Supplementary File
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Research Article RP-HPLC Method for Determination of Several Nsaids and Their Combination Drugs
Hindawi Publishing Corporation Chromatography Research International Volume 2013, Article ID 242868, 13 pages http://dx.doi.org/10.1155/2013/242868 Research Article RP-HPLC Method for Determination of Several NSAIDs and Their Combination Drugs Prinesh N. Patel, Gananadhamu Samanthula, Vishalkumar Shrigod, Sudipkumar C. Modh, and Jainishkumar R. Chaudhari Department of Pharmaceutical Analysis, National Institute of Pharmaceutical Education and Research (NIPER), Balanagar, Hyderabad, Andhra Pradesh 500037, India Correspondence should be addressed to Gananadhamu Samanthula; [email protected] Received 29 June 2013; Accepted 13 October 2013 Academic Editor: Andrew Shalliker Copyright © 2013 Prinesh N. Patel et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. An RP-HPLC method for simultaneous determination of 9 NSAIDs (paracetamol, salicylic acid, ibuprofen, naproxen, aceclofenac, diclofenac, ketorolac, etoricoxib, and aspirin) and their commonly prescribed combination drugs (thiocolchicoside, moxifloxacin, clopidogrel, chlorpheniramine maleate, dextromethorphan, and domperidone) was established. The separation was performed on ∘ Kromasil C18 (250 × 4.6 mm, 5 m) at 35 C using 15 mM phosphate buffer pH 3.25 and acetonitrile with gradient elution ata flow rate of 1.1 mL/min. The detection was performed by a diode array detector (DAD) at 230 nm with total run time of 30min. 2 Calibration curves were linear with correlation coefficients of determinationr ( ) > 0.999. Limit of detection (LOD) and Limit of quantification (LOQ) ranged from 0.04 to 0.97 g/mL and from 0.64 to 3.24 g/mL, respectively. -

01012100 Pure-Bred Horses 0 0 0 0 0 01012900 Lives Horses, Except
AR BR UY Mercosu PY applied NCM Description applied applied applied r Final Comments tariff tariff tariff tariff Offer 01012100 Pure-bred horses 0 0 0 0 0 01012900 Lives horses, except pure-bred breeding 2 2 2 2 0 01013000 Asses, pure-bred breeding 4 4 4 4 4 01019000 Asses, except pure-bred breeding 4 4 4 4 4 01022110 Purebred breeding cattle, pregnant or lactating 0 0 0 0 0 01022190 Other pure-bred cattle, for breeding 0 0 0 0 0 Other bovine animals for breeding,pregnant or 01022911 lactating 2 2 2 2 0 01022919 Other bovine animals for breeding 2 2 2 2 4 01022990 Other live catlle 2 2 2 2 0 01023110 Pure-bred breeding buffalo, pregnant or lactating 0 0 0 0 0 01023190 Other pure-bred breeding buffalo 0 0 0 0 0 Other buffalo for breeding, ex. pure-bred or 01023911 pregnant 2 2 2 2 0 Other buffalo for breeding, except pure-bred 01023919 breeding 2 2 2 2 4 01023990 Other buffalos 2 2 2 2 0 01029000 Other live animals of bovine species 0 0 0 0 0 01031000 Pure-bred breedig swines 0 0 0 0 0 01039100 Other live swine, weighing less than 50 kg 2 2 2 2 0 01039200 Other live swine, weighing 50 kg or more 2 2 2 2 0 01041011 Pure-bred breeding, pregnant or lactating, sheep 0 0 0 0 0 01041019 Other pure-bred breeding sheep 0 0 0 0 0 01041090 Others live sheep 2 2 2 2 0 01042010 Pure-bred breeding goats 0 0 0 0 0 01042090 Other live goats 2 2 2 2 0 Fowls spec.gallus domestic.w<=185g pure-bred 01051110 breeding 0 0 0 0 0 Oth.live fowls spec.gall.domest.weig.not more than 01051190 185g 2 2 2 2 0 01051200 Live turkeys, weighing not more than 185g 2 2 -

Comparative Study of the Efficacy of Flunixin, Ketoprofen and Phenylbutazone in Delman Horses with Mild Colic
Sys Rev Pharm 2020; 11(5): 464 468 A multifaceted review journal in the field of pharmacy E-ISSN 0976-2779 P-ISSN 0975-8453 Comparative Study of the Efficacy of Flunixin, Ketoprofen and Phenylbutazone in Delman Horses with Mild Colic Agus Purnomo1, Arya Pradana Wicaksono2, Dodit Hendrawan2, Muhammad Thohawi Elziyad Purnama3* 1Department of Veterinary Surgery and Radiology, Faculty of Veterinary Medicine, Universitas Gadjah Mada, DI Yogyakarta, 55281, Indonesia 2Postgraduate Studies, Faculty of Veterinary Medicine, Universitas Airlangga, Surabaya, 60115, Indonesia 3Department of Veterinary Anatomy, Faculty of Veterinary Medicine, Universitas Airlangga, Surabaya, 60115, Indonesia *Corresponding author E-mail: [email protected] Article History: Submitted: 26.02.2020 Revised: 16.04.2020 Accepted: 21.05.2020 ABSTRACT This study aimed to evaluate the efficacy of flunixin, ketoprofen and multiple range test. The results showed a significant alleviation in all phenylbutazone on serum biochemistry, plasma catecholamines and observed variables on Day 13, although the use of various NSAIDs serum cortisol in Delman horses with mild colic. During the study showed no significant difference. period, 32 horses were evaluated due to mild colic. Flunixin, Keywords: serum biochemical, catecholamine, cortisol, colic, NSAIDs ketoprofen, and phenylbutazone were administered intravenously at Correspondence: the recommended dose rates of 1.0; 2.2 and 4.4 mg/kg, respectively. Muhammad Thohawi Elziyad Purnama Administration of the NSAIDs commenced on Day 1 and continued Department of Veterinary Anatomy, Faculty of Veterinary Medicine, every 12 h for 12 days. Blood samples collected between days 2, 5, 9 Universitas Airlangga, Surabaya, 60115, Indonesia and 13 to evaluate AST, ALP, GGT, creatinine, urea, epinephrine, E-mail: [email protected] norepinephrine, and cortisol level. -

Nicolau Syndrome: a Review of Case Studies, Pharm Sci
The following manuscript was accepted for publication in Pharmaceutical Sciences. It is assigned to an issue after technical editing, formatting for publication and author proofing. Citation: Mojarrad P, Mollazadeh H, Barikbin B, Oghazian MB. Nicolau syndrome: a review of case studies, Pharm Sci. 2021, doi: 10.34172/PS.2021.32 Nicolau syndrome: a review of case studies Paria Mojarrad1, Hamid Mollazadeh2,3, Behnaz Barikbin1, Mohammad Bagher Oghazian4,1* 1 Clinical Research Development Unit, Imam Hasan Hospital, North Khorasan University of Medical Sciences, Bojnurd, Iran 2 Department of Physiology and Pharmacology, North Khorasan University of Medical Sciences, Bojnurd, Iran 3 Natural Product and Medicinal Plant Research Center, North Khorasan University of Medical Sciences, Bojnurd, Iran 4 Department of Internal Medicine, Faculty of Medicine, North Khorasan University of Medical Sciences, Bojnurd, Iran *Corresponding author: Mohammad Bagher Oghazian, Tel: +989151087370.Email: [email protected] Pharmaceutical Sciences (Indexed in ISI and Scopus) https://ps.tbzmed.ac.ir Abstract Nicolau syndrome, although it is quite rare, often occurs following intramuscular injections of different medications, especially diclofenac and penicillins. Accordingly, its symptoms usually begin with severe pain during injection, leading to ulceration and necrosis of the local tissue over time. Immediate diagnosis and treatment in the case of this syndrome, are of great importance. There are no established criteria for Nicolau's diagnosis, and preferably, these can be achieved by examining the patient's symptoms and eliminating differential diagnoses. The proposed treatments are primarily symptomatic therapy and measures such as fasciotomy, debridement, and plastic surgery provided in the affected area. The exact cause of this syndrome has not been determined yet. -

18 Analgesics Anti-Inflammatory Drugs and Antipyretics the Dosage of Alfentanil Used Depends on Whether the 2
18 Analgesics Anti-inflammatory Drugs and Antipyretics The dosage of alfentanil used depends on whether the 2. Virkkilä M, et al. Pharmacokinetics and effects of i.m. alfentanil minutes). However, some considered that there was no over- patient has spontaneous respiration or assisted ventila- as premedication for day-case ophthalmic surgery in elderly pa- all advantage of epidural over intravenous alfentanil either as tients. Br J Anaesth 1993; 71: 507–11. patient-controlled analgesia2 or by continuous infusion.3 tion and on the expected duration of anaesthesia. Doses 3. Hughes DA, Hill DA. Intrathecal alfentanil with and without bupivacaine for analgesia in labour. Anaesthesia 2000; 55: 1. Chrubasik J, et al. Relative analgesic potency of epidural fenta- are adjusted according to the needs of the patient. Chil- 1116–21. nyl, alfentanil, and morphine in treatment of postoperative pain. dren may require higher or more frequent doses than Anesthesiology 1988; 68: 929–33. Administration in children. Alfentanil is licensed in the UK 2. Chauvin M, et al. Equivalence of postoperative analgesia with adults, whereas the elderly or debilitated patients may for use in ventilated children during surgical procedures as an patient-controlled intravenous or epidural alfentanil. Anesth An- require lower or less frequent doses. Obese patients analgesic and adjunct to general anaesthetics or as a primary an- alg 1993; 76: 1251–8. may require doses based on their ideal (lean) body- aesthetic. When used as an adjunct in the maintenance of gen- 3. van den Nieuwenhuyzen MCO, et al. Epidural vs intravenous infusion of alfentanil in the management of postoperative pain weight. -

Non Steroidal Anti-Inflammatory Drugs
Non Steroidal Anti‐inflammatory Drugs (NSAIDs) 4 signs of inflammation • Redness ‐ due to local vessel dilatation • Heat ‐ due to local vessel dilatation • Swelling – due to influx of plasma proteins and phagocytic cells into the tissue spaces • Pain – due to local release of enzymes and increased tissue pressure NSAIDs • Cause relief of pain ‐. analgesic • Suppress the signs and symptoms of inflammation. • Exert antipyretic action. • Useful in pain related to inflammation. Esp for superficial/integumental pain . Classification of NSAIDs • Salicylates: aspirin, Sodium salicylate & diflunisal. • Propionic acid derivatives: ibuprofen, ketoprofen, naproxen. • Aryl acetic acid derivatives: diclofenac, ketorolac • Indole derivatives: indomethacin, sulindac • Alkanones: Nabumetone. • Oxicams: piroxicam, tenoxicam Classification of NSAIDs ….. • Anthranilic acid derivatives (fenamates): mefenamic acid and flufenamic acid. • Pyrazolone derivatives: phenylbutazone, oxyphenbutazone, azapropazone (apazone) & dipyrone (novalgine). • Aniline derivatives (analgesic only): paracetamol. Clinical Classif. • Non selective Irreversible COX inhibitors • Non slective Reversible COX inhibitors • Preferential COX 2 inhibitors • 10‐20 fold cox 2 selective • meloxicam, etodolac, nabumetone • Selective COX 2 inhibitors • > 50 fold COX ‐2 selective • Celecoxib, Etoricoxib, Rofecoxib, Valdecoxib • COX 3 Inhibitor? PCM Cyclooxygenase‐1 (COX‐1): -constitutively expressed in wide variety of cells all over the body. -"housekeeping enzyme" -ex. gastric cytoprotection, hemostasis Cyclooxygenase‐2 (COX‐2): -inducible enzyme -dramatically up-regulated during inflammation (10-18X) -constitutive : maintains renal blood flow and renal electrolyte homeostasis Salicylates Acetyl salicylic acid (aspirin). Kinetics: • Well absorbed from the stomach, more from upper small intestine. • Distributed all over the body, 50‐80% bound to plasma protein (albumin). • Metabolized to acetic acid and salicylates (active metabolite). • Salicylate is conjugated with glucuronic acid and glycine. • Excreted by the kidney. -

Discovery of Novel Pyridazine-Based Cyclooxygenase-2 Inhibitors with a Promising Gastric Safety Profile
molecules Article Discovery of Novel Pyridazine-Based Cyclooxygenase-2 Inhibitors with a Promising Gastric Safety Profile Abida Khan 1,* , Anupama Diwan 1, Hamdy Kh. Thabet 2, Mohd Imran 3 and Md. Afroz Bakht 4 1 School of Pharmaceutical Sciences, Apeejay Stya University, Sohna - Palwal Road, Sohna 122103, India; [email protected] 2 Department of Chemistry, Faculty of Arts and Science, Northern Border University, Rafha 91911, Saudi Arabia; [email protected] 3 Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Northern Border University, Rafha 91911, Saudi Arabia; [email protected] 4 Department of Chemistry, College of Science and Humanities, Prince Sattam Bin Abdulaziz University, Al-Kharj 11942, Saudi Arabia; [email protected] * Correspondence: [email protected]; Tel.: +91-8053027613 Received: 25 March 2020; Accepted: 21 April 2020; Published: 25 April 2020 Abstract: Cyclooxygenase-2 (COX-2) is implicated in the development of chronic inflammatory diseases. Recently, pyridazine derivatives have emerged as a novel prototype to develop COX-2 inhibitors. Accordingly, some pyridazine-based COX-2 inhibitors are reported herein. The reaction of aldehyde 3 and different hydrazines yielded the corresponding hydrazones. The hydrazones were further derivatized to the title compounds, which were assessed for COX-1 and COX-2 inhibitory action, gastric ulcerogenic effects, and lipid peroxidation properties. Molecular docking studies and determination of the physicochemical parameters were also carried out. The allocated structures of the reported compounds were coherent with their spectroscopic data. The compounds 9a (IC50 = 15.50 nM, 114.77%), 9b (IC50 = 17.50 nM, 101.65%), 12 (IC50 = 17.10 nM, 104.03%), 16b (IC50 = 16.90 nM, 105.26%), and 17 (IC50 = 17.70 nM, 100.5%) displayed better COX-2 inhibition than celecoxib (IC50 = 17.79 nM, 100%). -
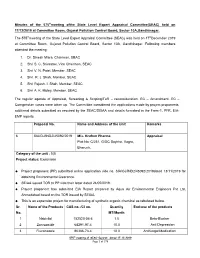
Minutes of the 575Thmeeting Ofthe State
Minutes of the 575th meeting ofthe State Level Expert Appraisal Committee(SEAC) held on 17/12/2019 at Committee Room, Gujarat Pollution Control Board, Sector 10A,Gandhinagar. The 575th meeting of the State Level Expert Appraisal Committee (SEAC) was held on 17 th December 2019 at Committee Room, Gujarat Pollution Control Board, Sector 10A, Gandhinagar. Following members attended the meeting: 1. Dr. Dinesh Misra, Chairman, SEAC 2. Shri S. C. Srivastav, Vice Chairman, SEAC 3. Shri V. N. Patel, Member, SEAC 4. Shri. R. J. Shah, Member, SEAC 5. Shri Rajesh. I. Shah, Member, SEAC 6. Shri A. K. Muley, Member, SEAC The regular agenda of Appraisal, Screening & Scoping/ToR – reconsideration, EC – Amendment, EC – Corrigendum cases were taken up. The Committee considered the applications made by project proponents, additional details submitted as required by the SEAC/SEIAA and details furnished in the Form-1, PFR, EIA- EMP reports. Proposal No. Name and Address of the Unit Remarks 6 SIA/GJ/IND2/45092/2019 M/s. Krufren Pharma Appraisal Plot No: C/251, GIDC Saykha, Vagra, Bharuch. Category of the unit : 5(f) Project status: Expansion • Project proponent (PP) submitted online application vide no. SIA/GJ/IND2/45092/2019dated 13/11/2019 for obtaining Environmental Clearance. • SEIAA issued TOR to PP vide their letter dated 24/05/2019. • Project proponent has submitted EIA Report prepared by Aqua Air Environmental Engineers Pvt Ltd, Ahmedabad based on the TOR issued by SEIAA. • This is an expansion project for manufacturing of synthetic organic chemical as tabulated below. Sr. Name of the Products CAS no. -

ANNEXURE Ii- Consolidated List of Unapproved List Licenced
Fixed dose combinations – declared unapproved by Drug Controller General of India Sl No Name of fixed dose combinations 1. 5 - bromosalicyl - 4 - chloranilide + Salicylic acid 2. * Aceclofenac + paracetamol + Chlorzoxazone 3. * Aceclofenac + Paracetamol + Serratiopeptidase 4. * Aceclofenac + Paracetamol + Tizanidine 5. * Aceclofenac + Paracetamol + Tramadol 6. Aceclofenac + Serratiopeptidase 7. Aceclofenac + Tramadol 8. Acetaminophen + Codine phosphate 9. Acetyl Salicylic acid + Ethoheptazine 10. Choline Bitartrate + Pyndoxine + Folic Acid + Vitamin E + Cyanocobalamin + Vitamin E + Cyanocobalamin + Vitamin E + Cyanocobalamin + Chromium Nicotmate + Manganese Sulfate + Zinc Sulfate" 11. Acriflavine + Gentian violet + Brilliant green 12. * Activated charcoal + Fungal distase + Lactic acid 13. Adepalene + Methyl Paraben 14. Adenocyl Cobalamine + Carbonyl lon + Folic Acid + Zinc Ascorbate 15. Adenocyl Cobalamine + Carbonyl Iron + Folic acid 16. Alendronate sodium + Calcium Carbonate + Vit - D3 17. Alendronate sodium + Chlicalceferol f+ Calcium Citrate + Magnesium Hydroxide 18. Allantoin + Dimethicone + Metylparaben + Propylparaben 19. Allantoin + Triclosan + Vit - E + Zinc Oxide 20. Allantoin + Vit - E + Cammelina Sinensis 21. Allobarbitone + Phospho - dimethyl - isopropyl - pyrazolone 22. Aloe extract + allantocin + Alfa tocoferal acetate + D-panthemol + Vita-A 23. Aloe extract + Vit - E + Dimethicone + Glycerine 24. Aloe vera + Jojoba oil + Vit - E 25. Aloe vera + Orange oil 26. Aloe vera + Vit-e acetate 27. Aloe + tocopherol 28. Aloevera -

RP-HPLC Method for Determination of Several Nsaids and Their Combination Drugs
Hindawi Publishing Corporation Chromatography Research International Volume 2013, Article ID 242868, 13 pages http://dx.doi.org/10.1155/2013/242868 Research Article RP-HPLC Method for Determination of Several NSAIDs and Their Combination Drugs Prinesh N. Patel, Gananadhamu Samanthula, Vishalkumar Shrigod, Sudipkumar C. Modh, and Jainishkumar R. Chaudhari Department of Pharmaceutical Analysis, National Institute of Pharmaceutical Education and Research (NIPER), Balanagar, Hyderabad, Andhra Pradesh 500037, India Correspondence should be addressed to Gananadhamu Samanthula; [email protected] Received 29 June 2013; Accepted 13 October 2013 Academic Editor: Andrew Shalliker Copyright © 2013 Prinesh N. Patel et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. An RP-HPLC method for simultaneous determination of 9 NSAIDs (paracetamol, salicylic acid, ibuprofen, naproxen, aceclofenac, diclofenac, ketorolac, etoricoxib, and aspirin) and their commonly prescribed combination drugs (thiocolchicoside, moxifloxacin, clopidogrel, chlorpheniramine maleate, dextromethorphan, and domperidone) was established. The separation was performed on ∘ Kromasil C18 (250 × 4.6 mm, 5 m) at 35 C using 15 mM phosphate buffer pH 3.25 and acetonitrile with gradient elution ata flow rate of 1.1 mL/min. The detection was performed by a diode array detector (DAD) at 230 nm with total run time of 30min. 2 Calibration curves were linear with correlation coefficients of determinationr ( ) > 0.999. Limit of detection (LOD) and Limit of quantification (LOQ) ranged from 0.04 to 0.97 g/mL and from 0.64 to 3.24 g/mL, respectively. -

Strategies for Chemical Synthesis of Pyrazolone Derivatives and Their Bio-Significance
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2016, 8(5):969-981 ISSN : 0975-7384 CODEN(USA) : JCPRC5 Strategies for chemical synthesis of pyrazolone derivatives and their bio-significance Sanjeev Dhawan 1, Rakesh Narang 2, Gopal L. Khatik 2, Harish Kumar Chopra 3 and Surendra Kumar Nayak 2* 1Jubilant Chemsys (Jubilant Life Sciences Ltd) 1A, Sector 16A, Noida (Uttar Pradesh)-201301, India 2Department of Pharmaceutical Chemistry, School of Pharmaceutical Sciences, Lovely Professional University, Phagwara (Punjab)-144411, India 3Department of Chemistry, Sant Longowal Institute of Engineering & Technology (Deemed University), Longowal, Sangrur (Punjab)-148106, India _____________________________________________________________________________________________ ABSTRACT Over the last few decades, pyrazolone derivatives have been used for various biochemical applications. Some of these derivatives such as metamizole, phenazone, aminopyrine and propyphenazone, are widely used as anti- inflammatory and analgesics. Moreover, pyrazolones have been exhibited antioxidant, antibacterial, anticancer and several other biological activities. Thus, keeping in view of their importance, synthetic strategies for existing as well as novel pyrazolone derivatives have been developed and explored their biochemical utility. As versatile features of pyrozaolones have emerged, so the aim of the present paper is to put chemical synthetic schemes and biological advancements of pyrazolone derivatives together. Keywords : Pyrazolones, -

Veterinary Kinsights
Veterinary KINsights Fever: Pathways and Antipyretic Mechanisms INTRODUCTION Fever (pyrexia) is defined as "a state of elevated core temperature, which is often, but not necessarily part of the defensive response of multicellular organisms (hosts) to the invasion of live (microorganisms) or inanimate matter recognized as pathogenic or alien by the host."1 Pyrexia is the body's endogenous response to infectious, inflammatory, and other processes which trigger the release of cytokines and pyrogens.2 While pyrexia is something equine practitioners deal with on a weekly basis, when choosing if and how to control fever, it is worth taking a deeper look at how commonly used drugs affect the fever pathways. Daniel J. Dreyfuss, DVM, MA FEVER PATHWAYS The most commonly understood pathway leading to fever involves cyclooxygenase (COX) and prostaglandins. Transported via the bloodstream, cytokines reach the preoptic-anterior hypothalamus (POAH), binding to specific receptors on neurons and endothelial cells in the area proximal to the organum vasculosum lamina terminalis (OVLT). Pyrogens- either endogenous or exogenous- activate and upregulate phospholipase A2, promoting the release of arachidonic acid. Additionally, the cytokines upregulate cyclooxygenase (COX) which catalyzes the conversion of arachidonic acid to prostaglandin E2 (PGE2). The PGE2 can then bind to E-type prostaglandin receptors, (EP-receptors), on the hypothalamus—specifically EP-3 receptors— resulting in the neuronal signaling leading to elevation of the hypothalamic set point. The elevation of the set point in the hypothalamic thermoregulatory center initiates a chain of events resulting in both behavioral and physiological responses generating and conserving body heat.3,4 This is fever. NEWLY REVEALED PATHWAYS Two additional pathways have been uncovered relatively recently, within the last 25 years, that also contribute to the generation of fever.