Special Committee on Covid-19 Response
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dáil Éireann
DÁIL ÉIREANN AN ROGHCHOISTE UM CHOMHSHAOL AGUS GHNÍOMHÚ AR SON NA HAERÁIDE SELECT COMMITTEE ON ENVIRONMENT AND CLIMATE ACTION Dé Céadaoin, 9 Meitheamh 2021 Wednesday, 9 June 2021 Tháinig an Romhchoiste le chéile ag 9.30 a.m. The Select Committee met at 9.30 a.m. Comhaltaí a bhí i láthair / Members present: Teachtaí Dála / Deputies Richard Bruton, Réada Cronin, Cormac Devlin, Alan Farrell, Darren O’Rourke, Christopher O’Sullivan, Neale Richmond,+ Ossian Smyth (Minister of State at the De- partment of the Environment, Climate and Communications), Jennifer Whitmore. + In éagmais le haghaidh cuid den choiste / In the absence for part of the meeting of Deputy Alan Farrell. I láthair / In attendance: Deputies Matt Carthy, Micheal Fitzmaurice, Micheal Healy-Rae, Michael Lowry, Denis Naughten, Richard O’Donoghue, Sean Sherlock and Duncan Smith Teachta / Deputy Brian Leddin sa Chathaoir / in the Chair. 1 SECA Business of Select Committee. Chairman: We are in public session. Members are reminded of the long-standing par- liamentary practice to the effect that they should not comment on, criticise or make charges against a person outside the Houses or an official by name or in such a way as to make him or her identifiable. I also remind members that they are only allowed to participate in this meeting if they are physically located on the Leinster House campus. In this regard, I ask that members, prior to making their contributions to the meeting, confirm they are on the grounds of the Lein- ster House campus. I note that the Minister of State at the Department of the Environment, Climate and Commu- nications, Deputy Ossian Smyth, is standing in for the Minister for the Environment, Climate and Communications, Deputy Eamon Ryan, today and that the Minister of State joins us from Government Buildings. -

Representations Received by the Chairman's Office from Public
Representations received by the Chairman’s Office from Public Representatives in 2020 On behalf of a Name General Issue Grand Total person Aidan Davitt 2 4 6 Aindrias Moynihan 0 20 20 Alan Hayes 1 0 1 Alan Kelly 0 2 2 Anne Rabbitte 1 1 2 Barry Cowen 0 3 3 Bernard Durkan 0 2 2 Brendan Griffin 0 21 21 Brian Stanley 0 1 1 Cathal Crowe 1 7 8 Catherine Martin 0 1 1 Catherine Murphy 6 4 10 Charlie Flanagan 0 5 5 Charlie McConalogue 1 4 5 Christopher O’Sullivan 10 12 22 Cian O’Callaghan 1 0 1 Ciaran Cannon 0 6 6 Claire Kerrane 0 1 1 Colm Brophy 1 2 3 Colm Burke 0 1 1 Cormac Devlin 0 14 14 Dara Calleary 0 1 1 Dara Mulvey 0 1 1 Darragh O’Brien 1 15 16 David Norris 0 1 1 Denis Naughten 0 16 16 Denise Mitchell 0 1 1 Dessie Ellis 1 1 2 Eamon O Cuiv 0 3 3 Emer Higgins 1 0 1 Eoghan Murphy 0 1 1 Fergus O’Dowd 0 3 3 Finian McGrath 0 1 1 Francis Noel Duffy 0 1 1 Frank Feighan 0 12 12 Garrett Ahearn 1 1 2 Gerard Craughwell 0 1 1 Gino Kenny 0 1 1 Heather Humphreys 0 9 9 Helen McEntee 0 6 6 Hildegarde Naughten 1 3 4 Imelda Munster 0 2 2 Jack Chambers 0 2 2 1 On behalf of a Name General Issue Grand Total person Jackie Cahill 3 2 5 James Browne 0 6 6 James Lawless 1 11 12 James O’Connor 3 7 10 Jennifer Carroll MacNeill 2 0 2 Jennifer Murnane O’Connor 4 4 8 Jerry Buttimer 0 2 2 Jim Daly 1 1 2 Joe Carey 3 3 6 Joe Flaherty 0 8 8 Joe McHugh 1 4 5 Joe O’Brien 1 0 1 Joe O’Reilly 0 1 1 John Brady 0 1 1 John Brassill 0 1 1 John Cummins 1 0 1 John Lahart 2 3 5 John Lawless 0 2 2 John McGahon 1 3 4 John McGuinness 3 13 16 John Paul Phelan 1 4 5 Johnny Mythen 1 0 1 Josepha -
Minutes Template
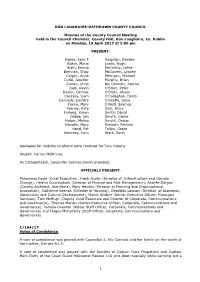
DÚN LAOGHAIRE-RATHDOWN COUNTY COUNCIL Minutes of the County Council Meeting held in the Council Chamber, County Hall, Dún Laoghaire, Co. Dublin on Monday, 10 April 2017 at 5.00 pm PRESENT: Bailey, John F Kingston, Deirdre Baker, Marie Lewis, Hugh Blain, Emma McCarthy, Lettie Brennan, Shay McGovern, Lynsey Colgan, Anne Merrigan, Michael Cuffe, Jennifer Murphy, Brian Curran, Chris Nic Cormaic, Sorcha Daly, Kevin O'Brien, Peter Devlin, Cormac O'Brien, Shane Dockery, Liam O'Callaghan, Denis Donnelly, Deirdre O'Keeffe, Dave Fayne, Mary O'Neill, Seamas Feeney, Kate Saul, Barry Furlong, Karen Smith, Dónal Gildea, Jim Smyth, Carrie Halpin, Melisa Smyth, Ossian Hanafin, Mary Stewart, Patricia Hand, Pat Tallon, Grace Kennedy, John Ward, Barry Apologies for inability to attend were received for Tom Murphy Absent: Carron McKinney An Cathaoirleach, Councillor Cormac Devlin presided. OFFICIALS PRESENT: Philomena Poole (Chief Executive), Frank Austin (Director of Infrastructure and Climate Change), Helena Cunningham (Director of Finance and Risk Management), Andrée Dargan (County Architect, Architects), Mary Henchy (Director of Planning and Organisational Innovation), Catherine Keenan (Director of Housing), Dearbhla Lawson (Director of Economic, Community and Cultural Development), Martin Allidine (Senior Executive Officer, Municipal Services), Tom McHugh (Deputy Chief Executive and Director of Corporate, Communications and Governance), Thomas Mahon (Senior Executive Officer, Corporate, Communications and Governance), Pamela Graydon (Senior Staff Officer, Corporate, Communications and Governance) and Fergus McCafferty (Staff Officer, Corporate, Communications and Governance) C/164/17 Votes of Condolence A vote of condolence was passed with Councillor S. Nic Cormaic and her family on the death of her mother, Deirdre R.I.P. A vote of condolence was passed with the families of Captain Dara Fitzpatrick and Captain Mark Duffy of the Coast Guard Helicopter Rescue 116 who died tragically while carrying out a 1 rescue mission on the west coast of Ireland on 14th March 2017. -
The Debate Can Be Accessed Here
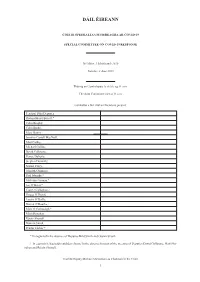
DÁIL ÉIREANN COISTE SPEISIALTA UM FHREAGRA AR COVID-19 SPECIAL COMMITTEE ON COVID-19 RESPONSE Dé Máirt, 2 Meitheamh 2020 Tuesday, 2 June 2020 Tháinig an Comhchoiste le chéile ag 11 a.m. The Joint Committee met at 11 a.m. Comhaltaí a bhí i láthair/Members present: Teachtaí Dála/Deputies Richard Boyd Barrett,* Colm Brophy, Colm Burke, Mary Butler, Jennifer Carroll MacNeill, Matt Carthy, Michael Collins, David Cullinane, Pearse Doherty, Stephen Donnelly, Norma Foley, John McGuinness, Paul Murphy,* Malcolm Noonan,* Joe O’Brien,* Cian O’Callaghan,+ Fergus O’Dowd, Louise O’Reilly, Darren O’Rourke,+ Marc Ó Cathasaigh,* Matt Shanahan, Róisín Shortall, Duncan Smith, Peadar Tóibín.+ * In éagmais/In the absence of Deputies Bríd Smith and Ossian Smyth. + In éagmais le haghaidh cuid den choiste/In the absence for part of the meeting of Deputies David Cullinane, Matt Sha- nahan and Róisín Shortall. Teachta/Deputy Michael McNamara sa Chathaoir/in the Chair. 1 SCR Business of Special Committee Chairman: Today Deputy Joe O’Brien will substitute for Deputy Ossian Smyth and Deputy Tóibín will substitute for Deputy Shanahan. Are the minutes of 19 and 26 May agreed? The minutes are agreed. A letter from Construction Industry Federation was sent under correspon- dence. I take it that the 36 items of correspondence are received and noted. Members will have received submissions for today’s meeting. Deputy David Cullinane: While we are dealing with correspondence, I sent a letter on behalf of the Sinn Féin group on a matter we also raised at our procedures meeting. We feel it is important that we have a follow-on session on private nursing homes with the HSE and the Department of Health. -

Contents Contents
Oireachtas Report Thursday 19th March, 2020 Contents Contents .......................................................................................................................................................... 1 Health (Preservation and Protection and other Emergency Measures in the Public Interest) Bill 2020: Second Stage ................................................................................................................................................... 2 Minister for Health (Deputy Simon Harris .................................................................................................. 2 Deputy Stephen Donnelly ........................................................................................................................... 6 Deputy Willie O'Dea .................................................................................................................................... 8 Deputy Robert Troy .................................................................................................................................... 9 Deputy Mary Lou McDonald .....................................................................................................................10 Deputy Louise O'Reilly ..............................................................................................................................12 Deputy Eamon Ryan ..................................................................................................................................14 Deputy Marc Ó Cathasaigh .......................................................................................................................15 -

List of TD's Wicklow, Greystones, Bray and DLR Areas
List of TD’s Wicklow, Greystones, Bray and DLR Areas Joe Behan Independent Councillor for Bray West [email protected] Melanie Corrigan Fine Gael Bray West [email protected] Mags Crean Independent Greystones [email protected] Anne Ferris Labour Councillor for Bray East [email protected] Aoife Flynn Kennedy Fine Gael Bray East [email protected] Tom Fortune Independent Councillor for Greystones [email protected] Steven Matthews Green Party Councillor for Bray East [email protected] Grace McManus Sinn Fein Bray East [email protected] Derek Mitchell Fine Gael Councillor for Greystones [email protected] Dermot O’Brien Bray West [email protected] Rory O’Connor Bray West [email protected] Lourda Scott Green Party for Greystones [email protected] Gerry Walsh Fianna Fail Counillor for Greystones [email protected] Jennifer Whitmore Social Democrats Coucillor for Greystones [email protected] Kazi Ahmed Glencullen – Sandyford [email protected] Emma Blain Fine Gael Councillor for Glencullen – Sandyford [email protected] Jennifer Carroll Macneill Killiney Shankill [email protected] Michael Clark Killiney Shankill [email protected] Cormac Devlin Fianna Fáil Councillor for Dún Laoghaire [email protected] Michael Fleming Glencullen – Sandyford [email protected] Jim Gildea Fine Gael Councillor for Killiney-Shankill [email protected] Lorraine Hall Dun Laoghaire [email protected] Melisa Halpin People Before -

Dáil Éireann
DÁIL ÉIREANN COISTE SPEISIALTA UM FHREAGRA AR COVID-19 SPECIAL COMMITTEE ON COVID-19 RESPONSE Dé Máirt, 16 Meitheamh 2020 Tuesday, 16 June 2020 Tháinig an Coiste le chéile ag 11 a.m. The Committee met at 11 a.m. Comhaltaí a bhí i láthair / Members present: Teachtaí Dála / Deputies Richard Boyd Barrett,* Colm Brophy, Colm Burke, Mary Butler, Jennifer Carroll MacNeill, Matt Carthy, Michael Collins, David Cullinane, Pearse Doherty, Stephen Donnelly, Mairéad Farrell,* Norma Foley, Gary Gannon,+ Neasa Hourigan,* John McGuinness, Paul Murphy,* Ged Nash,+ Fergus O’Dowd, Róisín Shortall, Duncan Smith, Peadar Tóibín.+ * In éagmais / In the absence of Deputies Louise O’Reilly, Bríd Smith and Ossian Smyth. + In éagmais le haghaidh cuid den choiste / In the absence for part of the meeting of Depu- ties Matt Shanahan, Róisín Shortall and Duncan Smith. Teachta / Deputy Michael McNamara sa Chathaoir / in the Chair. 1 SCR Business of Special Committee Chairman: We have been notified that Deputies Farrell, Hourigan, Ó Cathasaigh, Paul Murphy, Boyd Barrett and Tóibín will substitute for their party colleagues today. Are the min- utes of 9 and 11 June agreed? Agreed. I will take the 20 items of correspondence received as noted. Members will have received written submissions for today’s meeting. Deputy Róisín Shortall: Did we get anything from the Central Bank? Chairman: The Central Bank is not coming in today, it is coming later, on 7 July. Today is the Irish Fiscal Advisory Council and the ESRI. Deputy John McGuinness: Is it possible that the questions which went unanswered on which we were to be sent written reply would be flagged, given the quantity of correspondence being received, if the clerk does not mind? Chairman: Okay. -

Dáil Éireann
DÁIL ÉIREANN AN COMHCHOISTE UM IOMPAR AGUS CUMARSÁID JOINT COMMITTEE ON TRANSPORT AND COMMUNICATIONS Dé Céadaoin, 26 Bealtaine 2021 Wednesday, 26 May 2021 Tháinig an Comhchoiste le chéile ag 12.30 p.m. The Joint Committee met at 12.30 p.m. Comhaltaí a bhí i láthair / Members present: Teachtaí Dála / Deputies Seanadóirí / Senators Joe Carey, Lynn Boylan, Cathal Crowe, Jerry Buttimer, Michael Lowry, Gerard P. Craughwell, Steven Matthews, Timmy Dooley, James O’Connor, Gerry Horkan. Darren O’Rourke, Ruairí Ó Murchú, Duncan Smith. I láthair / In attendance: Deputy Michael McNamara. Teachta / Deputy Kieran O’Donnell sa Chathaoir / in the Chair. 1 JTC National Cybersecurity: Discussion (Resumed) Chairman: We are continuing our discussion of national cybersecurity. The specific pur- pose of this meeting is to discuss national cybersecurity in light of the recent cyberattacks on the HSE and the Department of Health. I welcome the Minister of State at the Department of the Environment, Climate and Communications, Deputy Ossian Smyth. All witnesses are again reminded of the long-standing parliamentary practice that they should not criticise or make charges against any person, persons or entity by name or in such a way as to make him, her or it identifiable, or otherwise engage in speech that might be regarded as damaging to the good name of the person or entity. If statements are potentially defama- tory in respect of an identifiable person or entity, witnesses will be directed to discontinue their remarks. It is imperative that they comply with all such directions. For witnesses attending remotely, outside of the Leinster House campus, there are some limitations to parliamentary privilege. -

Annual Report 2014 (Pdf
Dún Laoghaire-Rathdown County Council Annual Report 2014 Cover photo: ©Dennis Gilbert/VIEW www.viewpictures.co.uk Dún Laoghaire-Rathdown County Council Annual Report 2014 1 Contents Foreword 2014 2 Names, Addresses, Party Affiliations and Telephone Numbers of Members of Dún Laoghaire-Rathdown County Council 3 Councillors’ Committee Membership within Dún Laoghaire-Rathdown County Council 5 Councillor Membership of Other Bodies 7 Strategic Policy Committee (SPC) Membership 14 Strategic Policy Committee Reports 17 Councillors Meetings Attendance 1st January to 31st December 2014 18 List of Conferences/Training Attended During 2014 20 Audit of Councillors’ Motions Agreed at Council Meetings 2014 22 Local Elections (Disclosure of Donations and Expenditure) Act 1999 32 Payments to Councillors in 2014 34 Architecture and Culture Department 40 Corporate Services and Human Resources Department 44 Environment Department 48 Finance and I.T. Department 54 Housing and Community Department 58 Legal Services Department 65 Planning & Enterprise Department 66 Transportation and Water Services Department 72 Statement of Financial Position (Balance Sheet) as at 31st December 2014 80 Statement of Comprehensive Income (Income and Expenditure Account Statement) For Year Ended 31st December 2014 81 Performance Indicators 2014 82 Energy Management / Awareness 99 2 Dún Laoghaire-Rathdown County Council Annual Report 2014 Foreword 2014 We are pleased to introduce the Council’s Annual Report 2014, which outlines the work of the Council in delivering important public -

Ireland's Emergency Powers During the Covid-19 Pandemic
RESEARCH SERIES Ireland’s Emergency Powers During the Covid-19 Pandemic Conor Casey, Oran Doyle, David Kenny and Donna Lyons Ireland’s Emergency Powers During the Covid-19 Pandemic Report prepared for The Irish Human Rights and Equality Commission by The COVID-19 Law and Human Rights Observatory Conor Casey, Oran Doyle, David Kenny and Donna Lyons First published in February 2021 by the Irish Human Rights and Equality Commission 16–22 Green Street, Dublin 7, D07 CR20. Copyright © Irish Human Rights and Equality Commission February 2021 The Irish Human Rights and Equality Commission was established under statute on 1 November 2014 to protect and promote human rights and equality in Ireland, to promote a culture of respect for human rights, equality and intercultural understanding, to promote understanding and awareness of the importance of human rights and equality, and to work towards the elimination of human rights abuses and discrimination. ISBN 978-1-913492-03-8 Acknowledgements Foreword The authors of this Report are all members of the COVID-19 Law and Human I am delighted to present this report by the Trinity College Dublin COVID-19 Law Rights Observatory at Trinity College Dublin.1 The Observatory was established and Human Rights Observatory, which we commissioned in autumn 2020. We in June 2020, with the support of the Trinity College Dublin COVID Response did so in order to take stock of, and to better understand, the human rights and Fund, to engage in research across the full range of Ireland’s legal response to equality implications of the emergency measures undertaken since March 2020 to COVID-19, with the aim both to inform the public and to provoke public debate. -

The Debate Can Be Accessed Here
DÁIL ÉIREANN COISTE SPEISIALTA UM FHREAGRA AR COVID-19 SPECIAL COMMITTEE ON COVID-19 RESPONSE Dé Máirt, 28 Iúil 2020 Tuesday, 28 July 2020 Tháinig an Coiste le chéile ag 9 a.m. The Committee met at 9 a.m. Comhaltaí a bhí i láthair / Members present: Teachtaí Dála / Deputies Colm Burke, Jennifer Carroll MacNeill, Michael Collins, Cathal Crowe,* Cormac Devlin,* Bernard J. Durkan,* Neasa Hourigan,* Brian Leddin,* Paul McAuliffe,* Paul Murphy,+ Fergus O’Dowd, Louise O’Reilly, Darren O’Rourke,* Maurice Quinlivan,* Matt Shanahan, Róisín Shortall, Bríd Smith, Duncan Smith, Violet-Anne Wynne.+ * In éagmais / In the absence of Deputies Colm Brophy, Mary Butler, David Cullinane, Pearse Doherty, Stephen Donnelly and Ossian Smyth. + In éagmais le haghaidh cuid den choiste / In the absence for part of the meeting of Depu- ties Louise O’Reilly and Bríd Smith. Teachta / Deputy Michael McNamara sa Chathaoir / in the Chair. 1 SCR Business of Special Committee Chairman: We have a quorum and are in public session. We have been notified that the following Deputies will substitute for their party colleagues: Deputies Crowe, Devlin, Durkan, Hourigan, Leddin, McAuliffe, Murnane O’Connor, Murphy, O’Rourke, O’Sullivan, Quinlivan and Wynne. I take it that the ten items of correspondence received are noted. We will resume consideration of our draft report on nursing homes at 3.30 p.m. today, with a view to publication later this week. We also have a report on testing and tracing and an interim progress report to consider. It is unlikely that we will have sufficient time to deal with all of these but we will consider these matters in further detail at 3.30 p.m. -

Looking Back a T General Elections Both Past And
09 ELECTION / 2020 02 LESSON ACTIVITIES L O O K I N G B A C K A T G E N E R A L E L E C T I O N S - B O T H P A S T A N D P R E S E N T 20 Election 2020 – Results and Analysis at a Glance The 2020 General Election took place on Saturday the 9th of February. The election was called following the dissolution of the 32nd Dáil by the President, at the request of Taoiseach Leo Varadkar on 14 January 2020. Test your knowledge by filling in the blanks. The 33rd Dáil will have ____ TD’s (Teachta Dála) who will represent ____ constituencies. The number of allocated seats per constituency varies. Roscommon-Galway constituency has three seats, whereas Carlow-Kilkenny has _____ seats. Locate your constituency on the map. How many seats are allocated to your constituency? Why have some constituencies more TD seats than others? Image Source: By Erinthecute - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=86872192 Electorate and Constituencies: A constituency is an area that sends TDs to represent them in the Dáil. Constituencies are to be revised at least once in every twelve years in accordance with the census reports, which are compiled by the Central Statistics Office; under the Electoral Act 1997. The TDs (Teachta Dála) that represent each constituency are elected directly by the Irish people, otherwise known as the electorate. The electorate from each constituency elect their TDs to represent them in the Dáil during a general election.