3 CMJ Original Article 9-14 Corr.Pmd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

World Bank Document
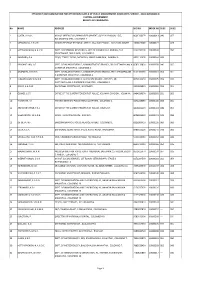
PROCUREMENT PLAN (Textual Part)P163742 Project information: [country] [Project name] [P-number]Sri Lanka – Climate Smart Irrigated Agriculture Project – P163742 Project Implementation agency: [insert legal name]Ministry of Public Disclosure Authorized Agriculture Date of the Procurement Plan: 24 January, 2019[insert date] Period covered by this Procurement Plan: [insert from – to period]24 January - 31 December 2019 Preamble In accordance with paragraph 5.9 of the “World Bank Procurement Regulations for IPF Borrowers” (July 2016) (“Procurement Regulations”) the Bank’s Systematic Tracking and Exchanges in Procurement (STEP) system will be Public Disclosure Authorized used to prepare, clear and update Procurement Plans and conduct all procurement transactions for the Project. This textual part along with the Procurement Plan tables in STEP constitute the Procurement Plan for the Project. The following conditions apply to all procurement activities in the Procurement Plan. The other elements of the Procurement Plan as required under paragraph 4.4 of the Procurement Regulations are set forth in STEP. The Bank’s Standard Procurement Documents: shall be used for all contracts subject to international competitive procurement and those Public Disclosure Authorized contracts as specified in the Procurement Plan tables in STEP. National Procurement Arrangements: : In accordance with the Procurement Regulations for IPF Borrowers (July 2016, revised November 2017) (“Procurement Regulations”), when approaching the national market, as agreed in the Procurement Plan tables in STEP, the country’s own procurement procedures may be used. When the Borrower, for the procurement of goods, works and non-consulting services, uses its own national open competitive procurement arrangements as set forth in Sri Lanka’s Procurement Guidelines 2006, such arrangements shall be subject to paragraph 5.4 of the Bank’s Procurement Regulations and the following conditions: Public Disclosure Authorized 1. -

Para Examen República Socialista Democrática De Sri Lanka Evaluación De La Estrategia Y El Programa En El País
Signatura: EC 2019/105/W.P.2 Tema: 3 Fecha: 30 de mayo de 2019 S Distribución: Pública Original Inglés República Socialista Democrática de Sri Lanka Evaluación de la estrategia y el programa en el país Nota para los miembros del Comité de Evaluación Funcionarios de contacto: Preguntas técnicas: Envío de documentación: Oscar A. Garcia Deirdre McGrenra Director Jefa Oficina de Evaluación Independiente del FIDA Unidad de los Órganos Rectores Tel.: (+39) 06 5459 2274 Tel.: (+39) 06 5459 2374 Correo electrónico: [email protected] Correo electrónico: [email protected] Fumiko Nakai Oficial Superior de Evaluación Oficina de Evaluación Independiente del FIDA Tel.: (+39) 06 5459 2283 Correo electrónico: [email protected] Comité de Evaluación — 105.o período de sesiones Roma, 19 de junio de 2019 Para examen EC 2019/105/W.P.2 Índice Agradecimientos ii Resumen iii Apéndices I. Agreement at completion point 1 II. Main report: Sri Lanka – Country Strategy and Programme Evaluation 7 i EC 2019/105/W.P.2 Agradecimientos Esta evaluación de la estrategia y el programa en el país ha estado dirigida por Fumiko Nakai, Oficial Superior de Evaluación y evaluadora principal de la Oficina de Evaluación Independiente del FIDA (IOE), con las aportaciones de Nihal Fernando (consultor en riego y gestión del agua, y adaptación al cambio climático); Jegatheeswary Gunasingam (consultora en gestión de recursos costeros y desarrollo de comunidades costeras); Nanda Karunagoda (consultor en financiación rural y microfinanciación); Susil Liyanarachchi (consultor en agricultura en pequeña escala, medios de vida rurales y género); Shijie Yang (Analista de Investigación en Evaluación de la IOE sobre datos sobre el impacto en la pobreza rural y eficiencia), y David Young (consultor superior en evaluación del rendimiento de la cartera de proyectos). -

47381-002: North Western Province Canal Project Resettlement Plan
Resettlement Plan March 2015 SRI: Mahaweli Water Security Investment Program This resettlement plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Sri Lanka Project Number: 47381 March 2015 Sri Lanka: Mahaweli Water Security Investment Program North Western Province Canal Project Tranche 1 Resettlement Implementation Plan Ministry of Mahaweli Development and Environment Democratic Socialist Republic of Sri Lanka This resettlement implementation plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or Staff. CONTENTS Page Executive Summary i I. PROJECT DESCRIPTION 1 A. Background 1 B. Rationale of the Project 2 C. Project Description and Location 3 D. Avoidance of Resettlement Impacts 3 II. SCOPE OF LAND ACQUISITION 7 A. Condition of the Building Structures 7 B. Affected Trees 8 C. Access to Land and Properties 8 D. Acquisition of Special Properties 10 E. Land Values 11 F. Resettlement options 11 III. SOCIO-ECONOMIC INFORMATION AND PROFILE OF PROJECT AREA 12 A. Population 12 B. Occupations 13 C. Infrastructure Facilities in the Project Area 14 D. -
EB PMAS Class 2 2011 2.Pdf
EFFICIENCY BAR EXAMINATION FOR OFFICERS IN CLASS II OF PUBLIC MANAGEMENT ASSISTANT'S SERVICE - 2011(II)2013(2014) CENTRAL GOVERNMENT RESULTS OF CANDIDATES No NAME ADDRESS NIC NO INDEX NO SUB1 SUB2 1 COSTA, K.A.G.C. M/Y OF DEFENCE & URBAN DEVELOPMENT, SUPPLY DIVISION, 15/5, 860170337V 10000013 040 057 BALADAKSHA MW, COLOMBO 3. 2 MEDAGODA, G.R.U.K. INLAND REVENUE REGIONAL OFFICE, 334, GALLE ROAD, KALUTARA SOUTH. 745802338V 10000027 --- 024 3 HETTIARACHCHI, H.A.S.W. DEPT. OF EXTERNAL RESOURCES, M/Y OF FINANCE & PLANNING, THE 823273010V 10000030 --- 050 SECRETARIAT, 3RD FLOOR, COLOMBO 1. 4 BANDARA, P.A. 230/4, TEMPLE ROAD, BATAPOLA, MADELGAMUWA, GAMPAHA. 682113260V 10000044 ABS --- 5 PRASANTHIKA, L.G. DEPT. OF INLAND REVENUE, ADMINISTRATIVE BRANCH, SRI CHITTAMPALAM A 858513383V 10000058 040 055 GARDINER MAWATHA, COLOMBO 2. 6 ATAPATTU, D.M.D.S. DEPT. OF INLAND REVENUE, ADMINISTRATION BRANCH, SRI CHITTAMPALAM 816130069V 10000061 054 051 A GARDINER MAWATHA, COLOMBO 2. 7 KUMARIHAMI, W.M.S.N. DEPT. OF INLAND REVENUE, ACCOUNTS BRANCH, POB 515, SRI 867010025V 10000075 059 070 CHITTAMPALAM A GARDINER MAWATHA, COLOMBO 2. 8 JENAT, A.A.D.M. DIVISIONAL SECRETARIAT, NEGOMBO. 685060892V 10000089 034 051 9 GOMES, J.S.T. OFFICE OF THE SUPERINTENDENT OF POLICE, KELANIYA DIVISION, KELANIYA. 846453857V 10000092 031 052 10 HARSHANI, A.I. FINANCE BRANCH, POLICE HEAD QUARTERS, COLOMBO 1. 827122858V 10000104 064 061 11 ABHAYARATHNE, Y.P.J. OFFICE OF THE SUPERINTENDENT OF POLICE, KELANIYA. 841800117V 10000118 049 057 12 WEERAKOON, W.A.D.B. 140/B, THANAYAM PLACE, INGIRIYA. 802893329V 10000121 049 068 13 DE SILVA, W.I. -

North Western Province Rural Roads – Project 5
Involuntary Resettlement Due Diligence Report August 2014 SRI: Integrated Road Investment Program North Western Province Rural Roads – Project 5 Prepared by Road Development Authority, Ministry of Highways, Ports and Shipping for the Asian Development Bank CURRENCY EQUIVALENTS (as of 14 May 2014) Currency unit – Sri Lanka rupee (SLRe/SLRs) SLRe 1.00 = $ 0.007669 $1.00 = SLR 130.400 ABBREVIATIONS ADB - Asian Development Bank AP - Affected Person API - Affected Property Inventory CBO - Community Based Organization CPs - Community Participants CV - Chief Valuer DRR - Due Diligence Report DS - Divisional Secretariat ESDD - Environmental and Social Development Division FGD - Focus Group Discussion GoSL - Government of Sri Lanka GN - Grama Niladari GND - Grama Niladari Division GPS - Global Positioning System GRC - Grievance Redress Committee GRM - Grievance Redress Mechanism INGO - International Non-Government Organizations iROAD - Integrated Road Investment Program IR - Involuntary Resettlement LAA - Land Acquisition Act MOHPS - Ministry of Highways, Ports and Shipping MOU - Memorandum of Understanding MFF - Multi-tranche Financing Facility NGO - Non-Government Organizations NIRP - National Involuntary Resettlement Policy NWP - North Western Province PCC - Project Coordinating Committee PIU - Project Implementing Unit PRA - Participatory Rural Appraisal PS - Pradeshiya Sabha RDA - Road Development Authority SPS - Safeguards Policy Statement This involuntary resettlement due diligence is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. -
Eb Exam. for Tech. Service Seg.(A)
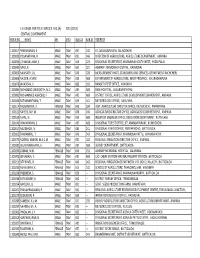
E.B. EXAM. FOR TECH. SERVICE SEG.(A) - 2011(2013) CENTRAL GOVERNMENT INDEX NO. NAME SEX MED SUB.03 SUB.04 ADDRESS 1100017 PRAPAHARAN, S. MALE TAM 057 040 67, ANANDAPURAM, KILINOCHCHI. 1100025 YOGANATHAN, R. MALE TAM 051 046 DIRECTOR OF AGRICULTURE, AGRICULTURE DEPARTMENT, AMPARA. 1100033 UTHAYAKUMAR, S. MALE TAM 044 023 DIVISIONAL SECRETARIAT, MANMUNAI SOUTH WEST, PADDIPALAI. 1100041 RAKU, K. MALE TAM 035 021 ASHRAFF, MEMORIAL HOSPITAL, KALMUNAI. 1100050 NAWSATH, A.L. MALE TAM 048 028 MEASUREMENT UNITS, STANDARDS AND SERVICES, DEPARTMENT KACHCHERI, 1100068 NALEER, A.M.M. MALE TAM 029 ABS DEPARTMENT OF AGRICULTURE, INTER PROVINCE, ANURADHAPURA. 1100076 JAYADEVA, V. MALE TAM 009 019 RANGE FOREST OFFICE, VAVUNIYA. 1100084 MOHAMED MASKOOTH, M.C. MALE TAM ABS ABS BASE HOSPITAL, AKKARAIPATHTHU. 1100092 MOHAMMED ASHIQUB, F. MALE TAM ABS ABS DISTRICT OFFICE, AGRICULTURE DEVELOPMENT DEPARTMENT, AMPARA. 1100106 SATHANANTHAM, T. MALE TAM 049 041 METEOROLOGY OFFICE, VAVUNIYA. 1100114 THUSYANTHY, K. FEMALE TAM 049 034 ASST. AGRICULTURE DIRECTOR OFFICE, KILINOCHCHI, PARANTHAN. 1100122 NAFEES, M.F.M. MALE TAM 058 046 AGRICULTURE DIRECTOR OFFICE, AGRICULTURE DEPARTMENT, AMPARA. 1100130 NIHAL, H. MALE TAM 059 ABS IRIGATION ENGINEER OFFICE, IRRIGATION DEPARTMENT, PUTTALAM. 1100149 PRAPAHARAN, S. MALE TAM ABS ABS DIVISIONAL FOREST OFFICE, 67, ANANDAPURAM, KILINOCHCHI. 1100157 NADESHON, N. MALE TAM 035 041 DIVISIONAL FOREST OFFICE, PERIYAR ROAD, BATTICALOA. 1100165 THARANIRAJ, T. MALE TAM 049 043 DIVISIONAL SECRETARIAT, MANMUNAI PATTU, ARAYAMPATHY. 1100173 NOORUL AMEEN, M.A.C.M. MALE TAM 050 042 REGIONAL IRRIGATION DIRECTOR OFFICE, AMPARA. 1100181 EBUNUSARKAANY, A. MALE TAM ABS ABS SURVEY DEPARTMENT, BATTICALOA. 1100190 ZAINAB, M.M. FEMALE TAM 046 052 ASHRAFF MEMORIAL HOSPITAL, KALMUNAI. -

Change in Other Field Crop Cultivation in the North Western Province
Change in Other Field Crop Cultivation in the North Western Province Wasanthi Wickramasinghe Research Report No: 160 October 2013 Hector Kobbekaduwa Agrarian Research and Training Institute 114, Wijerama Mawatha Colombo 7 Sri Lanka I First Published: October 2013 © 2013, Hector Kobbekaduwa Agrarian Research and Training Institute Coverpage Designed by: Udeni Karunaratne Final typesetting and lay-out by: Dilanthi Hewavitharana ISBN: 978-955-612-154-4 II FOREWORD Having reached a surplus paddy production in the country from mid 2000, government emphasis was placed on the development of Other Field Crop (OFC) sector to achieve self sufficiency targets of many other crops that can be produced in the country. Nevertheless, the performance of this sector in the recent past had not been promising. Therefore it is necessary to explore issues that are impedimented for the expansion of the OFC sector in Sri Lanka in order to provide some policy direction to the policy makers. A request was also made by the ministry of agriculture to investigate the factors responsible for the backward growth of this sector particularly in the North Western Province (NWP). Considering the necessity, HARTI undertook a study on the changes in other field crop sector in the NW province in 2011. Study identified the main farming system i.e. Chena that had been practiced in the dry zone for many years and supplied bulk of the OFC in the country. This traditional system had evolved into several farming systems in the recent past due to a number of factors. According to the study permanent homesteads cultivating mono-crops without fallowing (Goda hena), irrigated rice fields cultivating OFCs and supplementary irrigated uplands cultivating OFCs are the currently existing farming systems in the province. -

Democratic Socialist Republic of Sri Lanka COUNTRY STRATEGY and PROGRAMME EVALUATION
Independent Office of Evaluation Democratic Socialist Republic of Sri Lanka COUNTRY STRATEGY AND PROGRAMME EVALUATION Independent Office of Evaluation Independent Office of Evaluation International Fund for Agricultural Development Via Paolo di Dono, 44 - 00142 Rome, Italy Tel: +39 06 54591 - Fax: +39 06 5043463 E-mail: [email protected] www.ifad.org/evaluation www.twitter.com/IFADeval IFAD internal printing services www.youtube.com/IFADevaluation Democratic Socialist Republic of Sri Lanka Country Strategy and Programme Evaluation June 2019 Report No. 5080-LK Document of the International Fund for Agricultural Development Photos of activities supported by IFAD-financed projects in the Democratic Socialist Repubilc of Sri Lanka Front cover: A young farmer cultivating moringa, Anuradhapura District. ©IFAD/Smallholder Agribusiness Partnerships Programme Back cover: One of over 700 microirrigation schemes rehabilitated under the Dry Zone Livelihood Support and Partnership Programme, implemented between 2005 and 2013. At this site (Mulathella Ela, Haliela Divisional Secretariat, Badulla District), the canal was rehabilitated in 2011 to serve 30 acres of land; it is regularly maintained by beneficiary farmers. ©IFAD/Fumiko Nakai (left); A beneficiary of a floriculture project supported by the Smallholder Agribusiness Partnerships Programme, Rathnapura District. ©IFAD/Smallholder Agribusiness Partnerships Programme This report is a product of staff of the Independent Office of Evaluation of IFAD and the findings and conclusions expressed herein do not necessarily reflect the views of IFAD Member States or the representatives to its Executive Board. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of IFAD concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

North Western Province (NWP)
Environmental Impact Assessment December 2014 SRI: Water Resources Development Investment Program North Western Province (NWP) Prepared by Mahaweli Consultancy Bureau (Pvt) Ltd. for the Asian Development Bank. This environmental impact assessment is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section of this website. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. EIA STUDY OF THE PROPOSED NORTH WESTERN PROVINCE (NWP) CANAL PROJECT DRAFT FINAL REPORT MAHAWELI CONSULTANCY BUREAU (PRIVATE) LIMITED NO: 11, JAWATTA ROAD, COLOMBO 05 DECEMBER 2014 NWP Canal Project -EIA Study – Draft Final Report Abbreviation and Acronyms AMDP - Accelerated Mahaweli Development Project BW - Bed Width CEA - Central Environmental Authority CECB - Central Engineering and Consultancy Bureau CI - Cropping Intensity CKD - Chronic Kidney Disease Cumecs - Cubic Meters per second DS - Divisional Secretary DWLC - Department of Wildlife Conservation EC - Electrical Conductivity EIA - Environmental Impact Assessment EP - Eastern Province FD - Forest Department FSL - Full Supply Level FR - Forest Reserve GN - Grama Niladhari GSMB - Geological Survey -

Kurunegala District Map [
KURUNEGALA DISTRICT Administrative map Name & P-code of DS Divisions Map Locator Alawwa 6184 Ambanpola 6112 Bamunukotuwa 6149 Bingiriya 6142 Ehetuwewa 6109 Galgamuwa 6106 Ganewatta 6133 Giribawa 6103 ANURADHAPURA Ibbagamuwa 6130 Katupotha 6148 Kobeigane 6139 Kotawehera 6115 Kuliyapitiya East 6169 Ipologama ! Kuliyapitiya West 6172 Pahala! Giribawa Kurunegala 6154 GIRIBAWA Mahawa 6124 ! ! Tambutta Senarathgama Mallawapitiya 6157 ! ! Maradankadawala Mahagalkadawala Maspotha 6151 ! !Gamayagama Mawathagama 6160 ! Migalewa ! Narammala 6181 Attikulama Nikaweratiya 6121 Molewa! ! Palugama Weliyawa Panduwasnuwara 6145 ! ! Pannala 6178 Galgamuwa ! Polgahawela 6187 Nallachchiya! ! ! Legend Polpithigama 6127 Galgomuwa Mudiyannegama Rasnayakapura 6118 GALGAMUWA ! ! Rideegama 6163 Maha Torawa Udubaddawa 6175 ! DS Division Boundary Wariyapola 6136 Mamunugama ! EHETUWEWA Talawa! Weerambugedara 6166 Bulnewa! Main Road ! ! Ambanpola ! Kelegama Kendewa ! Moragollagama AMBANPOLA Tuttiripitiya ! Railway Line ! Mediyawa ! Katupitigama ! Nikawewa ! ! PUTTALAM KOTAWEHERA Ganekanda District HQ Uduweriya ! ! Kaluachchigama ! Madapokuna ! ! ! Daladagama Town ! POLPITHIGAMA ! ! Timbiriyawa Maho Polpitigama Viharehinne Ambale ! ! ! MAHAWA Likolapitiya Karambe Balalla ! ! ! NIKAWERATIYA Pugallegama MATALE ! ! !Ihalagama Kaduwala RASNAYAKAPURADiwullewa Egodayagama ! ! ! Nikaweratiya Polgahagangoda Landawatta Potuwewa ! ! ! Rambe ! Moragahawewa Hiriyala Kadigawa ! ! Madahapola ! Kaudottawa Digitowa ! ! ! KOBEIGANE Kumbukgete ! ! Diddeniya WARIYAPOLA ! Kobeigane Migahawela -

Adb Funded Integrated Road Investment Program
Social Monitoring Report Project Number: 47273 Loan Numbers: Tranche 1 – 3171 Tranche 2 – 3221 /3222 Tranche 3 – 3325 /3326 Semiannual Report January to June 2017 SRI: Integrated Road Investment Program PIC 02 – North Western and North Central Provinces Prepared by the Road Development Authority, Ministry of Higher Education and Highways for the Asian Development Bank. This social monitoring report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. Your attention is directed to the “terms of use” section on ADB’s website.'. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area ADB FUNDED INTEGRATED ROAD INVESTMENT PROGRAM SEMI ANNUAL SOCIAL COMPLIANCE MONITORING REPORT NORTH CENTRAL & NORTH WESTERN PROVINCES January-June 2017 REPORT PREPARED BY PYUNGHWA ENGINEERING CONSULTANTS In Association with RESOURCES DEVELOPMENT CONSULTANTS On behalf of Road Development Authority Ministry of Higher Education and Highways Submitted to Asian Development Bank In Association with Table of Contents Ref. Topic Page 1.0 Introduction 03 1.1 Background of the Project 03 1.2 Staffing Setup at PIU, PIC and Contractor related to Social Safeguard 03 2.0 The Conventional Road Contracts 04 3.0 Progress -

Section Vi: Schedule of Requirements
Section VI – Schedule of Requirements 6-1 SECTION VI: SCHEDULE OF REQUIREMENTS DRAFT ADB Standard Bidding Document Procurement of Radio Telecommunication Products and Services 6-2 Section VI – Schedule of Requirements Table of contents 1 Overview _____________________________________________ 3 1.1 Background ........................................................................................................................... 3 1.2 Structure of the Schedule of Requirements (SOR) ............................................................ 3 1.3 Project Objectives ................................................................................................................. 3 1.4 Scope of Work ....................................................................................................................... 6 2 Current Environment ___________________________________ 9 3 Desired State ________________________________________ 10 3.1 Services to be supported by the LTE Network ................................................................. 10 3.2 Functional Architecture ...................................................................................................... 10 3.3 Expected Implementation Timetable ................................................................................. 16 4 Guiding Principles ____________________________________ 17 4.1 Standards ............................................................................................................................ 17 4.2 Scalability ...........................................................................................................................