Bone Marrow Failure Gene Sequencing Panel
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification of the DNA Repair Defects in a Case of Dubowitz Syndrome
Identification of the DNA Repair Defects in a Case of Dubowitz Syndrome Jingyin Yue, Huimei Lu, Shijie Lan, Jingmei Liu, Mark N. Stein, Bruce G. Haffty, Zhiyuan Shen* The Cancer Institute of New Jersey, Robert Wood Johnson Medical School, New Brunswick, New Jersey, United States of America Abstract Dubowitz Syndrome is an autosomal recessive disorder with a unique set of clinical features including microcephaly and susceptibility to tumor formation. Although more than 140 cases of Dubowitz syndrome have been reported since 1965, the genetic defects of this disease has not been identified. In this study, we systematically analyzed the DNA damage response and repair capability of fibroblasts established from a Dubowitz Syndrome patient. Dubowitz syndrome fibroblasts are hypersensitive to ionizing radiation, bleomycin, and doxorubicin. However, they have relatively normal sensitivities to mitomycin-C, cisplatin, and camptothecin. Dubowitz syndrome fibroblasts also have normal DNA damage signaling and cell cycle checkpoint activations after DNA damage. These data implicate a defect in repair of DNA double strand break (DSB) likely due to defective non-homologous end joining (NHEJ). We further sequenced several genes involved in NHEJ, and identified a pair of novel compound mutations in the DNA Ligase IV gene. Furthermore, expression of wild type DNA ligase IV completely complement the DNA repair defects in Dubowitz syndrome fibroblasts, suggesting that the DNA ligase IV mutation is solely responsible for the DNA repair defects. These data suggests that at least subset of Dubowitz syndrome can be attributed to DNA ligase IV mutations. Citation: Yue J, Lu H, Lan S, Liu J, Stein MN, et al. -

WHIM Syndrome: from Pathogenesis Towards Personalized Medicine and Cure
Journal of Clinical Immunology (2019) 39:532–556 https://doi.org/10.1007/s10875-019-00665-w CME REVIEW WHIM Syndrome: from Pathogenesis Towards Personalized Medicine and Cure Lauren E. Heusinkveld1,2 & Shamik Majumdar1 & Ji-Liang Gao1 & David H. McDermott1 & Philip M. Murphy1 Received: 22 April 2019 /Accepted: 26 June 2019 /Published online: 16 July 2019 # This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply 2019 Abstract WHIM syndrome is a rare combined primary immunodeficiency disease named by acronym for the diagnostic tetrad of warts, hypogammaglobulinemia, infections, and myelokathexis. Myelokathexis is a unique form of non-cyclic severe congenital neutropenia caused by accumulation of mature and degenerating neutrophils in the bone marrow; monocytopenia and lympho- penia, especially B lymphopenia, also commonly occur. WHIM syndrome is usually caused by autosomal dominant mutations in the G protein-coupled chemokine receptor CXCR4 that impair desensitization, resulting in enhanced and prolonged G protein- and β-arrestin-dependent responses. Accordingly, CXCR4 antagonists have shown promise as mechanism-based treatments in phase 1 clinical trials. This review is based on analysis of all 105 published cases of WHIM syndrome and covers current concepts, recent advances, unresolved enigmas and controversies, and promising future research directions. Keywords Chemokine . CXCL12 . CXCR4 . CXCR2 . myelokathexis . human papillomavirus . plerixafor Historical Background [M:E] ratio with a “shift to the right”); and (3) numerous dysmorphic bone marrow neutrophils having cytoplasmic Myelokathexis was first described as a new type of severe hypervacuolation and hyperlobulated pyknotic nuclear lobes congenital neutropenia in 1964 by Krill and colleagues from connected by long thin strands (Fig. -

Dyskeratosis Congenita Precision Panel Overview Indications Clinical
Dyskeratosis Congenita Precision Panel Overview Dyskeratosis Congenita (DKC) is a rare, progressive bone marrow failure syndrome characterized by reticulated skin hyperpigmentation, nail dystrophy and oral leukoplakia. Patients usually present with symptoms of skin hyperpigmentation and nail changes during the first decade of life. It is caused by germline mutations in genes regulating telomere maintenance, resulting in very short telomeres. DKC is a genetically heterogeneous with X-linked recessive form being the most common, autosomal dominant and autosomal recessive subtypes based on different patters of inheritance. Early mortality is associated with bone marrow failure, infections, lung and pulmonary complications as well as malignancy. The Igenomix Dyskeratosis Congenita Precision Panel can be used for an accurate and directed diagnosis as well as differential diagnosis of reticulate pigmentary disorders ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Dyskeratosis Congenita Precision Panel is used for patients with a clinical diagnosis or suspicion with or without the following symptoms: ‐ Abnormal skin pigmentation (tan-to-gray hyperpigmented or hypopigmented macules and patches) ‐ Nail dystrophy ‐ Skin atrophy and telangiectasia ‐ Alopecia of the skin, eyebrows and eyelashes ‐ Mucosal leukoplakia ‐ Bone marrow failure ‐ Dental manifestations Clinical Utility The clinical utility of this panel is: ‐ The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. 1 ‐ Early initiation of treatment involving a multidisciplinary team in the form of hematopoietic stem cell transplantation as well as medical care to prevent complications and early surveillance of malignancy. -

The Hematological Complications of Alcoholism
The Hematological Complications of Alcoholism HAROLD S. BALLARD, M.D. Alcohol has numerous adverse effects on the various types of blood cells and their functions. For example, heavy alcohol consumption can cause generalized suppression of blood cell production and the production of structurally abnormal blood cell precursors that cannot mature into functional cells. Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia. Alcohol also interferes with the production and function of white blood cells, especially those that defend the body against invading bacteria. Consequently, alcoholics frequently suffer from bacterial infections. Finally, alcohol adversely affects the platelets and other components of the blood-clotting system. Heavy alcohol consumption thus may increase the drinker’s risk of suffering a stroke. KEY WORDS: adverse drug effect; AODE (alcohol and other drug effects); blood function; cell growth and differentiation; erythrocytes; leukocytes; platelets; plasma proteins; bone marrow; anemia; blood coagulation; thrombocytopenia; fibrinolysis; macrophage; monocyte; stroke; bacterial disease; literature review eople who abuse alcohol1 are at both direct and indirect. The direct in the number and function of WBC’s risk for numerous alcohol-related consequences of excessive alcohol increases the drinker’s risk of serious Pmedical complications, includ- consumption include toxic effects on infection, and impaired platelet produc- ing those affecting the blood (i.e., the the bone marrow; the blood cell pre- tion and function interfere with blood cursors; and the mature red blood blood cells as well as proteins present clotting, leading to symptoms ranging in the blood plasma) and the bone cells (RBC’s), white blood cells from a simple nosebleed to bleeding in marrow, where the blood cells are (WBC’s), and platelets. -

DNA Ligase IV Syndrome; a Review Thomas Altmann1 and Andrew R
Altmann and Gennery Orphanet Journal of Rare Diseases (2016) 11:137 DOI 10.1186/s13023-016-0520-1 REVIEW Open Access DNA ligase IV syndrome; a review Thomas Altmann1 and Andrew R. Gennery1,2* Abstract DNA ligase IV deficiency is a rare primary immunodeficiency, LIG4 syndrome, often associated with other systemic features. DNA ligase IV is part of the non-homologous end joining mechanism, required to repair DNA double stranded breaks. Ubiquitously expressed, it is required to prevent mutagenesis and apoptosis, which can result from DNA double strand breakage caused by intracellular events such as DNA replication and meiosis or extracellular events including damage by reactive oxygen species and ionising radiation. Within developing lymphocytes, DNA ligase IV is required to repair programmed DNA double stranded breaks induced during lymphocyte receptor development. Patients with hypomorphic mutations in LIG4 present with a range of phenotypes, from normal to severe combined immunodeficiency. All, however, manifest sensitivity to ionising radiation. Commonly associated features include primordial growth failure with severe microcephaly and a spectrum of learning difficulties, marrow hypoplasia and a predisposition to lymphoid malignancy. Diagnostic investigations include immunophenotyping, and testing for radiosensitivity. Some patients present with microcephaly as a predominant feature, but seemingly normal immunity. Treatment is mainly supportive, although haematopoietic stem cell transplantation has been used in a few cases. Keywords: DNA Ligase 4, Severe combined immunodeficiency, Primordial dwarfism, Radiosensitive, Lymphoid malignancy Background factors include intracellular events such as DNA replica- DNA ligase IV deficiency (OMIM 606593) or LIG4 syn- tion and meiosis, and extracellular events including drome (ORPHA99812), also known as Ligase 4 syn- damage by reactive oxygen species and ionising radi- drome, is a rare autosomal recessive disorder ation. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

The Genetics and Clinical Manifestations of Telomere Biology Disorders Sharon A
REVIEW The genetics and clinical manifestations of telomere biology disorders Sharon A. Savage, MD1, and Alison A. Bertuch, MD, PhD2 3 Abstract: Telomere biology disorders are a complex set of illnesses meric sequence is lost with each round of DNA replication. defined by the presence of very short telomeres. Individuals with classic Consequently, telomeres shorten with aging. In peripheral dyskeratosis congenita have the most severe phenotype, characterized blood leukocytes, the cells most extensively studied, the rate 4 by the triad of nail dystrophy, abnormal skin pigmentation, and oral of attrition is greatest during the first year of life. Thereafter, leukoplakia. More significantly, these individuals are at very high risk telomeres shorten more gradually. When the extent of telo- of bone marrow failure, cancer, and pulmonary fibrosis. A mutation in meric DNA loss exceeds a critical threshold, a robust anti- one of six different telomere biology genes can be identified in 50–60% proliferative signal is triggered, leading to cellular senes- of these individuals. DKC1, TERC, TERT, NOP10, and NHP2 encode cence or apoptosis. Thus, telomere attrition is thought to 1 components of telomerase or a telomerase-associated factor and TINF2, contribute to aging phenotypes. 5 a telomeric protein. Progressively shorter telomeres are inherited from With the 1985 discovery of telomerase, the enzyme that ex- generation to generation in autosomal dominant dyskeratosis congenita, tends telomeric nucleotide repeats, there has been rapid progress resulting in disease anticipation. Up to 10% of individuals with apparently both in our understanding of basic telomere biology and the con- acquired aplastic anemia or idiopathic pulmonary fibrosis also have short nection of telomere biology to human disease. -
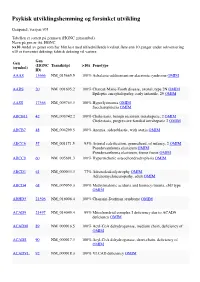
Psykisk Utviklingshemming Og Forsinket Utvikling
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

:.. ;}.·:···.·;·1 Congenital Neutropenia
C HAP T E R 13 >;:.. ;}.·:···.·;·1 CONGENITAL NEUTROPENIA Jill M. Watanabe, MD, MPH, and David C. Dale, MD defined by a neutrophil count less than 1500 cellS/ilL; KEY POINTS beyond 10 years of age, neutropenia is defined by a neu trophil count less' than 1800 cells//1L in persons of white Congenital Neutropenia and Asian descent. 1 In persons of African descent, neu tropenia is defined by a count of 800--1000 cells//1L. 1 (& Congenital neutropenia encompasses a heterogeneous group of The severity and duration of neutropenia are also clin iuheri ted diseases. ically important. Mild neutropenia is usually defined by • The genetic mutations causing congenital neutropenia may neutrophil counts of 1000-1500 cells//1L, moderate neu have an isolated effect on the bone marrow but can also affect tropenia is 500-1000 cells//1L, and severe neutropenia one or more other organ systems. is less than 500 cells//1L. Acute neutropenia usually is present for only 5-10 days; neutropenia is chronic if its (& The genetic defects underlying the diseases that cause con duration is at least several weeks. Almost all congenital genital neutropenia have been rapidly identified over the past neutropenias are chronic neutropenia. decade. The characteristics and causes of congenital neu (& Granulocyte colony-stimulating factor has dramatically tropenia are shown in Tables 13-1 and 13-2, and an algo improved the prognosis for children with congenital rithm for their diagnosis is presented in Figure 13-1. neutropenia. SEVERE CONGENITAL NEUTROPENIA Patient'; with severe congenital neutropenia (SCN) typi cally present with recurrent bacterial infections and neutrophil count'> persistently less than 200 cells//1L. -

Genomic Analysis of Bone Marrow Failure and Myelodysplastic Syndromes Reveals Phenotypic and Diagnostic Complexity
ARTICLES Bone Marrow Failure Genomic analysis of bone marrow failure and myelodysplastic syndromes reveals phenotypic and diagnostic complexity Michael Y. Zhang, 1 Siobán B. Keel, 2 Tom Walsh, 3 Ming K. Lee, 3 Suleyman Gulsuner, 3 Amanda C. Watts, 3 Colin C. Pritchard, 4 Stephen J. Salipante, 4 Michael R. Jeng, 5 Inga Hofmann, 6 David A. Williams, 6,7 Mark D. Fleming, 8 Janis L. Abkowitz, 2 Mary-Claire King, 3 and Akiko Shimamura 1,9,10 M.Y.Z. and S.B.K. contributed equally to this work. 1Clinical Research Division, Fred Hutchinson Cancer Research Center, Seattle, WA; 2Department of Medicine, Division of Hematology, University of Washington, Seattle, WA; 3Department of Medicine and Department of Genome Sciences, University of Washington, Seattle, WA; 4Department of Laboratory Medicine, University of Washington, Seattle, WA; 5Department of Pediatrics, Stanford University School of Medicine, Stanford, CA; 6Division of Hematology/Oncology, Boston Children’s Hospital, Dana Farber Cancer Institute, and Harvard Medical School, Boston, MA; 7Harvard Stem Cell Institute, Boston, MA; 8Department of Pathology, Boston Children’s Hospital, MA; 9Department of Pediatric Hematology/Oncology, Seattle Children’s Hospital, WA; 10 Department of Pediatrics, University of Washington, Seattle, WA, USA ABSTRACT Accurate and timely diagnosis of inherited bone marrow failure and inherited myelodysplastic syndromes is essen - tial to guide clinical management. Distinguishing inherited from acquired bone marrow failure/myelodysplastic syndrome poses a significant clinical challenge. At present, diagnostic genetic testing for inherited bone marrow failure/myelodysplastic syndrome is performed gene-by-gene, guided by clinical and laboratory evaluation. We hypothesized that standard clinically-directed genetic testing misses patients with cryptic or atypical presentations of inherited bone marrow failure/myelodysplastic syndrome. -

Iron Deficiency and the Anemia of Chronic Disease
Thomas G. DeLoughery, MD MACP FAWM Professor of Medicine, Pathology, and Pediatrics Oregon Health Sciences University Portland, Oregon [email protected] IRON DEFICIENCY AND THE ANEMIA OF CHRONIC DISEASE SIGNIFICANCE Lack of iron and the anemia of chronic disease are the most common causes of anemia in the world. The majority of pre-menopausal women will have some element of iron deficiency. The first clue to many GI cancers and other diseases is iron loss. Finally, iron deficiency is one of the most treatable medical disorders of the elderly. IRON METABOLISM It is crucial to understand normal iron metabolism to understand iron deficiency and the anemia of chronic disease. Iron in food is largely in ferric form (Fe+++ ) which is reduced by stomach acid to the ferrous form (Fe++). In the jejunum two receptors on the mucosal cells absorb iron. The one for heme-iron (heme iron receptor) is very avid for heme-bound iron (absorbs 30-40%). The other receptor - divalent metal transporter (DMT1) - takes up inorganic iron but is less efficient (1-10%). Iron is exported from the enterocyte via ferroportin and is then delivered to the transferrin receptor (TfR) and then to plasma transferrin. Transferrin is the main transport molecule for iron. Transferrin can deliver iron to the marrow for the use in RBC production or to the liver for storage in ferritin. Transferrin binds to the TfR on the cell and iron is delivered either for use in hemoglobin synthesis or storage. Iron that is contained in hemoglobin in senescent red cells is recycled by binding to ferritin in the macrophage and is transferred to transferrin for recycling.