Statewide Rural and Remote Clinical Network
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Your Labor Member in the Queensland Parliament
YOUR LABOR MEMBER IN THE QUEENSLAND PARLIAMENT Cape Vork / Douglas / Cooktown / Mareeba: Torres Strait / NPA P: 1800816264 - Fax: 07 40312437 P: 1800802391 - Fax: 07 4069 1620 PO Box 2080, Cairns 4870 PO Box 437, Thursday Island 4875 E: [email protected] E: cook.th [email protected] Submission to the Queensland Competition Authority Level 19 12 Creek Street BRISBANE QLD 4001 REVIEW OF SUN WATER PRICING STRUCTURE Submission to the Queensland Competition Authority by Jason O'Brien MP Member for Cook, on behalf of a constituent who is a Sun Water user, requesting changes to the pricing policy of Sun Water to their customers holding pension concession cards who access sun water for their domestic use only. Under the present Sun Water tariff structure they are able to negotiate how much revenue could be collected from variable and fixed charges. My submission is that Sun Water should be free to offer a Pensioner Water Subsidy Scheme for eligible pensions to reduce the impact of increased water price increases. This concession could be in the form of a rebate similar to the rate rebate scheme which applies across the state off local government rates charges. Sun Water must have the ability to provide water services to the community at a reasonable cost taking into account the most effective way to utilise the resource for the community's benefit. To this end pensions accessing Sun Water's resource purely for domestic use should be considered in a wider public interest context. Prices should be cost reflective and take into account relevant public interest matters such as pensioners accessing their resource In conclusion I submit that Sun Water should be providing a Pensioner Water Subsidy Scheme and the Queensland Competition Authority should recognise this as a public interest issue. -
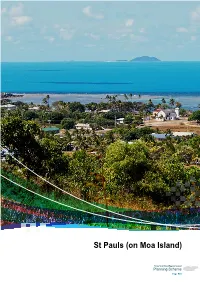
St Pauls (On Moa Island) - Local Plan Code
7.2.13 St Pauls (on Moa Island) - local plan code Part 7: Local Plans St Pauls (on Moa Island) St Pauls (on Moa Island) Torres Strait Island Regional Council Planning Scheme Page 523 Torres Strait Island Regional Council Planning Scheme Page 524 Part 7: Local Plans St Pauls (on Moa Island) Papua New Guinea Saibai Ugar Boigu Stephen Island Erub Dauan Darnley Island Masig Yorke Island Iama Mabuyag Yam Island Mer Poruma Murray Island Coconut Island Badu Kubin Moa SStt PPaulsauls Warraber Sue Island Keriri Hammond Island Mainland Australia Mainland Australia Torres Strait Island Regional Council Planning Scheme Page 525 Editor’s Note – Community Snapshot Location Topography and Environment • St Pauls is located on the eastern side of Moa • Moa Island, like other islands in the group, is Island, which is part of the Torres Strait inner and a submerged remnant of the Great Dividing near western group of islands. St Paul’s nearest Range, now separated by sea. The island neighbour is Kubin, which is located on the comprises of largely of rugged, open forest and south-western side of Moa Island. Approximately is approximately 17km in diameter at its widest 15km from the outskirts of St Pauls. point. • Native flora and fauna that have been identified Population near St Pauls include fawn leaf nosed bat, • According to the most recent census, there were grey goshawk, emerald monitor, little tern, 258 people living in St Pauls as at August 2011, red goshawk, radjah shelduck, lipidodactylus however, the population is highly transient and primilus, bare backed fruit bat, torresian tube- this may not be an accurate estimate. -

Between Australia and New Guinea-Ecological and Cultural
Geographical Review of Japan Vol. 59 (Ser. B), No. 2, 69-82, 1986 Between Australia and New Guinea-Ecological and Cultural Diversity in the Torres Strait with Special Reference to the Use of Marine Resources- George OHSHIMA* The region between lowland Papua and the northern tip of the Australian continent presents a fascinating panorama of ecological, cultural and socio-economic diversity. In lowland Papua and on its associated small islands such as Saibai, Boigu and Parama, a combination of coastal forests and muddy shores dominates the scene, whereas the Torres Strait Islands of volcanic and limestone origin, together with raised coral islands and their associated reef systems present a range of island ecosystems scattered over a broad territory some 800km in extent. Coralline habitats extend south wards to the Cape York Peninsula and some parts of Arnhem Land. Coupled with those ecological diversities within a relatively small compass across the Torres Strait, the region has evoked important questions concerning the archaeological and historical dichotomy between Australian hunter-gatherers and Melanesian horticulturalists. This notion is also reflectd in terms of its complex linguistic, ethnic and political composition. In summarizing the present day cultural diversity of the region, at least three major components emerge: hunter-gatherers in the Australian Northern Territory, Australian islanders and tribal Papuans. Historically, these groups have interacted in complex ways and this has resulted in an intricate intermingling of cultures and societies. Such acculturation processes operating over thousands of years make it difficult to isolate meaning ful trends in terms of "core-periphery" components of the individual cultures. -

How Torres Strait Islanders Shaped Australia's Border
11 ‘ESSENTIALLY SEA‑GOING PEOPLE’1 How Torres Strait Islanders shaped Australia’s border Tim Rowse As an Opposition member of parliament in the 1950s and 1960s, Gough Whitlam took a keen interest in Australia’s responsibilities, under the United Nations’ mandate, to develop the Territory of Papua New Guinea until it became a self-determining nation. In a chapter titled ‘International Affairs’, Whitlam proudly recalled his government’s steps towards Papua New Guinea’s independence (declared and recognised on 16 September 1975).2 However, Australia’s relationship with Papua New Guinea in the 1970s could also have been discussed by Whitlam under the heading ‘Indigenous Affairs’ because from 1973 Torres Strait Islanders demanded (and were accorded) a voice in designing the border between Australia and Papua New Guinea. Whitlam’s framing of the border issue as ‘international’, to the neglect of its domestic Indigenous dimension, is an instance of history being written in what Tracey Banivanua- Mar has called an ‘imperial’ mode. Historians, she argues, should ask to what extent decolonisation was merely an ‘imperial’ project: did ‘decolonisation’ not also enable the mobilisation of Indigenous ‘peoples’ to become self-determining in their relationships with other Indigenous 1 H. C. Coombs to Minister for Aboriginal Affairs (Gordon Bryant), 11 April 1973, cited in Dexter, Pandora’s Box, 355. 2 Whitlam, The Whitlam Government, 4, 10, 26, 72, 115, 154, 738. 247 INDIGENOUS SELF-determinatiON IN AUSTRALIA peoples?3 This is what the Torres Strait Islanders did when they asserted their political interests during the negotiation of the Australia–Papua New Guinea border, though you will not learn this from Whitlam’s ‘imperial’ account. -

Cultural Heritage Series
VOLUME 4 PART 2 MEMOIRS OF THE QUEENSLAND MUSEUM CULTURAL HERITAGE SERIES 17 OCTOBER 2008 © The State of Queensland (Queensland Museum) 2008 PO Box 3300, South Brisbane 4101, Australia Phone 06 7 3840 7555 Fax 06 7 3846 1226 Email [email protected] Website www.qm.qld.gov.au National Library of Australia card number ISSN 1440-4788 NOTE Papers published in this volume and in all previous volumes of the Memoirs of the Queensland Museum may be reproduced for scientific research, individual study or other educational purposes. Properly acknowledged quotations may be made but queries regarding the republication of any papers should be addressed to the Editor in Chief. Copies of the journal can be purchased from the Queensland Museum Shop. A Guide to Authors is displayed at the Queensland Museum web site A Queensland Government Project Typeset at the Queensland Museum CHAPTER 4 HISTORICAL MUA ANNA SHNUKAL Shnukal, A. 2008 10 17: Historical Mua. Memoirs of the Queensland Museum, Cultural Heritage Series 4(2): 61-205. Brisbane. ISSN 1440-4788. As a consequence of their different origins, populations, legal status, administrations and rates of growth, the post-contact western and eastern Muan communities followed different historical trajectories. This chapter traces the history of Mua, linking events with the family connections which always existed but were down-played until the second half of the 20th century. There are four sections, each relating to a different period of Mua’s history. Each is historically contextualised and contains discussions on economy, administration, infrastructure, health, religion, education and population. Totalai, Dabu, Poid, Kubin, St Paul’s community, Port Lihou, church missions, Pacific Islanders, education, health, Torres Strait history, Mua (Banks Island). -

Boigu Islands, Form the Northern Island Group of Torres Strait, Located Approximately 150 Km North of Thursday Island (See Figure 1)
PROFILE FOR MANAGEMENT OF THE HABITATS AND RELATED ECOLOGICAL AND CULTURAL RESOURCE VALUES OF DAUAN ISLAND January 2013 Prepared by 3D Environmental for Torres Strait Regional Authority Land & Sea Management Unit Cover image: 3D Environmental (2013) EXECUTIVE SUMMARY The granite rock pile that forms Dauan, along with nearby Saibai and Boigu Islands, form the Northern Island Group of Torres Strait, located approximately 150 km north of Thursday Island (see Figure 1). Whilst Saibai and Boigu Island are extensions of the alluvial Fly Platform, geologically part of the Papua New Guinea mainland, Dauan is formed on continental basement rock which extends northward from Cape York Peninsula to Mabadauan Hill on the south-west coast of Papua New Guinea. A total of 14 vegetation communities, within ten broad vegetation groups and 14 regional ecosystems are recognised on the island. The total known flora of comprises 402 species (14 ferns, 388 angiosperms), with 317 native and 85 naturalised species. Nine plant species are considered threatened at the commonwealth and state levels and a further 25 species considered to have significance at a regional level. As for the majority of Torres Strait Islands there is a lack of systematic survey of fauna habitats on the island. A desktop review identified 135 fauna species that are reported to occur on Dauan. This can be compared with the 384 terrestrial fauna species that have been reported for the broader Torres Strait Island group. The Dauan fauna comprises 20 reptiles, 100 birds, 3 frogs and 12 mammals. Of these, one reptile, one bird and four mammal species are introduced. -

Torres Strait Islanders: a New Deal
The Parliament of the Commonwealth of Australia TORRES STRAIT ISLANDERS: A NEW DEAL A REPORT ON GREATER AUTONOMY FOR TORRES STRAIT ISLANDERS House of Representatives Standing Committee on Aboriginal & Torres Strait Islander Affairs August 1997 Canberra Commonwealth of Australia 1997 ISBN This document was produced from camera-ready copy prepared by the House of Representatives Standing Committee on Aboriginal and Torres Strait Islander Affairs and printed by AGPS Canberra. The cover was produced in the AGPS design studios. The graphic on the cover was developed from a photograph taken on Yorke/Masig Island during the Committee's visit in October 1996. CONTENTS FOREWORD ix TERMS OF REFERENCE xii MEMBERSHIP OF THE COMMITTEE xiii GLOSSARY xiv SUMMARY AND RECOMMENDATIONS xv CHAPTER 1 – INTRODUCTION REFERRAL TO COMMITTEE.......................................................................................................................................1 CONDUCT OF THE INQUIRY ......................................................................................................................................1 SCOPE OF THE REPORT.............................................................................................................................................2 PRELIMINARY OBSERVATIONS .................................................................................................................................3 Commonwealth-State Cooperation ....................................................................................................................3 -

Card Operated Meter Information
Purchasing a power card for your card-operated meter Power cards are available from the following sales outlets: Community Retail Agent Address Arkai (Kubin) Community T.S.I.R.C. - Kubin KUBIN COMMUNITY, MOA ISLAND QLD 4875 Arkai (Kubin) Community CEQ - Kubin IKILGAU YABY RD, KUBIN VILLAGE, MOA ISLAND QLD 4875 Aurukun Island & Cape 39 KANG KANG RD, AURUKUN QLD 4892 Aurukun Supermarket Aurukun Kang Kang Café 502 KANG KAND RD, AURUKUN QLD 4892 Badu (Mulgrave) Island Badu Hotel 199 NONA ST, BADU ISLAND QLD 4875 Badu (Mulgrave) Island Island & Cape Badu MAIRU ST, BADU ISLAND QLD 4875 Supermarket (Bottom Shop) Badu (Mulgrave) Island J & J Supermarket 341 CHAPMAN ST, BADU ISLAND QLD (Top Shop) 4875 Badu (Mulgrave) Island T.S.I.R.C. - Badu NONA ST, BADU ISLAND QLD 4875 Bamaga Bamaga BP Service AIRPORT RD, BAMAGA QLD 4876 Station Bamaga Cape York Traders 201 LUI ST, BAMAGA QLD 4876 – Bamaga Store Bamaga CEQ – Bamaga 105 ADIDI AT, BAMAGA QLD 4876 Supermarket Boigu (Talbot) Island CEQ – Boigu TOBY ST, BOIGU QLD 4875 Supermarket Boigu (Talbot) Island T.S.I.R.C. - Boigu 66 CHAMBERS ST, BOIGU ISLAND QLD 4875 Darnley Island (Erub) Daido Tavern PILOT ST, DARNLEY ISLAND QLD 4875 Darnley Island (Erub) T.S.I.R.C. - Darnley COUNCIL OFFICE, DARNLEY ISLAND QLD 4875 Dauan Island (Mt CEQ - Dauan MAIN ST, DAUAN ISLAND QLD 4875 Cornwallis) Supermarket Dauan Island (Mt T.S.I.R.C. - Dauan COUNCIL OFFICE, MAIN ST, DAUAN Cornwallis) ISLAND QLD 4875 Doomadgee CEQ – Doomadgee 266 GUNNALUNJA DR, DOOMADGEE QLD Supermarket 4830 Doomadgee Doomadgee 1 GOODEEDAWA RD, DOOMADGEE -

Part 7 Transport Infrastructure Plan
Sea Transport Safety The marine investigation unit of the Australian Transport Safety Bureau (ATSB) was contacted for information pertaining to recent accidents and incidents with large trading vessels in the region. The data provided related to five incidents that occurred after July 1995 and before 2004: a) A man overboard from the vessel Murshidabad in 1996; b) A close quarters situation between the Maersk Taupo and a small dive runabout off Ackers Shoal Beacon in 1997; c) The grounding of the vessel Thebes on Larpent Bank in 1997; d) The grounding of the vessel Dakshineshwar on Larpent Bank in 1997; and e) The grounding of the vessel NOL Amber on Larpent Bank in 1997. Figure 3.7 shows the location of marine accidents that have occurred in northern Queensland in 2004. Figure 3.7 Location of Marine Accidents in Northern Queensland (2004) Source: MSQ: 2005 Torres Strait Transport Infrastructure Plan - Integrated Strategy Report J:\mmpl\10303705\Engineering\Reports\Transport Infrastructure Plan\Transport Infrastructure Plan - Rev I.doc Revision I November 2006 Page 21 Figure 3.8 Existing Ferry Services Torres Strait Transport Ugar (Stephen) Island Infrastructure Plan Papua New Guinea Ferry Routes ° Saibai (Kaumag) Island Dauan Island Erub (Darnley) Island Map 1 - Saibai (Kaumag) Island to Dauan Island 1:200,000 Map 2 - Ugar (Stephen) Island to Erub (Darnley) Island 1:150,000 Hammond Waiben Map 1 Island (Thursday) Island Map 2 Nguruppai (Horn) Island Muralug (Prince of Wales) Island Map 3 Seisia Seisia Map 3 - Thursday Island 1:300,000 -

1998 ANNUAL REPORT 60011 Cover 16/11/98 2:43 PM Page 2
TORRES STRAIT REGIONAL AUTHORITY 1997~1998 ANNUAL REPORT 60011 Cover 16/11/98 2:43 PM Page 2 ©Commonwealth of Australia 1998 ISSN 1324–163X This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Torres Strait Regional Authority (TSRA). Requests and inquiries concerning reproduction rights should be directed to the Public Affairs Officer, TSRA, PO Box 261, Thursday Island, Queensland 4875. The artwork on the front cover was designed by Torres Strait Islander artist, Alick Tipoti. Annual Report 1997~98 PUPUA NEW GUINEA SAIBAI ISLAND (Kaumag Is) BOIGU ISLAND UGAR (STEPHEN) ISLAND DAUAN ISLAND TORRES STRAIT DARNLEY ISLAND YAM ISLAND MASIG (YORKE) ISLAND MABUIAG ISLAND MER (MURRAY) ISLAND BADU ISLAND PORUMA (COCONUT) ISLAND ST PAULS WARRABER (SUE) ISLAND KUBIN MOA ISLAND HAMMOND ISLAND THURSDAY ISLAND (Port Kennedy, Tamwoy) HORN ISLAND PRINCE OF WALES ISLAND SEISIA BAMAGA CAPE YORK TORRES STRAIT REGIONAL AUTHORITY © Commonwealth of Australia 1998 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Torres Strait Regional Authority (TSRA). Requests and inquiries concerning reproduction rights should be directed to the Public Affairs Officer, TSRA, PO Box 261, Thursday Island, Queensland 4875. The artwork on the front cover was designed by Torres Strait Islander artist, Alick Tipoti. TORRES STRAIT REGIONAL AUTHORITY Senator the Hon. John Herron Minister for Aboriginal and Torres Strait Islander Affairs Suite MF44 Parliament House CANBERRA ACT 2600 Dear Minister In accordance with section 144ZB of the Aboriginal and Torres Strait Islander Commission Act 1989, I am delighted to present you with the fourth Annual Report of the Torres Strait Regional Authority (TSRA). -

Water Stories from Torres Strait: Dauan and Saibai Islands
Water stories from Torres Strait: Dauan and Saibai Islands by Teena Akiba, Torres Strait Island Regional Council Let me tell you some water stories about growing up on Dauan Island. Dauan Island, in the north western island group of Torres Strait, is much known for its rocky hillsides, large boulders and tropical flora and fauna. Throughout the island there are many caves, some of which still remain undiscovered. Some, however, are well-known for their freshwater springs that form wells to supply water for the families. In total, there are 21 named natural wells on Dauan: Manarr, Dhobani, Dhaniw erad, Woesa- kuik, Dhogai-pudhaisinga, Meri-Mila, Akana-mai, Kupa kuik, Valley, Sazil-mudh, Wasana- pudhayzinga, Kuku, Kaladagam, Sapu, Mari-nguki, Arum-kodh, Awgadhaw-nguki, Kuyaman Klakau Pagayzinga, Maiwan, Gaile, Ama Kuduloena mai. As children we would scour the hills without carrying any water with us because we could always find a drink from a nearby well. We would clear the dead leaves and other material away from the well and wait for the water to settle. Then we would break leaves from nearby trees or use lily pads, shape them into a cone and scoop the water up to quench our thirst; then continue on our barefooted quests. Some of the wells are filled with water all year round while others may look dry but are surrounded by lush plant growth and are home to many animals. When holes are dug in these dry wells, they fill with water which, when settled, form clear filtered bodies of water. As a child growing up in the late 1970s and early 1980s, I recollect waking early in the mornings to help our grandparents, uncles or aunts follow the hoses that went for kilometres from the well to the shower shed. -

Dauan Land and Sea Profile
Dauan Land and Sea Profile RANGER GROUP Rangers 2015 MANAGEMENT PRIORITIES LAND • Weeds • Burning • Native plants and animals • Community garden OVERVIEW • Native nursery Traditional island name Dauan SEA Western name Mount Cornwallis • Turtle and dugong • Marine Debris Top Western Islands Cluster Guda Maluilgal Nation • Sea Patrol Local government TSIRC & TSC Registered Native Title Dauanalgaw (TSI) PEOPLE • Visitor management Body Corporate (RNTBC) Corporation RNTBC • Traditional and cultural sites • Traditional ecological knowledge Land type Continental Island • Community involvement Air distance from • Training 135 Thursday Island (km) Area (ha) 364 KEY VALUES Indicative max length (km) 3 CLIMATE CHANGE RISK Indicative max breadth (km) 3 Vulnerability to sea level rise (+1.0m) Very Low Max elevation (m) 295 Sea level rise response options Very High Healthy sea Marine water Coral reefs Seagrass Dugong Marine turtles Coastline length (km) 10 ecosystems quality meadows Population 133 (2011 ABS Census) Area of island zoned 21 development (ha) Subsistence Healthy land Sustainable Coasts Mangroves Coastal birds fishing ecosystems human settlements and beaches and wetlands Area of disturbed / 35 (9.6%) / undisturbed vegetation (ha/%) 329 (90.4%) Supporting the Land and Sea Management Strategy for Torres Strait COMMUNITY OVERVIEW FUTURE SUSTAINABILITY INITIATIVES Dauan is a very small (364ha) continental island RECENT ACHIEVEMENTS The Dauan community is highly reliant on air transport, diesel powered electricity generation and barge transport in the Top Western Islands Cluster of the Torres Recent land and sea management achievements include: of supplies and materials to and from the community. Strait about 135km north of Thursday Island. ○ Community-based dugong and turtle management plan in place Renewable energy options will be explored to reduce Dauan (population 133) lies just a few km from carbon emissions and work towards energy independence.