Neurotransmitters in Health and Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Psychosis: 30 Years of Progress
Journal of Clinical Pharmacy and Therapeutics (2006) 31, 523–534 REVIEW ARTICLE Treatment of psychosis: 30 years of progress I. R. De Oliveira* MD PhD andM.F.Juruena MD *Department of Neuropsychiatry, School of Medicine, Federal University of Bahia, Salvador, BA, Brazil and Department of Psychological Medicine, Institute of Psychiatry, King’s College, University of London, London, UK phrenia. Thirty years ago, psychiatrists had few SUMMARY neuroleptics available to them. These were all Background: Thirty years ago, psychiatrists had compounds, today known as conventional anti- only a few choices of old neuroleptics available to psychotics, and all were liable to cause severe extra them, currently defined as conventional or typical pyramidal side-effects (EPS). Nowadays, new antipsychotics, as a result schizophrenics had to treatments are more ambitious, aiming not only to suffer the severe extra pyramidal side effects. improve psychotic symptoms, but also quality of Nowadays, new treatments are more ambitious, life and social reinsertion. We briefly but critically aiming not only to improve psychotic symptoms, outline the advances in diagnosis and treatment but also quality of life and social reinsertion. Our of schizophrenia, from the mid 1970s up to the objective is to briefly but critically review the present. advances in the treatment of schizophrenia with antipsychotics in the past 30 years. We conclude DIAGNOSIS OF SCHIZOPHRENIA that conventional antipsychotics still have a place when just the cost of treatment, a key factor in Up until the early 1970s, schizophrenia diagnoses poor regions, is considered. The atypical anti- remained debatable. The lack of uniform diagnostic psychotic drugs are a class of agents that have criteria led to relative rates of schizophrenia being become the most widely used to treat a variety of very different, for example, in New York and psychoses because of their superiority with London, as demonstrated in an important study regard to extra pyramidal symptoms. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

Management of Side Effects of Antipsychotics
Management of side effects of antipsychotics Oliver Freudenreich, MD, FACLP Co-Director, MGH Schizophrenia Program www.mghcme.org Disclosures I have the following relevant financial relationship with a commercial interest to disclose (recipient SELF; content SCHIZOPHRENIA): • Alkermes – Consultant honoraria (Advisory Board) • Avanir – Research grant (to institution) • Janssen – Research grant (to institution), consultant honoraria (Advisory Board) • Neurocrine – Consultant honoraria (Advisory Board) • Novartis – Consultant honoraria • Otsuka – Research grant (to institution) • Roche – Consultant honoraria • Saladax – Research grant (to institution) • Elsevier – Honoraria (medical editing) • Global Medical Education – Honoraria (CME speaker and content developer) • Medscape – Honoraria (CME speaker) • Wolters-Kluwer – Royalties (content developer) • UpToDate – Royalties, honoraria (content developer and editor) • American Psychiatric Association – Consultant honoraria (SMI Adviser) www.mghcme.org Outline • Antipsychotic side effect summary • Critical side effect management – NMS – Cardiac side effects – Gastrointestinal side effects – Clozapine black box warnings • Routine side effect management – Metabolic side effects – Motor side effects – Prolactin elevation • The man-in-the-arena algorithm www.mghcme.org Receptor profile and side effects • Alpha-1 – Hypotension: slow titration • Dopamine-2 – Dystonia: prophylactic anticholinergic – Akathisia, parkinsonism, tardive dyskinesia – Hyperprolactinemia • Histamine-1 – Sedation – Weight gain -

Sex-Specific Cannabidiol- and Iloperidone-Induced Neuronal Activity Changes in an in Vitro MAM Model System of Schizophrenia
International Journal of Molecular Sciences Article Sex-Specific Cannabidiol- and Iloperidone-Induced Neuronal Activity Changes in an In Vitro MAM Model System of Schizophrenia Rachel-Karson Thériault 1,2,†, Myles St-Denis 1,†, Tristen Hewitt 1,2, Jibran Y. Khokhar 2,3 , Jasmin Lalonde 1,2 and Melissa L. Perreault 2,3,* 1 Department of Molecular and Cellular Biology, University of Guelph, Guelph, ON N1G 2W1, Canada; [email protected] (R.-K.T.); [email protected] (M.S.-D.); [email protected] (T.H.); [email protected] (J.L.) 2 Collaborative Program in Neuroscience, University of Guelph, Guelph, ON N1G 2W1, Canada; [email protected] 3 Department of Biomedical Sciences, University of Guelph, Guelph, ON N1G 2W1, Canada * Correspondence: [email protected]; Tel.: +1-(519)-824-4120 (ext. 52013) † These authors contributed equally to this work. Abstract: Cortical circuit dysfunction is thought to be an underlying mechanism of schizophrenia (SZ) pathophysiology with normalization of aberrant circuit activity proposed as a biomarker for antipsychotic efficacy. Cannabidiol (CBD) shows potential as an adjunctive antipsychotic therapy; however, potential sex effects in these drug interactions remain unknown. In the present study, we sought to elucidate sex effects of CBD coadministration with the atypical antipsychotic iloperidone (ILO) on the activity of primary cortical neuron cultures derived from the rat methylazoxymethanol Citation: Thériault, R.-K.; St-Denis, acetate (MAM) model used for the study of SZ. Spontaneous network activity measurements were M.; Hewitt, T.; Khokhar, J.Y.; Lalonde, J.; Perreault, M.L. Sex-Specific obtained using a multielectrode array at baseline and following administration of CBD or ILO Cannabidiol- and Iloperidone- alone, or combined. -

Washington State Health Care Authority
Washington State Health Care Authority Prescription Drug Program 626 8th Ave SE, Olympia, WA 98501 ● 206-521-2029 https://www.hca.wa.gov/about-hca/prescription-drug-program February 17, 2021 Dear Interested Party, Based on recommendations by the Washington State Pharmacy and Therapeutics Committee, the Health Care Authority, Uniform Medical Plan (UMP), and the Department of Labor & Industries (L&I) have named the following drugs as preferred in their respective therapeutic classes on the Washington State Preferred Drug List (PDL), effective immediately: Antiplatelet reviewed 8/15/2018 Agency Coverage Ingredient Name Label Name of Preferred Product L&I UMP clopidogrel bisulfate clopidogrel tablet Not participating Yes The effect of this recommendation is no change to the Washington PDL. Second Generation Antipsychotics reviewed 12/18/2019 Agency Coverage Ingredient Name Label Name of Preferred Products L&I UMP aripiprazole Abilify Maintena® suspension reconstituted No Yes aripiprazole solution Yes Yes aripiprazole tablet Yes Yes aripiprazole ODT tablet dispersible Yes Yes aripiprazole lauroxil Aristada® injectable No Yes Aristada Initio® injectable No Yes asenapine maleate Saphris® sublingual Yes Yes brexpiprazole Rexulti® tablet Yes Yes cariprazine HCL Vraylar® capsule Yes Yes clozapine clozapine tablet Yes Yes clozapine ODT tablet dispersible Yes Yes iloperidone Fanapt® tablet Yes Yes Fanapt Titration Pack® tablet Yes Yes lurasidone HCL Latuda® tablet Yes Yes olanzapine olanzapine injectable No Yes olanzapine tablet Yes Yes olanzapine -

Antipsychotic Medication Reduction
So tonight we'll be discussing antipsychotic medication reduction. I'm happy to share some of my experiences with this challenging initiative and in nursing homes. I have no financial affiliations to disclose. And for our objectives and our agenda today, we're going to assess and evaluate appropriate antipsychotic medication use in nursing home residents, and apply strategies toward behavior management and antipsychotic medication reduction. The first part of the program we'll look at current trends and rates of antipsychotic medication use. We'll discuss the CMS initiative and latest policy issues. And then we'll look at a couple case studies. So first off, this first graph goes over the national progress in reducing the inappropriate use of antipsychotic medications in nursing homes. The taller red bar gives us the 2011 baseline number of 23.9%. That's a dotted red line indicates the start of the 2012 CMS initiative. That's the National Partnership to Improve Dementia Care in Nursing Homes. The latest information all the way down at the end is from the third quarter of 2018, which shows that nationally we have a 14.6% use rate. Overall, this looks like a reduction of nearly 40% since the initiative began. Overall though, I think this is great progress. Why should we be concerned with antipsychotic medications at all in this population? I have to say, that when I first exited my training from psychiatry and geriatric psychiatry, the black box warning had not yet come out. And it hit me that most of all the training that I learned was getting reversed when I entered the care setting. -

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -

Psychotropic Medication Concerns When Treating Individuals with Developmental Disabilities
Tuesday, 2:30 – 4:00, C2 Psychotropic Medication Concerns when Treating Individuals with Developmental Disabilities Richard Berchou 248-613-6716 [email protected] Objective: Identify effective methods for the practical application of concepts related to improving the delivery of services for persons with developmental disabilities Notes: Medication Assistance On-Line Resources OBTAINING MEDICATION: • Needy Meds o Needymeds.com • Partnership for Prescriptions Assistance o Pparx.org • Patient Assistance Program Center o Rxassist.org • Insurance coverage & Prior authorization forms for most drug plans o Covermymeds.com REMINDERS TO TAKE MEDICATION: • Medication reminder by Email, Phone call, or Text message o Sugaredspoon.com ANSWER MOST QUESTIONS ABOUT MEDICATIONS: • Univ. of Michigan/West Virginia Schools of Pharmacy o Justaskblue.com • Interactions between medications, over-the-counter (OTC) products and some foods; also has a pictorial Pill Identifier: May input an entire list of medications o Drugs.com OTHER TRUSTED SITES: • Patient friendly information about disease and diagnoses o Mayoclinic.com, familydoctor.org • Package inserts, boxed warnings, “Dear Doctor” letters (can sign up to receive e- mail alerts) o Dailymed.nlm.nih.gov • Communications about drug safety o www.Fda.gov/cder/drug/drugsafety/drugindex.htm • Purchasing medications on-line o Pharnacychecker.com Updated 2013 Psychotropic Medication for Persons with Developmental Disabilities April 23, 2013 Richard Berchou, Pharm. D. Assoc. Clinical Prof., Dept. Psychiatry & Behavioral -
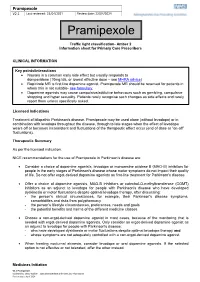
Pramipexole V2.1 Last Reviewed: 22/04/2021 Review Date: 22/04/2024
Pramipexole V2.1 Last reviewed: 22/04/2021 Review date: 22/04/2024 Pramipexole Traffic light classification- Amber 2 Information sheet for Primary Care Prescribers CLINICAL INFORMATION Key points/interactions Nausea is a common early side effect but usually responds to domperidone (10mg tds, or lowest effective dose – see MHRA advice) Ropinirole MR is first line dopamine agonist. Pramipexole MR should be reserved for patients in whom this is not suitable- see formulary. Dopamine agonists may cause compulsive/addictive behaviours such as gambling, compulsive shopping and hyper sexuality. Patients rarely recognise such changes as side effects and rarely report them unless specifically asked. Licensed Indications Treatment of idiopathic Parkinson's disease. Pramipexole may be used alone (without levodopa) or in combination with levodopa throughout the disease, through to late stages when the effect of levodopa wears off or becomes inconsistent and fluctuations of the therapeutic effect occur (end of dose or “on-off” fluctuations). Therapeutic Summary As per the licensed indication. NICE recommendations for the use of Pramipexole in Parkinson’s disease are: Consider a choice of dopamine agonists, levodopa or monoamine oxidase B (MAO-B) inhibitors for people in the early stages of Parkinson's disease whose motor symptoms do not impact their quality of life. Do not offer ergot-derived dopamine agonists as first-line treatment for Parkinson's disease. Offer a choice of dopamine agonists, MAO-B inhibitors or catechol-O-methyltransferase (COMT) -

Efficacy of Antimanic Treatments: Meta-Analysis of Randomized, Controlled Trials
Neuropsychopharmacology (2011) 36, 375–389 & 2011 American College of Neuropsychopharmacology. All rights reserved 0893-133X/11 $32.00 www.neuropsychopharmacology.org Efficacy of Antimanic Treatments: Meta-analysis of Randomized, Controlled Trials ,1,2 2,3 4 2 Ays¸egu¨l Yildiz* , Eduard Vieta , Stefan Leucht and Ross J Baldessarini 1 2 Department of Psychiatry, Dokuz Eylu¨l University, Izmir, Turkey; Department of Psychiatry, Harvard Medical School and International Consortium for Bipolar Disorder Research and Psychopharmacology Program, McLean Division of Massachusetts General Hospital, Boston, 3 Massachusetts; Bipolar Disorders Program, Institute of Clinical Neuroscience, Hospital Clinic, University of Barcelona, IDIBAPS, CIBERSAM, 4 Barcelona, Spain; Department of Psychiatry and Psychotherapy, Klinik fu¨r Psychiatrie und Psychotherapie der TU-Mu¨nchen, Klinikum rechts der Isar, Technische Universita¨t Mu¨nchen, Mu¨nchen, Germany We conducted meta-analyses of findings from randomized, placebo-controlled, short-term trials for acute mania in manic or mixed states of DSM (III–IV) bipolar I disorder in 56 drug–placebo comparisons of 17 agents from 38 studies involving 10 800 patients. Of drugs tested, 13 (76%) were more effective than placebo: aripiprazole, asenapine, carbamazepine, cariprazine, haloperidol, lithium, olanzapine, paliperdone, quetiapine, risperidone, tamoxifen, valproate, and ziprasidone. Their pooled effect size for mania improvement (Hedges’ g in 48 trials) was 0.42 (confidence interval (CI): 0.36–0.48); pooled responder risk ratio (46 trials) was 1.52 (CI: 1.42–1.62); responder rate difference (RD) was 17% (drug: 48%, placebo: 31%), yielding an estimated number-needed-to-treat of 6 (all po0.0001). In several direct comparisons, responses to various antipsychotics were somewhat greater or more rapid than lithium, valproate, or carbamazepine; lithium did not differ from valproate, nor did second generation antipsychotics differ from haloperidol. -

CHAPTER 6 Sleep and Stroke G.J
CHAPTER 6 Sleep and Stroke G.J. Meskill*, C. Guilleminault** *Comprehensive Sleep Medicine Associates, Houston, TX, USA **The Stanford Center for Sleep Sciences and Medicine, Redwood City, CA, USA OUTLINE Introduction 115 Stroke, Parasomnias, and Sleep- Related Movement Disorders 120 Sleep Apnea is a Risk Factor for Stroke 115 Diagnosis 120 Pathophysiology 116 Treatment 122 Stroke Increases the Risk of Sleep Apnea 118 Conclusions 123 Stroke and the Sleep–Wake Cycle 118 References 124 INTRODUCTION Stroke, defined as a focal neurological deficit of acute onset and vascular origin, is the sec- ond leading cause of death worldwide and is a major source of physical, psychological, and monetary hardship. There are more than 15 million cases worldwide annually, and 795,000 in the United States alone. In total, 137,000 stroke patients will die from stroke complications, and more than 50% will have physical and mental impairment.1 Factoring healthcare services, medications, and productivity loss, strokes cost the United States $34 billion annually.2 SLEEP APNEA IS A RISK FACTOR FOR STROKE Obstructive sleep apnea (OSA) is characterized by recurrent episodes of partial or complete interruption in breathing during sleep due to increased upper airway resistance. OSA has been identified as an independent risk factor for several cardiovascular and cerebrovascular Sleep and Neurologic Disease. http://dx.doi.org/10.1016/B978-0-12-804074-4.00006-6 Copyright © 2017 Elsevier Inc. All rights reserved. 115 116 6. SLEEP AND STROKE morbidities, including hypertension, ischemic heart disease, heart failure, atrial fibrillation, and hypertrophic cardiomyopathy.3–6 The incidence of OSA varies due to significant differ- ences in the sensitivity of testing sites, testing modalities (e.g., in-laboratory polysomnog- raphy vs. -

List Item Pramipexole Teva
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Pramipexole Teva 0.088 mg tablets Pramipexole Teva 0.18 mg tablets Pramipexole Teva 0.35 mg tablets Pramipexole Teva 0.7 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Pramipexole Teva 0.088 mg tablets Each tablet contains 0.125 mg pramipexole dihydrochloride monohydrate equivalent to 0.088 mg pramipexole. Pramipexole Teva 0.18 mg tablets Each tablet contains 0.25 mg pramipexole dihydrochloride monohydrate equivalent to 0.18 mg pramipexole. Pramipexole Teva 0.35 mg tablets Each tablet contains 0.5 mg pramipexole dihydrochloride monohydrate equivalent to 0.35 mg pramipexole. Pramipexole Teva 0.7 mg tablets Each tablet contains 1.0 mg pramipexole dihydrochloride monohydrate equivalent to 0.7 mg pramipexole. Please note: Pramipexole doses as published in the literature refer to the salt form. Therefore, doses will be expressed in terms of both pramipexole base and pramipexole salt (in brackets). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Tablet Pramipexole Teva 0.088 mg tablets White, round, flat face bevel edge tablet, 5.55 mm diameter, embossed with “93” on one side and “P1” on the other side. Pramipexole Teva 0.18 mg tablets White, round, flat face bevel edge tablet, 7.00 mm diameter, embossed with "P2" over "P2" on the scored side and "93" on the other side. The tablet can be divided into equal halves. Pramipexole Teva 0.35 mg tablets White to off-white, oval, biconvex tablets, engraved with 9 vertical scoreline 3 on the scored side, and 8023 on the other side.