Anya A. Trumler Primary Congenital or Infantile Glaucoma 48 Juvenile Open-Angle Glaucoma 52 Aphakic Glaucoma 55 Uveitic Glaucoma 58 Sturge-WeberSyndrome 62 m xii CONTENTS Congenital Ectropion Uveae 65 Aniridia 68 Posterior Embryotoxon 70 C- C- 4 Iris Anomalies 72 Michael J.Bartiss and BruceM. Schall Central Pupillary Cysts (Pupillary Margin Epithelial Cysts) 72 Aniridia 74 BrusbJield Spots 76 Ectopia Lentis et Pupillae 78 Heterochromia Iridis 80 Iris Coloboma 82 Iris Stromal Cysts 84 Juvenile Xanthogranuloma 86 Lisch Nodules 88 Melanosis Oculi (Ocular Melanocytosis) 90 Persistent Pupillary Membrane 92 Posterior Synechiae 94 Axenfeld-Rieger Anomaly 96 -5 Lens Anomalies 98 Jonathan H. Salvin and Hillary Gordon Congenital and Developmental Cataracts 98 Ectopia Lentis 102 Anterior Lenticonus 104 Posterior Lenticonus 106 Spherophakia 108 C- 6 Retinal Anomalies 110 Barry N. Wasserman,Anuradha Ganesh, Alex V Levin, Carol L. Shields, Jerry A. Shields, and Alok S. -

An Operation for Congenital Ptosis by George Young
Br J Ophthalmol: first published as 10.1136/bjo.8.6.272 on 1 June 1924. Downloaded from 272 THE BRITISH JOURNAL OF OPHTHALMIOI,OGY added plus lenses (eye being under atropin), J.2, fluently. This made her left eye equal, for distance, to her better eye, which is now getting worse owing to increased bulging, and will probably follow the course of the other one soon. R.V.: 6/36, c. -1.OD sph. + 3.50D cyl. 1550: 6/24 and J.5. Furthermore, it may be noted that the intraocular tension was now normal on the side of the iridectomy, while the right eye was hard, and I submitted it again to pilocarpin and bandage at night. I sent her home for a fortnight to feed up, take malt and cod liver oil and fats, and to take plenty of rest and recuperate. On July 8 the final result was: L.V.: 6/36, c.-5.OD sph. +3.50D cyl. 1600: 6/12 full, and -3.OD sph. and +3.50D cyl. J.2. Soon I shall tattoo the stellate leucoma with an artificial pupil. May 10, 1924. Since writing the above, some ten months ago, affairs have kept steady. There is no bulging of the left cornea or scar. I attempted tattooing at two sittings, and have considerably diminished the glare of the scar, but I refrain from risking the deep tattooing necessary for securing an imitation round black pupil, fearing to do harm. Glasses were prescribed and worn with comfort and great help, the vision being maintained as above.