Fas Ligand Against Phagocytes Cutting Edge: Chemotactic Activity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Critical Contribution of OX40 Ligand to T Helper Cell Type 2
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Brief Definitive Report Critical Contribution of OX40 Ligand to T Helper Cell Type 2 Differentiation in Experimental Leishmaniasis By Hisaya Akiba,*§ Yasushi Miyahira,‡ Machiko Atsuta,*§ Kazuyoshi Takeda,*§ Chiyoko Nohara,* Toshiro Futagawa,* Hironori Matsuda,* Takashi Aoki,‡ Hideo Yagita,*§ and Ko Okumura*§ From the *Department of Immunology and the ‡Department of Parasitology, Juntendo University School of Medicine, Tokyo 113-8421, Japan; and §CREST (Core Research for Evolutional Science and Technology) of Japan Science and Technology Corporation, Tokyo 101-0062, Japan Abstract Infection of inbred mouse strains with Leishmania major is a well characterized model for analy- sis of T helper (Th)1 and Th2 cell development in vivo. In this study, to address the role of co- stimulatory molecules CD27, CD30, 4-1BB, and OX40, which belong to the tumor necrosis factor receptor superfamily, in the development of Th1 and Th2 cells in vivo, we administered monoclonal antibody (mAb) against their ligands, CD70, CD30 ligand (L), 4-1BBL, and OX40L, to mice infected with L. major. Whereas anti-CD70, anti-CD30L, and anti–4-1BBL mAb ex- hibited no effect in either susceptible BALB/c or resistant C57BL/6 mice, the administration of anti-OX40L mAb abrogated progressive disease in BALB/c mice. Flow cytometric analysis indicated that OX40 was expressed on CD41 T cells and OX40L was expressed on CD11c1 dendritic cells in the popliteal lymph nodes of L. major–infected BALB/c mice. In vitro stimu- lation of these CD41 T cells showed that anti-OX40L mAb treatment resulted in substantially reduced production of Th2 cytokines. -

Belongs to the TNF Family a New Class of Reverse Signaling
A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink This information is current as J Immunol 2007; 179:4307-4312; ; of September 27, 2021. doi: 10.4049/jimmunol.179.7.4307 http://www.jimmunol.org/content/179/7/4307 References This article cites 85 articles, 38 of which you can access for free at: Downloaded from http://www.jimmunol.org/content/179/7/4307.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision http://www.jimmunol.org/ • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: by guest on September 27, 2021 http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. THE JOURNAL OF IMMUNOLOGY BRIEF REVIEWS A New Class of Reverse Signaling Costimulators Belongs to the TNF Family Mingyi Sun and Pamela J. Fink1 Recent evidence shows that many molecules of the TNF still remains unclear (7). The N-terminal cytoplasmic domains family serve as counter-receptors, inducing costimulation of most TNF family members are conserved across species but through reverse signals in addition to delivering signals not between family members, suggesting that the intracellular through their respective TNF receptors. -

Immunity in the Developing Lung Foxa2 Programs Th2 Cell-Mediated
Foxa2 Programs Th2 Cell-Mediated Innate Immunity in the Developing Lung Gang Chen, Huajing Wan, Fengming Luo, Liqian Zhang, Yan Xu, Ian Lewkowich, Marsha Wills-Karp and Jeffrey A. This information is current as Whitsett of September 27, 2021. J Immunol 2010; 184:6133-6141; Prepublished online 5 May 2010; doi: 10.4049/jimmunol.1000223 http://www.jimmunol.org/content/184/11/6133 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2010/05/05/jimmunol.100022 Material 3.DC1 http://www.jimmunol.org/ References This article cites 59 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/184/11/6133.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 27, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Foxa2 Programs Th2 Cell-Mediated Innate Immunity in the Developing Lung Gang Chen,* Huajing Wan,† Fengming Luo,‡ Liqian Zhang,* Yan Xu,* Ian Lewkowich,x Marsha Wills-Karp,x and Jeffrey A. -

CD154-Independent Rejection Critical Role of OX40 in CD28
Critical Role of OX40 in CD28 and CD154-Independent Rejection Gülçin Demirci, Farhana Amanullah, Reshma Kewalaramani, Hideo Yagita, Terry B. Strom, Mohamed H. This information is current as Sayegh and Xian Chang Li of October 1, 2021. J Immunol 2004; 172:1691-1698; ; doi: 10.4049/jimmunol.172.3.1691 http://www.jimmunol.org/content/172/3/1691 Downloaded from References This article cites 42 articles, 23 of which you can access for free at: http://www.jimmunol.org/content/172/3/1691.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on October 1, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2004 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Critical Role of OX40 in CD28 and CD154-Independent Rejection1 Gu¨lc¸in Demirci,* Farhana Amanullah,* Reshma Kewalaramani,† Hideo Yagita,‡ Terry B. Strom,* Mohamed H. Sayegh,† and Xian Chang Li*2 Blocking both CD28 and CD154 costimulatory pathways can induce transplant tolerance in some, but not all, transplant models. -

Cells by OX40 Ligand and CD70 on Activated B CD28-Independent
CD28-Independent Costimulation of T Cells by OX40 Ligand and CD70 on Activated B Cells1 Hisaya Akiba,*† Hideo Oshima,*‡ Kazuyoshi Takeda,*† Machiko Atsuta,*† Hiroyasu Nakano,*† Atsuo Nakajima,§ Chiyoko Nohara,* Hideo Yagita,*† and Ko Okumura2*† OX40 and its ligand (OX40L) have been implicated in T cell-dependent humoral immune responses. To further characterize the role of OX40/OX40L in T-B cell interaction, we newly generated an anti-mouse OX40L mAb (RM134L) that can inhibit the costimulatory activity of OX40L transfectants for anti-CD3-stimulated T cell proliferation. Flow cytometric analyses using RM134L and an anti-mouse OX40 mAb indicated that OX40 was inducible on splenic T cells by stimulation with immobilized anti-CD3 mAb in a CD28-independent manner, while OX40L was not expressed on resting or activated T cells. OX40L was inducible on splenic B cells by stimulation with anti-IgM Ab plus anti-CD40 mAb, but not by either alone. These activated B cells exhibited a potent costimulatory activity for anti-CD3-stimulated T cell proliferation and IL-2 production. Anti-CD80 and anti- CD86 mAbs partially inhibited the costimulatory activity, and further inhibition was obtained by their combination with RM134L and/or anti-CD70 mAb. We also found the anti-IgM Ab- plus anti-CD40 mAb-stimulated B cells exhibited a potent costimulatory activity for proliferation of and IL-2 production by anti-CD3-stimulated CD282 T cells from CD28-deficient mice, which was substantially inhibited by RM134L and/or anti-CD70 mAb. These results indicated that OX40L and CD70 expressed on surface Ig- and CD40-stimulated B cells can provide CD28-independent costimulatory signals to T cells. -

Characterisation of Chicken OX40 and OX40L
Characterisation of chicken OX40 and OX40L von Stephanie Hanna Katharina Scherer Inaugural-Dissertation zur Erlangung der Doktorw¨urde der Tier¨arztlichenFakult¨at der Ludwig-Maximilians-Universit¨atM¨unchen Characterisation of chicken OX40 and OX40L von Stephanie Hanna Katharina Scherer aus Baunach bei Bamberg M¨unchen2018 Aus dem Veterin¨arwissenschaftlichenDepartment der Tier¨arztlichenFakult¨at der Ludwig-Maximilians-Universit¨atM¨unchen Lehrstuhl f¨urPhysiologie Arbeit angefertigt unter der Leitung von Univ.-Prof. Dr. Thomas G¨obel Gedruckt mit Genehmigung der Tier¨arztlichenFakult¨at der Ludwig-Maximilians-Universit¨atM¨unchen Dekan: Univ.-Prof. Dr. Reinhard K. Straubinger, Ph.D. Berichterstatter: Univ.-Prof. Dr. Thomas G¨obel Korreferenten: Priv.-Doz. Dr. Nadja Herbach Univ.-Prof. Dr. Bernhard Aigner Prof. Dr. Herbert Kaltner Univ.-Prof. Dr. R¨udiger Wanke Tag der Promotion: 27. Juli 2018 Meinen Eltern und Großeltern Contents List of Figures 11 Abbreviations 13 1 Introduction 17 2 Fundamentals 19 2.1 T cell activation . 19 2.1.1 The activation of T cells requires the presence of several signals 19 2.1.2 Costimulatory signals transmitted via members of the im- munoglobulin superfamily . 22 2.1.3 Costimulatory signals transmitted via members of the cy- tokine receptor family . 23 2.1.4 Costimulatory signals transmitted via members of the tumour necrosis factor receptor superfamily . 24 2.2 The tumour necrosis factor receptor superfamily . 26 2.2.1 The structure of tumour necrosis factor receptors . 26 2.2.2 Functional classification of TNFRSF members . 28 2.3 The tumour necrosis factor superfamily . 29 2.3.1 The structure of tumour necrosis factor ligands . -

Contribution of CD30/CD153 but Not of CD27/CD70, CD134/OX40L, Or
Contribution of CD30/CD153 but not of CD27/CD70, CD134/OX40L, or CD137/4-1BBL to the optimal induction of protective immunity to Mycobacterium avium Manuela Flo´ rido,* Margarida Borges,* Hideo Yagita,† and Rui Appelberg*,‡,1 *Laboratory of Microbiology and Immunology of Infection, Institute for Molecular and Cell Biology, and ‡ICBAS, Instituto de Cieˆncias Biome´dicas de Abel Salazar, University of Porto, Portugal; and †Department of Immunology, Juntendo University School of Medicine, Tokyo, Japan Abstract: A panel of monoclonal antibodies spe- the role played by the TNFRSF members CD27 (TNFRSF7), cific for CD27 ligand (CD70), CD30 ligand CD30 (TNFRSF8), CD134 (TNFRSF4 or OX40), and CD137 (CD153), CD134 ligand (OX40L), and CD137 li- (TNFRSF9 or 4-1BB) and their ligands CD70 (TNFSF7), gand (4-1BBL) were screened in vivo for their CD153 (TNFSF8), OX40L (TNFSF4), and 4-1BBL (TNFSF9), ability to affect the control of Mycobacterium respectively. avium infection in C57Bl/6 mice. Only the block- CD27/CD70 interactions participate in the early phases of T ing of CD153 led to increased mycobacterial bur- cell responses [2]. Engaging CD27 on T cells activates these dens. We then used CD30-deficient mice and found cells, leading to cytokine secretion and proliferation, and po- an increase in the proliferation of two strains of M. tentiates the activity of other accessory molecules [3]. Mice avium in these mice as compared with control an- deficient in CD27 have impaired responses to influenza virus imals. The increased mycobacterial growth was as- and reduced T cell memory generation [4]. Conversely, chronic sociated with decreased T cell expansion and re- in vivo triggering of CD27 by expression of a CD70 transgene duced interferon-␥ (IFN-␥) responses as a result of led to massive activation and proliferation of T cells with reduced polarization of the antigen-specific, IFN- conversion of naı¨ve cells into cells with an activated/memory ␥-producing T cells. -

Blockade of PD-1, PD-L1, and TIM-3 Altered Distinct Immune- and Cancer-Related Signaling Pathways in the Transcriptome of Human Breast Cancer Explants
G C A T T A C G G C A T genes Article Blockade of PD-1, PD-L1, and TIM-3 Altered Distinct Immune- and Cancer-Related Signaling Pathways in the Transcriptome of Human Breast Cancer Explants 1, 1, 2 1 1, Reem Saleh y, Salman M. Toor y, Dana Al-Ali , Varun Sasidharan Nair and Eyad Elkord * 1 Cancer Research Center, Qatar Biomedical Research Institute (QBRI), Hamad Bin Khalifa University (HBKU), Qatar Foundation (QF), Doha 34110, Qatar; [email protected] (R.S.); [email protected] (S.M.T.); [email protected] (V.S.N.) 2 Department of Medicine, Weil Cornell Medicine-Qatar, Doha 24144, Qatar; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +974-4454-2367 Authors contributed equally to this work. y Received: 21 May 2020; Accepted: 21 June 2020; Published: 25 June 2020 Abstract: Immune checkpoint inhibitors (ICIs) are yet to have a major advantage over conventional therapies, as only a fraction of patients benefit from the currently approved ICIs and their response rates remain low. We investigated the effects of different ICIs—anti-programmed cell death protein 1 (PD-1), anti-programmed death ligand-1 (PD-L1), and anti-T cell immunoglobulin and mucin-domain containing-3 (TIM-3)—on human primary breast cancer explant cultures using RNA-Seq. Transcriptomic data revealed that PD-1, PD-L1, and TIM-3 blockade follow unique mechanisms by upregulating or downregulating distinct pathways, but they collectively enhance immune responses and suppress cancer-related pathways to exert anti-tumorigenic effects. -

Jimmunol.1700608.Full.Pdf
The Ox40/Ox40 Ligand Pathway Promotes Pathogenic Th Cell Responses, Plasmablast Accumulation, and Lupus Nephritis in NZB/W F1 Mice This information is current as of September 29, 2021. Jonathan Sitrin, Eric Suto, Arthur Wuster, Jeffrey Eastham-Anderson, Jeong M. Kim, Cary D. Austin, Wyne P. Lee and Timothy W. Behrens J Immunol published online 10 July 2017 http://www.jimmunol.org/content/early/2017/07/07/jimmun Downloaded from ol.1700608 Supplementary http://www.jimmunol.org/content/suppl/2017/07/07/jimmunol.170060 http://www.jimmunol.org/ Material 8.DCSupplemental Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 29, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Author Choice Freely available online through The Journal of Immunology Author Choice option Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2017 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published July 10, 2017, doi:10.4049/jimmunol.1700608 The Journal of Immunology The Ox40/Ox40 Ligand Pathway Promotes Pathogenic Th Cell Responses, Plasmablast Accumulation, and Lupus Nephritis in NZB/W F1 Mice Jonathan Sitrin,* Eric Suto,† Arthur Wuster,*,‡ Jeffrey Eastham-Anderson,x Jeong M. -

Downloaded From
Engagement of CD153 (CD30 Ligand) by CD30 + T Cells Inhibits Class Switch DNA Recombination and Antibody Production in Human IgD+ IgM+ B Cells This information is current as of September 26, 2021. Andrea Cerutti, Andràs Schaffer, Raymond G. Goodwin, Shefali Shah, Hong Zan, Scott Ely and Paolo Casali J Immunol 2000; 165:786-794; ; doi: 10.4049/jimmunol.165.2.786 http://www.jimmunol.org/content/165/2/786 Downloaded from References This article cites 72 articles, 42 of which you can access for free at: http://www.jimmunol.org/content/165/2/786.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 26, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Engagement of CD153 (CD30 Ligand) by CD30؉ T Cells Inhibits Class Switch DNA Recombination and Antibody Production in Human IgD؉ IgM؉ B Cells1 Andrea Cerutti,2* Andràs Schaffer,*† Raymond G. -

OX40L Blockade Is Therapeutic in Arthritis, Despite Promoting Osteoclastogenesis
OX40L blockade is therapeutic in arthritis, despite promoting osteoclastogenesis Emily Gwyer Findlaya,1,2, Lynett Danksb,1, Jodie Maddena, Mary M. Cavanagha, Kay McNameeb, Fiona McCannb, Robert J. Snelgrovea, Stevan Shawc, Marc Feldmannd,3, Peter Charles Taylord, Nicole J. Horwoodd, and Tracy Hussella,3,4 aLeukocyte Biology Section, National Heart and Lung Institute, Imperial College London, London SW7 2AZ, United Kingdom; bKennedy Institute of Rheumatology, London W6 8LH, United Kingdom; cUCB Pharma, Slough SL1 4EN, United Kingdom; and dNuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, Kennedy Institute of Rheumatology, University of Oxford, Oxford OX3 7FY, United Kingdom Contributed by Marc Feldmann, November 19, 2013 (sent for review May 16, 2013) An immune response is essential for protection against infection, The TNF superfamily member OX40 (CD134) is induced 24 to but, in many individuals, aberrant responses against self tissues 48 h after T-cell activation and binds the equally inducible OX40 cause autoimmune diseases such as rheumatoid arthritis (RA). ligand (OX40L) on antigen-presenting cells (APCs), causing a bi- How to diminish the autoimmune response while not augmenting directional activating signal to both cells. OX40 signaling promotes infectious risk is a challenge. Modern targeted therapies such as T-cell survival and their division and cytokine production, and, in anti-TNF or anti-CD20 antibodies ameliorate disease, but at the APCs, OX40L signaling causes maturation and the release of in- cost of some increase in infectious risk. Approaches that might flammatory mediators (7), or, in the case of B cells, increased IgG specifically reduce autoimmunity and tissue damage without production (8). -
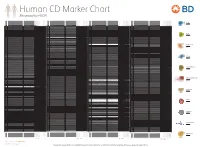
Reviewed by HLDA1
Human CD Marker Chart Reviewed by HLDA1 T Cell Key Markers CD3 CD4 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD8 CD1a R4, T6, Leu6, HTA1 b-2-Microglobulin, CD74 + + + – + – – – CD74 DHLAG, HLADG, Ia-g, li, invariant chain HLA-DR, CD44 + + + + + + CD158g KIR2DS5 + + CD248 TEM1, Endosialin, CD164L1, MGC119478, MGC119479 Collagen I/IV Fibronectin + ST6GAL1, MGC48859, SIAT1, ST6GALL, ST6N, ST6 b-Galactosamide a-2,6-sialyl- CD1b R1, T6m Leu6 b-2-Microglobulin + + + – + – – – CD75 CD22 CD158h KIR2DS1, p50.1 HLA-C + + CD249 APA, gp160, EAP, ENPEP + + tranferase, Sialo-masked lactosamine, Carbohydrate of a2,6 sialyltransferase + – – + – – + – – CD1c M241, R7, T6, Leu6, BDCA1 b-2-Microglobulin + + + – + – – – CD75S a2,6 Sialylated lactosamine CD22 (proposed) + + – – + + – + + + CD158i KIR2DS4, p50.3 HLA-C + – + CD252 TNFSF4,