Correlation Between Flow Cytometry and Histologic Findings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Introduction to Flow Cytometry Principles Data Analysis Protocols Troubleshooting
Flow Cytometry ipl.qxd 11/12/06 11:14 Page i Introduction to Flow Cytometry Principles Data analysis Protocols Troubleshooting By Misha Rahman, Ph.D. Technical advisors Andy Lane, Ph.D. Angie Swindell, M.Sc. Sarah Bartram, B.Sc. Your first choice for antibodies! Flow Cytometry ipl.qxd 11/12/06 11:14 Page ii Flow Cytometry ipl.qxd 11/12/06 11:14 Page iii Introduction to Flow Cytometry Principles Data analysis Protocols Troubleshooting By Misha Rahman, Ph.D. Technical advisors Andy Lane, Ph.D. Angie Swindell, M.Sc. Sarah Bartram, B.Sc. Flow Cytometry ipl.qxd 11/12/06 11:14 Page 2 Preface How can I explain what flow cytometry is to someone that knows nothing about it? Well, imagine it to be a lot like visiting a supermarket. You choose the goods you want and take them to the cashier. Usually you have to pile them onto a conveyor. The clerk picks up one item at a time and interrogates it with a laser to read the barcode. Once identified and if sense prevails, similar goods are collected together e.g. fruit and vegetables go into one shopping bag and household goods into another. Now picture in your mind the whole process automated; replace shopping with biological cells; and substitute the barcode with cellular markers – welcome to the world of flow cytometry and cell sorting! We aim to give you a basic overview of all the important facets of flow cytometry without delving too deeply into the complex mathematics and physics behind it all. For that there are other books (some recommended at the back). -

Bone Marrow Immunophenotyping by Flow Cytometry in Refractory Cytopenia of Childhood
Myelodysplastic Syndromes ARTICLES Bone marrow immunophenotyping by flow cytometry in refractory cytopenia of childhood Anna M. Aalbers,1,2 Marry M. van den Heuvel-Eibrink,2 Irith Baumann,3 Michael Dworzak,4 Henrik Hasle,5 Franco Locatelli,6 Barbara De Moerloose,7 Markus Schmugge,8 Ester Mejstrikova,9 Michaela Nováková,9 Marco Zecca,10 C. Michel Zwaan,2 Jeroen G. te Marvelde,1 Anton W. Langerak,1 Jacques J.M. van Dongen,1 Rob Pieters,2 Charlotte M. Niemeyer,11 and Vincent H.J. van der Velden1 1Department of Immunology, Erasmus MC, Erasmus University Medical Center, Rotterdam, The Netherlands; 2Department of Pediatric Oncology/Hematology, Sophia Children’s Hospital - Erasmus University Medical Center, Rotterdam, The Netherlands; 3Department of Pathology, Clinical Centre South West, Böblingen Clinics, Germany; 4St. Anna Children’s Hospital and Children’s Cancer Research Institute, Department of Pediatrics, Medical University of Vienna, Austria; 5Department of Pediatrics, Aarhus University Hospital Skejby, Aarhus, Denmark; 6Department of Pediatric Hematology-Oncology, IRCCS Ospedale Bambino Gesù, Rome, University of Pavia, Italy; 7Department of Pediatric Hematology/Oncology, Ghent University Hospital, Ghent, Belgium; 8Department of Hematology, University Children’s Hospital, Zurich, Switzerland; 9Department of Pediatric Hematology/Oncology, Charles University and University Hospital Motol, Prague, Czech Republic; 10Pediatric Hematology, Fondazione IRCCS Policlinico San Matteo, Pavia, Italy; and 11Department of Pediatrics and Adolescent Medicine, Division of Pediatric Hematology and Oncology, University of Freiburg, Germany ABSTRACT Refractory cytopenia of childhood is the most common type of childhood myelodysplastic syndrome. Because the majority of children with refractory cytopenia have a normal karyotype and a hypocellular bone marrow, differ- entiating refractory cytopenia from the immune-mediated bone marrow failure syndrome (very) severe aplastic anemia can be challenging. -

The AML Guide Information for Patients and Caregivers Acute Myeloid Leukemia
The AML Guide Information for Patients and Caregivers Acute Myeloid Leukemia Emily, AML survivor Revised 2012 Inside Front Cover A Message from Louis J. DeGennaro, PhD President and CEO of The Leukemia & Lymphoma Society The Leukemia & Lymphoma Society (LLS) wants to bring you the most up-to-date blood cancer information. We know how important it is for you to understand your treatment and support options. With this knowledge, you can work with members of your healthcare team to move forward with the hope of remission and recovery. Our vision is that one day most people who have been diagnosed with acute myeloid leukemia (AML) will be cured or will be able to manage their disease and have a good quality of life. We hope that the information in this Guide will help you along your journey. LLS is the world’s largest voluntary health organization dedicated to funding blood cancer research, advocacy and patient services. Since the first funding in 1954, LLS has invested more than $814 million in research specifically targeting blood cancers. We will continue to invest in research for cures and in programs and services that improve the quality of life for people who have AML and their families. We wish you well. Louis J. DeGennaro, PhD President and Chief Executive Officer The Leukemia & Lymphoma Society Inside This Guide 2 Introduction 3 Here to Help 6 Part 1—Understanding AML About Marrow, Blood and Blood Cells About AML Diagnosis Types of AML 11 Part 2—Treatment Choosing a Specialist Ask Your Doctor Treatment Planning About AML Treatments Relapsed or Refractory AML Stem Cell Transplantation Acute Promyelocytic Leukemia (APL) Treatment Acute Monocytic Leukemia Treatment AML Treatment in Children AML Treatment in Older Patients 24 Part 3—About Clinical Trials 25 Part 4—Side Effects and Follow-Up Care Side Effects of AML Treatment Long-Term and Late Effects Follow-up Care Tracking Your AML Tests 30 Take Care of Yourself 31 Medical Terms This LLS Guide about AML is for information only. -

Treatment Induced Cytotoxic T-Cell Modulation in Multiple Myeloma Patients
ORIGINAL RESEARCH published: 15 June 2021 doi: 10.3389/fonc.2021.682658 Treatment Induced Cytotoxic T-Cell Modulation in Multiple Myeloma Patients Gregorio Barilà, Laura Pavan, Susanna Vedovato, Tamara Berno, Mariella Lo Schirico, Massimiliano Arangio Febbo, Antonella Teramo, Giulia Calabretto, Cristina Vicenzetto, Vanessa Rebecca Gasparini, Anna Fregnani, Sabrina Manni, Valentina Trimarco, Samuela Carraro, Monica Facco, Francesco Piazza, Gianpietro Semenzato and Renato Zambello* Department of Medicine (DIMED), Hematology and Clinical Immunology Section, Padua University School of Medicine, Edited by: Padova, Italy Roberto Mina, Università degli Studi di Torino, Italy Reviewed by: The biology of plasma cell dyscrasias (PCD) involves both genetic and immune-related Mattia D’ Agostino, factors. Since genetic lesions are necessary but not sufficient for Multiple Myeloma (MM) University of Turin, Italy evolution, several authors hypothesized that immune dysfunction involving both B and T Michele Cea, University of Genoa, Italy cell counterparts plays a key role in the pathogenesis of the disease. The aim of this study *Correspondence: is to evaluate the impact of cornerstone treatments for Multiple Myeloma into immune Renato Zambello system shaping. A large series of 976 bone marrow samples from 735 patients affected by [email protected] PCD was studied by flow analysis to identify discrete immune subsets. Treated MM Specialty section: samples displayed a reduction of CD4+ cells (p<0.0001) and an increase of CD8+ This article was submitted to (p<0.0001), CD8+/DR+ (p<0.0001) and CD3+/CD57+ (p<0.0001) cells. Although these Hematologic Malignancies, findings were to some extent demonstrated also following bortezomib treatment, a more a section of the journal Frontiers in Oncology pronounced cytotoxic polarization was shown after exposure to autologous stem cell Received: 18 March 2021 transplantation (ASCT) and Lenalidomide (Len) treatment. -
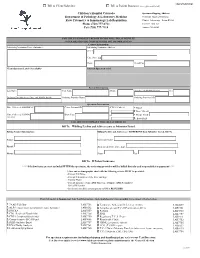
Immunology and Flow Cytometry Lab
Client/Submitter Bill to Client/Submitter Bill to Patient Insurance (see requirements below) Children's Hospital Colorado Specimen Shipping Address: Department of Pathology & Laboratory Medicine Children's Hospital Colorado Flow Cytometry & Immunology Lab Requisition Clinical Laboratory - Room B0200 Phone (720) 777-6711 13123 E. 16th Ave Fax (720) 777-7118 Aurora, CO 80045 FAILURE TO COMPLETE BELOW FIELDS WILL DELAY RESULTS ***PLEASE PROVIDE COMPLETE BILLING INFORMATION** Contact Information Submitting Institution Name (Submitter) Submitting Institution Address Street City, State, Zip Phone Result Fax Client Specimen Label (if available) Internal Specimen Label Patient Information Last Name First Name Middle I Birthdate (MM/DD/YYYY) Sex Ordering Provider (Last, First, and Middle Initial) Ordering Provider Phone Ordering Provider NPI Specimen Information Date Collected (MM/DD/YY) Client External ID ICD-10 Code(s) □ Blood 1 □ Bone Marrow Time Collected (HHMM) Draw Type 2 □ Tissue-Fresh: AM / PM 3 □ Body Fluid FAILURE TO COMPLETE WILL DELAY RESULTS Bill To: □ Billing Facility and Address same as Submitter Listed Billing Contact Information: Billing Facility and Address are DIFFERENT than Submitter Listed, Bill To: Name: ___________________________________________________________ Institution Name: _______________________________________________________ Email: ___________________________________________________________ Address (incl City, State, Zip): ______________________________________________ Phone: ___________________________________________________________ -
Overview of Flow Cytometry and Its Uses for Cell Analysis and Sorting
Principles of flow cytometry: overview of flow cytometry and its uses for cell analysis and sorting Shoreline Community College BIOL 288 Flow Cytometry • What is Flow Cytometry? – Measurement of cells or particles in a fluid stream • The first commercial cytometer was developed in 1956 (Coulter counter) • The first fluorescent based cytometer was developed in 1968. • In 1978 the term Flow Cytometry was adopted and companies began to manufacture commercial instrument systems Flow Cytometry • Flow cytometry uses fluorescent light and non-fluorescent light to categorize and quantify cells or particles. • An Instrument collects and measures multiple characteristics of individual cells within a population as they pass through a focused beam of light. • Modern flow cytometers are powerful tools; at rates of several thousand to 10’s of thousand cells per second, quantifiable data on complex mixtures can be obtained revealing the heterogeneity of a sample and its many subsets of cells. • Examples of use Immunophenotyping | Cell proliferation | Tracking proteins or genes Activation studies |Immune response | Apoptosis Cell sorting All of the above and in addition, single to multiple populations are physically separated and purified from a mixed sample for downstream assays Flow Cytometry Where is flow cytometry used? Biomedical research labs Immunology, Cancer Biology, Neurobiology, Molecular biology, Microbiology, Parasitology Diagnostic Laboratories Virology - HIV/AIDS, Hematology, Transplant and Tumor Immunology, Prenatal Diagnosis Medical Engineering Protein Engineering, Microvessicle and Nanoparticles Marine and Plant Biology Fluorescence • Fluorescent molecules emit light energy within a spectral range • Fluorescent Dyes and Proteins are selective and highly sensitive detection molecules used as markers to classify cellular properties. • Monoclonal antibodies and tetramers when coupled with fluorescent dyes can be detected using flow cytometry. -

Flow Cytometric Determination for Dengue Virus-Infected Cells: Its Application for Antibody-Dependent Enhancement Study
Flow Cytometric Determination for Dengue Virus-Infected Cells: Its Application for Antibody-Dependent Enhancement Study Kao-Jean Huang*, Yu-Ching Yang*, Yee-Shin Lin*, Hsiao-Sheng Liu*, Trai-Ming Yeh**, Shun-Hua Chen*, Ching-Chuan Liu*** and Huan-Yao Lei*! *Departments of Microbiology and Immunology, College of Medicine, National Cheng Kung University, Tainan, Taiwan **Department of Medical Technology, College of Medicine, National Cheng Kung University, Tainan, Taiwan ***Department of Pediatrics, College of Medicine, National Cheng Kung University, Tainan, Taiwan Abstract The theory of antibody-dependent enhancement plays an important role in the dengue virus infection. However, its molecular mechanism is not clearly studied partially due to lack of a sensitive assay to determine the dengue virus-infected cells. We developed a flow cytometric assay with anti-dengue antibody intracellular staining on dengue virus-infected cells. Both anti-E and anti-prM Abs could enhance the dengue virus infection. The anti-prM Ab not only enhanced the dengue virus infected cell mass, but also increased the dengue virus protein synthesis within the cells. The effect of anti-prM Ab- mediated enhancement on dengue virus infection is serotype-independent. We concluded that the target cell-based flow cytometry with anti-dengue antibody intracellular staining on dengue virus- infected cells is a sensitive assay to detect the dengue virus infected cells and to evaluate the effect of enhancing antibody on dengue virus infection on cell lines or human primary monocytes. Keywords: Dengue, enhancing antibody, ADE, flow cytometry. Introduction characterized by abnormalities of haemostasis and increased vascular permeability, which in Dengue is an acute infectious disease caused some instances results in DSS. -

Current Challenges in Providing Good Leukapheresis Products for Manufacturing of CAR-T Cells for Patients with Relapsed/Refractory NHL Or ALL
cells Article Current Challenges in Providing Good Leukapheresis Products for Manufacturing of CAR-T Cells for Patients with Relapsed/Refractory NHL or ALL Felix Korell 1,*, Sascha Laier 2, Sandra Sauer 1, Kaya Veelken 1, Hannah Hennemann 1, Maria-Luisa Schubert 1, Tim Sauer 1, Petra Pavel 2, Carsten Mueller-Tidow 1, Peter Dreger 1, Michael Schmitt 1 and Anita Schmitt 1 1 Department of Internal Medicine V, University Hospital Heidelberg, 69120 Heidelberg, Germany; [email protected] (S.S.); [email protected] (K.V.); [email protected] (H.H.); [email protected] (M.-L.S.); [email protected] (T.S.); [email protected] (C.M.-T.); [email protected] (P.D.); [email protected] (M.S.); [email protected] (A.S.) 2 Institute of Clinical Transfusion Medicine and Cell Therapy (IKTZ), 89081 Heidelberg, Germany; [email protected] (S.L.); [email protected] (P.P.) * Correspondence: [email protected] Received: 9 April 2020; Accepted: 13 May 2020; Published: 15 May 2020 Abstract: Background: T lymphocyte collection through leukapheresis is an essential step for chimeric antigen receptor T (CAR-T) cell therapy. Timing of apheresis is challenging in heavily pretreated patients who suffer from rapid progressive disease and receive T cell impairing medication. Methods: A total of 75 unstimulated leukaphereses were analyzed including 45 aphereses in patients and 30 in healthy donors. Thereof, 41 adult patients with Non-Hodgkin’s lymphoma (85%) or acute lymphoblastic leukemia (15%) underwent leukapheresis for CAR-T cell production. -

Flow Cytometry: Basic Principles and Applications
Critical Reviews in Biotechnology ISSN: 0738-8551 (Print) 1549-7801 (Online) Journal homepage: http://www.tandfonline.com/loi/ibty20 Flow cytometry: basic principles and applications Aysun Adan, Günel Alizada, Yağmur Kiraz, Yusuf Baran & Ayten Nalbant To cite this article: Aysun Adan, Günel Alizada, Yağmur Kiraz, Yusuf Baran & Ayten Nalbant (2016): Flow cytometry: basic principles and applications, Critical Reviews in Biotechnology, DOI: 10.3109/07388551.2015.1128876 To link to this article: http://dx.doi.org/10.3109/07388551.2015.1128876 Published online: 14 Jan 2016. Submit your article to this journal Article views: 364 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ibty20 Download by: [Universidad Autonoma Metropolitana] Date: 09 May 2016, At: 17:45 http://informahealthcare.com/bty ISSN: 0738-8551 (print), 1549-7801 (electronic) Crit Rev Biotechnol, Early Online: 1–14 ! 2016 Taylor & Francis. DOI: 10.3109/07388551.2015.1128876 REVIEW ARTICLE Flow cytometry: basic principles and applications Aysun Adan1*,Gu¨nel Alizada2*, Yag˘mur Kiraz1,2*, Yusuf Baran1,2, and Ayten Nalbant2 1Faculty of Life and Natural Sciences, Abdullah Gu¨l University, Kayseri, Turkey and 2Department of Molecular Biology and Genetics, I_zmir Institute of Technology, I_zmir, Turkey Abstract Keywords Flow cytometry is a sophisticated instrument measuring multiple physical characteristics of a Apoptosis, cytokines, flow cytometer, single cell such as size and granularity simultaneously as the cell flows in suspension through a fluorescence, fluorescent-activated cell measuring device. Its working depends on the light scattering features of the cells under sorting, histogram, immunophenotyping, investigation, which may be derived from dyes or monoclonal antibodies targeting either light scatter extracellular molecules located on the surface or intracellular molecules inside the cell. -

Characterization of Immunophenotyping in ALL: a Single Center Study of Western India Dr
DOI: 10.21276/sjams.2016.4.9.35 Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2016; 4(9C):3349-3354 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Original Research Article Characterization of Immunophenotyping in ALL: A Single Center Study of Western India Dr. Sandeeep K Jasuja1, Dr Sandhya Gulati2, Shraddha Patel3, Dr Nidhi Sharma4 1Asso. Professor and Head, Department of Medical Oncology, SMS MC & Attached Hospitals, Jaipur, Rajasthan, India 2Professor, Department of Pathology, SMS MC & Attached Hospitals, Jaipur, Rajasthan, India 3Observational Trainer, Department of Medical Oncology, SMS MC & Attached Hospitals, Jaipur, Rajasthan, India 4Assistant Professor, Department of Pathology, SMS MC & Attached Hospitals, Jaipur, Rajasthan, India *Corresponding author Dr. Sandeeep K Jasuja Email: [email protected] Abstract: This retrospective observational study was done among 227 ALL cases at a cancer treatment center in Western India. Data were collected retrospectively from hospital records during June 2015 to May 2016. Diagnosis of ALL was made based on the complete blood cell counts, peripheral blood smear/bone marrow aspirate smear and immunophenotyping study. Out of 227 ALL patients, 217 cases were of B-ALL, 8 cases were of T-ALL and 2 cases were of biphenotypic ALL. Of these 217 cases of B-ALL 190 (87.56) were pediatric age (range 0.5-15 years) and 27 (12.44) were adult (range 16-52 years). T-ALL cases were equally distributed in both age groups, 4 (50%) cases in pediatric age group (range 1-7 years)and 4 (50%) cases were adult (range 19-62 years). -

SY3200 Cell Sorter True Innovation Inside
SY3200 Cell Sorter true innovation inside Europe True Innovation The SY3200™ system is one of the most innovative and versatile Flow Cytometry Research platforms available in the market. True innovation drives superior performance and versatility in the SY3200 system. From optics to electronics, revolutionary technology provides solutions that enable the complex applications of today and tomorrow. Advancements in discovery of new markers and new dyes have improved the ability to identify more populations in a single assay. This has advanced the use of flow cytometry in an increasing number of applications as well as challenged instrumentation to continue to adapt to new parameters. The SY3200 has been designed to easily adapt to the ever increasing need for flexibility and sensitivity in new applications. Whereas some systems are merely evolutionary in design, the SY3200 brings revolutionary, innovative and cutting edge technology to elevate the science of flow cytometry. The innovative and flexible laser delivery array allows for ultimate laser compatibility while the unique reflective collection optics ensure maximum fluoresence collection efficiency. Powerful, Sony designed electronics enable collection of high resolution data and ultra high speed cell sorting while maintaining superior sensitivity. Plug and Play PMTs in the Scalable PMT Array (SPA) module provide the ultimate flexibility in collection options while minimizing cost. The SY3200 provides true innovation to deliver a comprehensive cell sorting solution that meets the challenges of the increasing complexity of research flow cytometry applications. Ultimate Configurability The SY3200 platform is designed for configurability to adapt to the demanding needs of a variety of sorting labs. Unique to any system in flow cytometry, the SY3200 is expandable to a dual system layout, effectively enabling two systems in one. -

Plasma-Cell-Dyscrasias-Sflc-Assay Executive
Comparative Effectiveness Review Number 73 Effective Health Care Program Serum Free Light Chain Analysis for the Diagnosis, Management, and Prognosis of Plasma Cell Dyscrasias Executive Summary Background Effective Health Care Program Plasma cell dyscrasias (PCDs) are a group The Effective Health Care Program of neoplastic disorders characterized by was initiated in 2005 to provide the uninhibited expansion of a monoclonal valid evidence about the comparative population of malignant plasma cells.1 effectiveness of different medical Multiple myeloma (MM) is the most interventions. The object is to help common malignant plasma cell tumor, consumers, health care providers, accounting for about 1 percent of all and others in making informed cancer types,1 and the second most choices among treatment alternatives. common hematologic malignancy in Through its Comparative Effectiveness the United States. With an age-adjusted Reviews, the program supports incidence rate of 5.5 cases per 100,000 systematic appraisals of existing population,2 an estimated 19,900 new scientific evidence regarding diagnoses and 10,790 deaths due to treatments for high-priority health myeloma occurred in 2007, according conditions. It also promotes and to the American Cancer Society.3 Although generates new scientific evidence by the median survival has improved to identifying gaps in existing scientific 5 years with current standards of evidence and supporting new research. treatment,4 the annual costs of modern The program puts special emphasis therapies can range from $50,000 to on translating findings into a variety $125,000 per patient.5,6 of useful formats for different In PCDs, each abnormally expanded stakeholders, including consumers.