Fact Sheet for Healthcare Providers Emergency Use Authorization (Eua) of Sotrovimab
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Corporate Governance
Strategic report Governance and remuneration Financial statements Investor information Corporate Governance In this section Chairman’s Governance statement 78 The Board 80 Corporate Executive Team 83 Board architecture 85 Board roles and responsibilities 86 Board activity and principal decisions 87 Our purpose, values and culture 90 The Board’s approach to engagement 91 Board performance 94 Board Committee information 96 Our Board Committee reports 97 Section 172 statement 108 Directors’ report 109 GSK Annual Report 2020 77 Chairman’s Governance statement In last year’s Governance statement, I explained that our primary Education and focus on Science objective for 2020 was to ensure there was clarity between the Given the critical importance of strengthening the pipeline, Board and management on GSK’s execution of strategy and its the Board has benefitted from devoting a higher proportion of operational priorities. We have aligned our long-term priorities its time in understanding the science behind our strategy and of Innovation, Performance and Trust powered by culture testing its application. It is important that the Board has a and agreed on the metrics to measure delivery against them. working understanding of the key strategic themes upon The Board’s annual cycle of meetings ensures that all major which our R&D strategy is based. These themes have been components of our strategy are reviewed over the course complemented by Board R&D science thematic deep dives. of the year. Our focus was on the fundamentals of our strategy: human The COVID-19 pandemic impacted and dominated all our genetics, the immune system and AI and ML, as well as to lives for the majority of 2020. -

Emergency Use Authorization (EUA) for Sotrovimab 500 Mg Center for Drug Evaluation and Research (CDER) Review
Emergency Use Authorization (EUA) for Sotrovimab 500 mg Center for Drug Evaluation and Research (CDER) Review Identifying Information Application Type EUA (EUA or Pre-EUA) If EUA, designate whether pre-event or intra-event EUA request. EUA Application EUA 000100 Number(s) Sponsor (entity EUA Sponsor requesting EUA or GlaxoSmithKline Research & Development Limited pre-EUA 980 Great West Road consideration), point Brentford Middlesex, TW8 9GS of contact, address, UK phone number, fax number, email GSK US Point of Contact address Debra H. Lake, M.S. Sr. Director Global Regulatory Affairs GlaxoSmithKline 5 Moore Drive PO Box 13398 Research Triangle Park, NC 27709-3398 (b) (6) Email: Phone Manufacturer, if GlaxoSmithKline, Parma. different from Sponsor Submission Date(s) Part 1: March 24, 2021 Part 2: March 29, 2021 Receipt Date(s) Part 1: March 24, 2021 Part 2: March 29, 2021 OND Division / Office Division of Antivirals /Office of Infectious Disease 1 Reference ID: 4802027 Product in the No Strategic National Stockpile (SNS) Distributor, if other (b) (4) than Sponsor I. EUA Determination/Declaration On February 4, 2020, the Secretary of Health and Human Services determined pursuant to section 564 of the Federal Food, Drug and Cosmetic (FD&C) Act that there is a public health emergency that has a significant potential to affect national security or the health and security of United States (US) citizens living abroad and that involves a novel (new) coronavirus (nCoV) first detected in Wuhan City, Hubei Province, China in 2019 (2019-nCoV). The virus is now named SARS-CoV-2, which causes the illness COVID-19. -

PEDIARIX Is a Vaccine
HIGHLIGHTS OF PRESCRIBING INFORMATION • If Guillain-Barré syndrome occurs within 6 weeks of receipt of a prior These highlights do not include all the information needed to use vaccine containing tetanus toxoid, the decision to give PEDIARIX should PEDIARIX safely and effectively. See full prescribing information for be based on potential benefits and risks. (5.2) PEDIARIX. • The tip caps of the prefilled syringes contain natural rubber latex which may cause allergic reactions. (5.3) PEDIARIX [Diphtheria and Tetanus Toxoids and Acellular Pertussis • Syncope (fainting) can occur in association with administration of Adsorbed, Hepatitis B (Recombinant) and Inactivated Poliovirus injectable vaccines, including PEDIARIX. Procedures should be in place Vaccine], Suspension for Intramuscular Injection to avoid falling injury and to restore cerebral perfusion following Initial U.S. Approval: 2002 syncope. (5.4) • If temperature ≥105°F, collapse or shock-like state, or persistent, ----------------------------- INDICATIONS AND USAGE ---------------------------- PEDIARIX is a vaccine indicated for active immunization against diphtheria, inconsolable crying lasting ≥3 hours have occurred within 48 hours after tetanus, pertussis, infection caused by all known subtypes of hepatitis B virus, receipt of a pertussis-containing vaccine, or if seizures have occurred and poliomyelitis. PEDIARIX is approved for use as a 3-dose series in infants within 3 days after receipt of a pertussis-containing vaccine, the decision born of hepatitis B surface antigen (HBsAg)-negative mothers. PEDIARIX to give PEDIARIX should be based on potential benefits and risks. (5.5) may be given as early as 6 weeks of age through 6 years of age (prior to the • For children at higher risk for seizures, an antipyretic may be 7th birthday). -

Final Attendee List
Jennifer Abnet GlaxoSmithKline I GlaxoSmithKline I Jane Arboleda APRN Guardant I Molly Benson Sanjiv Agarwala MD Puma Biotechnology I Cancer Expert Now I Joe Arminger AbbVie I Seth Berkowitz LCSW, Manmeet Ahluwalia MD, CCLS MBA Patricia Armstrong The Leukemia & Lymphoma Miami Cancer Institute I Novartis I Society V Steve Albers Kim Arnold APRN CPNP Barry Berman MD, MS Alexion V CPHON Florida Cancer Specialists I Servier Pharmaceuticals I Maritza Alencar DNP, Tizano Bernard MBA, APRN, BMTCN Sheila Arrington MSN, Cancer Care Centers of Miami Cancer Institute V APRN, NP-C, AOCN Brevard I Puma Biotechnology I Carmen Allen MSIT Ana Mari Bernardini Pharmavoxx V Shannon Ashmon Novartis Oncology I Eisai, Inc I Luly Almeida Bernard Berry MBA Incyte Corporation I Sarah Ashton MS AstraZeneca Pharmaceuticals Guardant Health I I Talat Almukhtar MD Orlando Health Cancer Melissa Austin Jason Bever Institute I Cancer Care Centers of Oncopeptides I Brevard I Beatrice Alvarado Roberts Amy Bignon MD Garland Avera Doyle Caris Life Sciences I University of Florida I Jazz Pharmaceuticals I Nadeem Bilani MD Tadeu Ambros MD Francie Babcock Cleveland Clinic I FCS I AMAG Pharmaceuticals/Covis I Angela Bilik RN BSN Douglas Anderson AstraZeneca I Incyte Corporation I Craig Bailey Astra Zeneca I Jamie Bilsky BS Blesson Andrews Genentech V Genentech I Kevin Barr Daiichi Sankyo I Rohit Bishnoi MD Ollie Annum PharmD University of Florida I BHMCR I Leonard Bennett PharmD EMD Serono I Brady Blackman Susmitha Apuri MD MorphoSys I Florida Cancer Specialists I Michael Bennett As of 4-22-21 Kimberly Blandon RN MSN Rick Breitenstein Memorial Cancer Institute I Apellis Pharmaceuticals I Denise Capo Karyopharm Therapeutics I Taryn Boiteau GlaxoSmithKline I Amanda Bridges Florida Society of Clinical Heidi Caravetta Tracy Bonds RN, BSN, Oncology I Exelixis, Inc. -

GLAXOSMITHKLINE LLC V. TEVA PHARMACEUTICALS USA, INC
Case: 18-1976 Document: 111 Page: 1 Filed: 10/02/2020 United States Court of Appeals for the Federal Circuit ______________________ GLAXOSMITHKLINE LLC, SMITHKLINE BEECHAM (CORK) LIMITED, Plaintiffs-Appellants v. TEVA PHARMACEUTICALS USA, INC., Defendant-Cross-Appellant ______________________ 2018-1976, 2018-2023 ______________________ Appeals from the United States District Court for the District of Delaware in No. 1:14-cv-00878-LPS-CJB, Chief Judge Leonard P. Stark. ______________________ Decided: October 2, 2020 ______________________ JUANITA ROSE BROOKS, Fish & Richardson, PC, San Diego, CA, argued for plaintiffs-appellants. Also represented by MICHAEL ARI AMON, CRAIG E. COUNTRYMAN, JONATHAN ELLIOT SINGER; ELIZABETH M. FLANAGAN, MICHAEL J. KANE, WILLIAM WOODFORD, Minneapolis, MN; DOUGLAS E. MCCANN, Wilmington, DE. WILLIAM M. JAY, Goodwin Procter LLP, Washington, DC, argued for defendant-cross-appellant. Also represented by JAIME ANN SANTOS; ELAINE BLAIS, J. Case: 18-1976 Document: 111 Page: 2 Filed: 10/02/2020 2 GLAXOSMITHKLINE LLC v. TEVA PHARMACEUTICALS USA, INC. ANTHONY DOWNS, ROBERT FREDERICKSON, III, CHRISTOPHER T. HOLDING, ALEXANDRA LU, LANA S. SHIFERMAN, DARYL L. WIESEN, Boston, MA; IRA J. LEVY, New York, NY. HANSJORG SAUER, Biotechnology Innovation Organization, Washington, DC, for amicus curiae Biotechnology Innovation Organization. Also represented by MELISSA A. BRAND; BRIAN PAUL BARRETT, Eli Lilly and Company, Indianapolis, IN. MICHAEL N. KENNEDY, Covington & Burling LLP, Washington, DC, for amicus curiae Pharmaceutical Research and Manufacturers of America. Also represented by STEVEN JOHN WINKELMAN; DAVID EVAN KORN, Pharmaceutical Research and Manufacturers Association of America, Washington, DC. ANDREW CURTIS NICHOLS, Winston & Strawn LLP, Washington, DC, for amicus curiae Association for Accessible Medicines. Also represented by GEORGE C. -

Declarations of Interest Thorax: First Published As 10.1136/Thoraxjnl-2016-209333.476 on 15 November 2016
Declarations of interest Thorax: first published as 10.1136/thoraxjnl-2016-209333.476 on 15 November 2016. Downloaded from KF Rabe reports financial for support for consultancy work P297 LUNG-FUNCTION PROFILE BEFORE AND AFTER THE from AstraZeneca, Chiesi, Novartis, MSD and GlaxoSmithKline, FIRST MODERATE TO SEVERE EXACERBATION DURING and grants from Altana, Novartis, AstraZeneca, MSD and THE WISDOM STUDY Nycomed. F Maltais reports financial support from Boehringer Ingelheim 10.1136/thoraxjnl-2016-209333.476 during the conduct of the study and, outside of the submitted work, financial support from Boehringer Ingelheim and GlaxoS- E Wouters, outside of the submitted work, reports personal fees mithKline for attendance at advisory boards, financial support from AstraZeneca, GlaxoSmithKline, Novartis, Takeda, Pfizer from Boehringer Ingelheim, GlaxoSmithKline, AstraZeneca and and Boehringer Ingelheim, and grants from AstraZeneca, GlaxoS- Novartis for speaking activities, and research support from Boeh- mithKline and Novartis. ringer Ingelheim, GlaxoSmithKline, AstraZeneca, Nycomed and H Magnussen received funding from Almirall, AstraZeneca, Novartis. Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Merck, Novar- tis, Takeda and Roche to conduct clinical studies, and has spoken at meetings and is a member of advisory boards for these and P295 EFFICACY AND SAFETY OF TIOTROPIUM/OLODATEROL other companies. IN PATIENTS WITH COPD BY ATS CATEGORY R Rodriguez-Roisin reports personal fees from AstraZeneca, Boehringer Ingelheim, Mylan, Pearl Therapeutics, Takeda, Teva 10.1136/thoraxjnl-2016-209333.474 and Ferrer, and grants and personal fees from Menarini and Almirall. F Maltais reports financial support from Boehringer Ingelheim K Tetzlaff and S Bell are employees of Boehringer Ingelheim during the conduct of the study and, outside of the submitted Pharma GmbH & Co. -
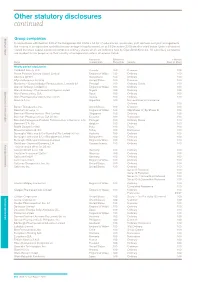
Other Statutory Disclosures Continued
Other statutory disclosures continued Strategic reportGroup companies Governance & remuneration Financial statements In accordance with Section 409 of the Companies Act 2006 a full list of subsidiaries, associates, joint ventures and joint arrangements, the country of incorporation and effective percentage of equity owned, as at 31 December 2015 are disclosed below. Unless otherwise stated the share capital disclosed comprises ordinary shares which are indirectly held by GlaxoSmithKline plc. All subsidiary companies are resident for tax purposes in their country of incorporation unless otherwise stated. Country of Effective % % Held by Name incorporation Ownership Security Class of Share Wholly owned subsidiaries 1506369 Alberta ULC Canada 100 Common 100 Action Potential Venture Capital Limited England & Wales 100 Ordinary 100 Adechsa GmbH Switzerland 100 Ordinary 100 Affymax Research Institute United States 100 Common 100 Alenfarma – Especialidades Farmaceuticas, Limitada (iv) Portugal 100 Ordinary Quota 100 Allen & Hanburys Limited (iv) England & Wales 100 Ordinary 100 Allen & Hanburys Pharmaceutical Nigeria Limited Nigeria 100 Ordinary 100 Allen Farmaceutica, S.A. Spain 100 Ordinary 100 Allen Pharmazeutika Gesellschaft m.b.H. Austria 100 Ordinary 100 Aners S.A (iv) Argentina 100 Non-endorsable Nominative Ordinary 100 Barrier Therapeutics, Inc. United States 100 Common 100 Beecham Group p l c England & Wales 100 20p Shares 'A'; 5p Shares B 100 Beecham Pharmaceuticals (Pte) Limited Singapore 100 Ordinary 100 Beecham Pharmaceuticals S.A (iv) (vi) Ecuador 100 Nominative 100 Beecham Portuguesa-Produtos Farmaceuticos e Quimicos, Lda Portugal 100 Ordinary Quota 100 Beecham S.A. (iv) Belgium 100 Ordinary 100 Biddle Sawyer Limited India 100 Equity 100 Biovesta Ilaçlari Ltd. Sti. Turkey 100 Nominative 100 Burroughs Wellcome & Co (Australia) Pty Limited (iv) (vi) Australia 100 Ordinary 100 Burroughs Wellcome & Co (Bangladesh) Limited Bangladesh 100 Ordinary 100 Burroughs Wellcome International Limited England & Wales 100 Ordinary 100 Caribbean Chemical Company, Ltd. -

Glaxosmithkline Plc Annual Report for the Year Ended 31St December 2000
GlaxoSmithKline 01 GlaxoSmithKline plc Annual Report for the year ended 31st December 2000 Contents Report of the Directors 02 Financial summary 03 Joint statement by the Chairman and the Chief Executive Officer 05 Description of business 29 Corporate governance 37 Remuneration report 47 Operating and financial review and prospects 69 Financial statements 70 Directors’ statements of responsibility 71 Report by the auditors 72 Consolidated statement of profit and loss 72 Consolidated statement of total recognised gains and losses 74 Consolidated statement of cash flow 76 Consolidated balance sheet 76 Reconciliation of movements in equity shareholders’ funds 77 Company balance sheet 78 Notes to the financial statements 136 Group companies 142 Principal financial statements in US$ 144 Financial record 153 Investor information 154 Shareholder return 156 Taxation information for shareholders 157 Shareholder information 158 Share capital 160 Cross reference to Form 20-F 162 Glossary of terms The Annual Report was approved by the Board 163 Index of Directors on 22nd March 2001 and published on 12th April 2001. Contact details 02 GlaxoSmithKline Financial summary 2000 1999 Increase Business performance £m £m CER % £ % Sales 18,079 16,164 9 12 Trading profit 5,026 4,378 12 15 Profit before taxation 5,327 4,708 11 13 Earnings/Net income 3,697 3,222 13 15 Earnings per Ordinary Share 61.0p 52.7p 14 16 Total results Profit before taxation 6,029 4,236 Earnings/Net income 4,154 2,859 Earnings per Ordinary Share 68.5p 46.7p Business performance: results exclude merger items and restructuring costs; 1999 sales and trading profit exclude the Healthcare Services businesses which were disposed of in 1999. -

Updates on COVID-19 Monoclonal Antibody Treatment In
Updates on COVID-19 Monoclonal Antibody (mAb) Treatment in the Outpatient Setting Overview • All providers should know how and when to refer patients for monoclonal antibody (mAB) treatment. • mAb treatment, when given early after symptom onset, can decrease the risk of hospitalization and death due to COVID-19 by as much as 70% to 85%. • Eligibility criteria for mAb treatment have been expanded to include additional medical conditions and factors that may place patients at high risk for progression to severe COVID-19. • Continue to refer eligible symptomatic patients for mAb treatment, regardless of vaccination status. • Sotrovimab is a new mAb product that has been granted emergency use authorization (EUA) by the Food and Drug Administration (FDA). • The EUA for REGEN-COV (casirivimab + imdevimab) has been updated to reduce the dose and allow for subcutaneous administration. • The EUA for REGEN-COV has also been expanded to include use as post-exposure prophylaxis for people exposed to someone with COVID-19 and at high risk for severe illness. • Health care providers should use only REGEN-COV or sotrovimab for the treatment of COVID-19 until further notice due to increasing prevalence of SARS-CoV-2 variants resistant to bamlanivimab and etesevimab. August 20, 2021 Dear Colleague, This letter summarizes important updates on monoclonal antibody (mAb) emergency use authorizations (EUAs) and treatment guidance. mAbs are the only authorized treatment option for patients with mild to moderate COVID-19 who are at high risk of developing severe illness. It is also the only option for post-exposure prophylaxis (PEP). As cases of COVID-19 continue to rise in New York City (NYC) due to more contagious and dangerous variants, it is critical that providers assist eligible patients to access this life-saving treatment by increasing patient awareness, encouraging prompt diagnostic testing following a COVID-19 exposure or symptom onset, and offering or referring patients for treatment. -

ESG Performance Summary 2020 About This Report
ESG Performance Summary 2020 About this report In this report: Trust is one of our three long-term priorities Our commitments 1 and is essential to how we achieve our purpose, Data summary 2 drive long-term growth and add value for society SASB index 17 United Nations Global Compact and our shareholders. Communication on Progress 20 Global Reporting Initiative We have 13 commitments that support About our reporting guidelines 25 our Trust priority and drive progress in the This document provides a comprehensive Assurance report 30 key areas where we can make a significant summary of environmental, social and Public policies available online 32 impact, and ensure that we are running our governance (ESG) data from across our business in a responsible way. business. This complements our wider reporting on responsible business in our These commitments seek to address Annual Report where we report progress In our Annual Report: the most material topics relevant to on our 13 Trust commitments and in the Stakeholder engagement our stakeholders and to our business, responsible business pages of gsk.com. Progress against our Trust commitments and are designed to help us respond Climate change resilience (TCFD) to challenges and opportunities within our industry and society more broadly. Other online reporting: They contribute to many of the UN Materiality assessment Sustainable Development Goals, and Human rights as a science-led, global healthcare Sustainable Development Goals company, our biggest contribution is Political advocacy towards Goal 3: ensure healthy lives Patient group funding and promote well-being for all at all ages. Trade association memberships Charitable grant contributions Cautionary statement Criteria for working with Public Policy Groups See page 32 of this document for the cautionary statement regarding forward-looking statements. -

Curriculum Vitae Leonard Friedland, M.D
CURRICULUM VITAE LEONARD FRIEDLAND, M.D. 5 Crescent Drive, Philadelphia, PA 19112 484-620-9540 [email protected] [email protected] PROFILE I am a pediatrician and research scientist who is passionate about vaccines. I spend my days helping people understand the science of vaccines and complex ideas about how vaccines help to improve public health and the lives of patients. Following a rewarding academic career in teaching and patient care, I joined GSK in 2003 to focus my efforts on vaccination and public health. At GSK, I am involved in the development of vaccines for use in children, adolescents, adults, the elderly, and pregnancy; including vaccines for the prevention of flu, meningitis, whooping cough, rotavirus, hepatitis, measles, RSV and shingles. I am privileged to be GSK’s medical and public health representative and spokesperson for US vaccine topics at CDC, other public health venues, congresses, and media outlets. EDUCATION Vassar College, Poughkeepsie, NY A.B. (Biology), 1979-1983 Mount Sinai School of Medicine, New York, NY M.D., 1983-1987 Xavier Univeristy Center for Management and Professional Development, Cincinnati, OH Physician Leadership and Management Program, 1994-1995 GRADUATE MEDICAL TRAINING Residency, Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, 1987-1990 Fellowship, Pediatric Emergency Medicine, St. Christopher’s Hospital for Children, Philadelphia, 1990-1992 PROFESSIONAL EXPERIENCE GlaxoSmithKline (GSK), Philadelphia, PA 2003 – present Vice President, Scientific Affairs and Public Health, Vaccines, North America (2013-present) Provide strategic scientific affairs leadership for development and marketed vaccines within the US. Influence and inform prophylactic vaccines medical affairs, health outcomes and epidemiology strategy and research priorities. -

Glaxosmithkline Press Releases Page 1 of 2 Corporate Archive
Corporate Archive: GlaxoSmithKline, Government reach civil settlement Page 1 of 2 Corporate News, Articles and Press Releases Bookmark Us Home Home > GlaxoSmithKline Press Release > 2003 Company Airbus GlaxoSmithKline Press Releases Amazon AOL Apple AstraZeneca 16th April, 2003 ATT Boeing GlaxoSmithKline, Government reach civil settlement British-Telecom Cadbury- (Gsk) Schweppes Prescription Assistance Program Annual income under $42k Cisco to qualify CitiGroup www.myrxadvocate.com Glaxosmithkline careers Coca-Cola The Premier online Destination for Jobs paying Over $100K. Dell Search Now. Birth Defects Lawsuit Ebay www.TheLadders.com If you have given birth to a child with birth defects GlaxoSmithKline while on ... Glaxosmithkline Job -2006 www.awkolaw.com/drugs_paxilbirth -2005 Every Job. Everywhere. -2004 www.JobsOnline.net -2003 Birth Defects Lawsuit Google If you have given birth to a child with birth defects while Halliburton on ... Hewlett-Packard www.awkolaw.com/drugs_paxilbirth HSBC IBM GlaxoSmithKline, Government reach civil settlement Intel KPMG PHILADELPHIA, PA., April 16, 2003 -- GlaxoSmithKline today announced it has reached a civil settlement with the U.S. Department of Justice, acting through the U.S. Attorney’s Office for Massachusetts, the Office of the Inspector McDonalds General of the US Department of Health and Human Services and the states. Microsoft Morgan-Stanley The sole issue at the heart of the investigation leading to the settlement was how GSK’s heritage companies Nestle interpreted an ambiguous aspect of the Medicaid Best Price Statute and how they applied that statute to limited arrangements with a single customer involving the repackaging of a small number of its products. Oracle Orange GSK continues to believe that its interpretation of the law was reasonable and in good faith.