8Th CRM Main Report.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Initial Environmental Examination IND
Initial Environmental Examination Document stage: Updated Project Number: 49107-006 February 2020 IND: West Bengal Drinking Water Sector Improvement Program – Bulk Water Supply for 2 - Blocks of Mejia and Gangajalghati, Bankura District Package No: DWW/BK/03 Prepared by Public Health Engineering Department, Government of West Bengal for the Asian Development Bank. ABBREVIATIONS ADB – Asian Development Bank CPCB – Central Pollution Control Board CTE – consent toestablish CTO – consent tooperate DSISC design, supervision and institutional support consultant EAC – Expert Appraisal Committee EHS – Environmental, Health and Safety EIA – Environmental Impact Assessment EMP – Environmental Management Plan GRC – grievance redress committee GRM – grievance redress mechanism GOI – Government of India GoWB – Government of West Bengal HSGO – Head, Safeguards and Gender Officer IBPS – Intermediate Booster Pumping Station IEE – Initial Environmental Examination IWD – Irrigation and Waterways Department MoEFCC – Ministry of Environment,Forestand Climate Change WBPCB – West Bengal Pollution Control Board NOC – No Objection Certificate PHED – Public Health Engineering Department PIU – Project Implementation Unit PMC – Project Management Consultant PMU – Project Management Unit PWSS - Pied Water Supply Scheme PPTA – Project Preparatory Technical Assistance REA – Rapid Environmental Assessment ROW – right of way SPS – Safeguard Policy Statement WHO – World Health Organization WTP – water treatment plant WBDWSIP – West Bengal Drinking Water Sector Improvement Project WEIGHTS AND MEASURES m3/hr cubic meter per hour dBA decibel C degree Celsius ha hectare km kilometre lpcd liters per capita per day m meter mbgl meters below ground level mgd million gallons per day MLD million liters per day mm millimeter km2 square kilometer NOTES In this report, "$" refers to US dollars. This initial environmental examination is a document of the borrower. -

District Disaster Management Plan Bankura ( 2019-2020 )
DISTRICT DISASTER MANAGEMENT PLAN BANKURA ( 2019-2020 ) Prepared by: DISTRICT DISASTER MANAGEMENT CELL, BANKURA WEST BENGAL INDEX CHAPTER No. CONTENT Page No. Chapter 1 Introduction 1 -13 Chapter 2 Hazard, Vulnerability, Capacity and Risk Assessment (HVCRA) 14 – 24 Chapter 3 Institutional Arrangement for Disaster Management (DM) 25 – 27 Chapter 4 Prevention and Mitigation Measures 28 – 34 Chapter 5 Preparedness Measures 35 - 50 Chapter 6 Capacity Building and Training Measures 51 – 57 Chapter 7 Response and Relief Measures 58 – 71 Chapter 8 Reconstruction, Rehabilitation and Recovery 72 – 76 Chapter 9 Financial Resources for Implementation of DDMP 77 Chapter 10 Procedure and Methodology for Monitoring, Evaluation, Updation and 78 – 79 Maintenance of DDMP Chapter 11 Co-ordination Mechanism for Implementation of DDMP 80 – 82 Chapter 12 Standard Operating Procedures (SOPs ) and Check List 83 – 99 Chapter 13 Important Telephone Numbers 100 - 105 AnnexURE Annexure 1 List of Civil Defence Equipment 106 - 108 List of Events or Melas where large crowds gather with event date and Annexure 2 location 109 - 110 Annexure 3 List of Petrol Pump 111 - 112 Annexure 4 List of LPG go-down 113 - 114 Annexure 5 List of Inflammable Industry 115 - 118 Annexure 6 Vulnerability Report 119 Annexure 7 Large Crowd 120 CHAPTER-1 INTRODUCTION Bankura though being a rain fed district, it is widely known as the drought prone district of the State. Drought is a regular feature in the North-West part of the district covering Chhatna, Saltora, Gangajalghati, Barjora, Bankura-I, Bankura-II, Mejia, Indpur, Hirbandh & Ranibandh Blocks. Though this district receives good amount of rainfall, around 1400 mm. -

District Disaster Management Plan 2016
DISTRICT DISASTER MANAGEMENT PLAN 2016 BANKURA OFFICE OF THE DISTRICT MAGISTRATE, BANKURA DISTRICT DISASTER MANAGEMENT CELL INDEX Sl. No. CONTENT Page No. 1 Introduction 1 2 Administrative Map of the District 2 – 5 3 District Profile 6 – 12 4 Preparedness – District Disaster Management Cell Emergency Contingency Plan 13 – 17 Stock position of relief materials 18 Identification of temporary cyclone / flood shelters 19 – 24 5 Preparedness –CIVIL DEFENCE 25 - 39 6 Preparedness – PUBLIC HEALTH ENGINEERING 40 – 42 7 Preparedness – HEALTH 43 – 62 8 Preparedness – IRRIGATION 63 – 67 9 Preparedness – AGRICULTURE 68 – 73 10 Preparedness – ANIMAL RESOURCES 74 – 78 DEVELOPMENT 11 Preparedness – HORTICULTURE 79 - 81 12 Important Telephone Numbers and e-mails 82 - 85 13 Preparedness Checklist for Various Departments 86 – 90 INTRODUCTION Bankura though being a rain fed district, it is widely known as the drought prone district of the State. Drought is a regular feature in the North-West part of the district covering Chhatna, Saltora, Gangajalghati, Barjora, Bankura-I, Bankura-II, Mejia, Indpur, Hirbandh & Ranibandh Blocks. Though this district receives good amount of rainfall, around 1400 mm. annually, is received per year yet cultivation and production of crop primarily depends on constricted period of erratic rainfall. About 80% to 90% rainfall is generally received by the district from June to September depending on the onset of monsoon. A conspicuous feature of this district is the absence of significant rainfall in the month of September and October. High runoff rate of rain water, inadequate storage facilities of the surface –runoff and low water holding capacity of the soil accelerate the drought situation. -

Appendix a List of Reference Maps
Appendix A List of Reference Maps List of Mouza (A Land – Settlement Division of an Area) Maps Police station Name of Mouza J.L. No. Police station Name of Mouza J.L. No. Nituria Saltora Barddhaman Jujuti 158 Chanchai 46 Mejhia Japamali 70 Chak Tentul 16 Jalanpur 74 Rhondia 4 Banjora 73 Gopalpur 121 Jangpur 72 Konerpur 161 Sarama 71 Dadpur 123 Dighalgram 69 Nala 20 Purbator 67 Belkas 21 Debagram 66 Baharpur 22 Damodarmohan 64 Idilpur 45 Balarampur 63 Fakirpur 25 Purunia 62 Kanchanagar 26 Murra 61 Bangpur 32 Telenda 60 Mirchhoba 33 Mejhia 37 Becharhat 79 Shrirampur 80 Barjora Pratappur 15 Hatsimul 81 Sitarampur 16 Kanthalgachi 83 Paharpur 51 Chaitpur 84 Krishnanagore 52 Amirpur 85 Bamandihi 53 Manikhati 108 Purakunda 54 Kalinagore 160 Tajpur 56 Pakhanna Bhairabpur 57 Pakhanna 58 Gopalpur 59 Galsi Gohagram 70 Radhakantapur 60 Dakshin 114 Bhasapur Sonda 116 Patrasair Uttar Patashpur 1 Sikarpur 117 Deulpara 2 Dumur 120 Khanpara 27 Jujuti 158 K. Bhattacharyya, The Lower Damodar River, India, Advances in Asian 253 Human-Environmental Research 3, DOI 10.1007/978-94-007-0467-1, C Springer Science+Business Media B.V. 2011 254 Appendix A Police station Name of Mouza J.L. No. Police station Name of Mouza J.L. No. Tashuli 28 Merual 159 Ghoradanga 29 Konarpur 161 Uttar Gobindapur 30 Panchpara 60 Mamudpur 61 Salkhara 64 Sonamukhi Palashdanga 1 Jamalpur Paikpara 66 Joynagar 2 Ujirpur 69 Alampur 4 Dhapdhara 64 Dihipara 5 Sonargeria 65 Rangamatia 8 Muidipur 67 Kenety 9 Haragobindapur 40 Nityanandapur 10 Beloa 108 Amritpara 136 Beshia 138 Bara 139 Memari -

Village & Town Directory, Bankura, Part XIII-A, Series-23, West Bengal
CENSUS OF INDIA 1981 SERIES 23 WEST BENGAL DISTRICT CENSUS HANDBOOK PART XIII-A VILLAGE & TOWN DIRECTORY BANKURA DISTRICT S.)I[~GHOSH of the Indian AdlTlinistratiYe Service DJiRI:CTQR '-IF CENSUS OPERATIONS WEST llEN~AL Price: (Inland) Rs. 15.00 Paise 11. lForeima) :£ 1.75 •• 5 , 40 Cellt.. PuBLISHED BY THB CONTROLLER. GoVERNMENT PRINTING.. WEST BENGAL ANa PRINTED BY MILl AR.T PRESS. 36. IMDAD ALl LANE, CALcuTTA-700016 1988 CONTENTS Page Poreword VII Preface IX Acbowledgemtnt XI Important Statistics XIII Aualytical Note 1-26 (i) Census Concepts: Rural and urban areas. Census House/Household. Scheduled Castes/Scheduled Tribes, Literates, Main Workers, Marginal Workers, Non-Workers (ii) Brief history of the District Census Handbook (iii) Scope of Village Directory and Town Directory (iv) Brief history of the District (v) Physical Aspects (vi) Major Characteristics (vii) Place of Religious. Historical or Archaeological importance in the villages and place of Tourist interest (viii) Brief analysis of the Village and Town Directory data. SECTION I-VILLAGE DIRECTORY 1. Saltora Police Station (a) Alphabetical list of villages 29 (b) Village Directory Statement 32 2. Mejhia Police Station (a) Alphabetical list of villages 50 (b) Village Directory Statement 52 3. Barjora Police Station (a) Alphabetical list of villages 61 (b) Village Directory Statement 64 .c. GangajaJghati Police Station (a) Alphabetical list of villages 86 (b) Village Directory Statement 90 5. Cbatna Police Station (a) Alphabetical list of villagCl 116 (b) Village Directory Statement 11. 6. Bankura Poliee Station (a) Alphabetical list of viUages 151 (b) Village Directory Statement 156 7. Onda Police Station (a) Alphabetical1ist of villages 190 (b) Village Directory Statement 194 I. -

Shilpakanan Ph-Iii- Flat 1 1317
SHILPAKANAN PH-III- FLAT SL FORM NAME ADDRESS REMARKS NO. 1 1317 ABHIJIT GHATAK 4/24, SAROJINI NAIDU PATH , CITY CENTRE , DURGAPUR -713216 2 1947 AJOY CHAUDHAURY C 18 PARK AVENUE P.O-BIDHANNAGAR DURGAPUR-713212 BURDWAN 3 1393 ALOKE KUMAR KUNDU B 24 SBI STAFF QTR DAVID HARE RD. TARULATA KUNDU DURGAPUR-713205 DIST-BURDWAN 4 1893 AMITAVA GHOSH SANCHITA 190, K.G.R.S PATH PURBACHALPALLY GHOSH P.O- ANGUS DIST-HOOGHLY PIN-71222 5 1370 AMIYA MISHRA JAYANTI VILL-JALANPUR, P.O-MALIARA P.S- MISHRA MEJHIA, DIST-BANKURA PIN-722142, 6 1380 AMRITA BHATTACHARYA 457, ANANDA ENCLAVE,ANANDAPUR KOLKATA-700107 7 1917 AMRITA DUTTA ARGOSY CO-OP HOUSING SOCIETY LTD FLAT-BB 45/7, BL-BB45, ROAD -146, PREMISE-05 NEW TOWN AA 1B KOLKATA-700156 8 1301 ANIL KUMAR MODI C/O-ANITA NISWAS , SARDA PALLY-1, P.O-UKHRA , DIST-BURDWAN (W.B) PIN- 713363 9 1314 ANIMESH UPADHYAY VILL-PANCHGACHIA , P.O-ETHORA , DIST- BURDWAN , PIN-713359 10 1969 ANINDYA SUNDAR MANDAL BELIAGHATA SAROBAR CO-OP HOUSING SOCIETY LTD. FLAT NO 3/A 25C RADHA MADHAB DUTTA KOL-700010 11 1365 ANUP KUMAR MUKHERJEE BN-8, D.P.L TOWNSHIP DURGAPUR PIN- SUPARNA MUKHERJEE 713202 12 1951 ANUP KUMAR ROY VILL-GOPALPUR UTTARPARA P.O- GOPALPUR DURGAPUR-12 DIST- BURDWAN 713212 13 1837 ANURUPA PAUL C/O-S.K MUKHERJEE ED-1, MALCOSE SARANI SECTOR-2C, BIDHANNAGAR , DURGAPUR-12 14 1775 APARNA SARKAR(SURAL) HEALTH CENTRE QUATER , P.O- DURLOVPUR DT- BANKURA PIN-722133 15 1806 APARUP BNERJEE P.O+AT-PANDAVESWAR N.S.B RD DIST- BURDWAN 16 1770 ARIJIT KHAN 127, RAJA RAMCHAND GHAT ROAD P.O- PANIHATI KOLKATA -700114 107 of 209 SHILPAKANAN -

District Disaster Management Plan Bankura ( 2020-2021 )
DISTRICT DISASTER MANAGEMENT PLAN BANKURA ( 2020-2021 ) Prepared by: DISTRICT DISASTER MANAGEMENT CELL, BANKURA WEST BENGAL INDEX CHAPTER No. CONTENT Page No. Chapter 1 Introduction 1 -13 Chapter 2 Hazard, Vulnerability, Capacity and Risk Assessment (HVCRA) 14 – 24 Chapter 3 Institutional Arrangement for Disaster Management (DM) 25 – 27 Chapter 4 Prevention and Mitigation Measures 28 – 34 Chapter 5 Preparedness Measures 35 - 50 Chapter 6 Capacity Building and Training Measures 51 – 57 Chapter 7 Response and Relief Measures 58 – 71 Chapter 8 Reconstruction, Rehabilitation and Recovery 72 – 76 Chapter 9 Financial Resources for Implementation of DDMP 77 Chapter 10 Procedure and Methodology for Monitoring, Evaluation, Updation and 78 – 79 Maintenance of DDMP Chapter 11 Co-ordination Mechanism for Implementation of DDMP 80 – 82 Chapter 12 Standard Operating Procedures (SOPs ) and Check List 83 – 99 Chapter 13 Important Telephone Numbers 100 - 104 AnnexURE List of Events or Melas where large crowds gather with event date and Annexure 1 location 105 - 107 Annexure 2 List of Petrol Pump 108 - 109 Annexure 3 List of LPG go-down 110 - 111 Annexure 4 List of Inflammable Industry 112 - 115 Annexure 5 Vulnerability Report 116 Annexure 6 Large Crowd 117-119 Annexure 7 Heritage Building 120 Annexure 8 MAJOR DISASTER & FINANCIAL LOSS DURING LAST FINANCIAL YEAR 121 Annexure 9 LIST OF EQUPMENTS WHICH MAY BE PROCURED IN THE NEXT YEAR 122 CHAPTER-1 INTRODUCTION Bankura though being a rain fed district, it is widely known as the drought prone district of the State. Drought is a regular feature in the North-West part of the district covering Chhatna, Saltora, Gangajalghati, Barjora, Bankura-I, Bankura-II, Mejia, Indpur, Hirbandh & Ranibandh Blocks. -
![West Bengal Drinking Water Sector Improvement Program: Water Supply Distribution System for Mejia & Gangajalghati Block (Bankura District) [Package WW/BK/04]](https://docslib.b-cdn.net/cover/5516/west-bengal-drinking-water-sector-improvement-program-water-supply-distribution-system-for-mejia-gangajalghati-block-bankura-district-package-ww-bk-04-8675516.webp)
West Bengal Drinking Water Sector Improvement Program: Water Supply Distribution System for Mejia & Gangajalghati Block (Bankura District) [Package WW/BK/04]
Initial Environmental Examination Document Stage: Draft Project Number: 49107-006 October 2018 IND: West Bengal Drinking Water Sector Improvement Program: Water Supply Distribution System for Mejia & Gangajalghati block (Bankura District) [Package WW/BK/04] Prepared by Public Health Engineering Department, Government of West Bengal for the Asian Development Bank. ABBREVIATIONS ADB – Asian Development Bank CPCB – Central Pollution Control Board CTE – consent to establish CTO – consent to operate DSISC design, supervision and institutional support consultant EAC – Expert Appraisal Committee EHS – Environmental, Health and Safety EIA – Environmental Impact Assessment EMP – Environmental Management Plan GRC – grievance redress committee GRM – grievance redress mechanism GOI – Government of India GoWB – Government of West Bengal HSGO – Head, Safeguards and Gender Officer IBPS – Intermediate Booster Pumping Station IEE – Initial Environmental Examination IWD – Irrigation and Waterways Department MoEFCC – Ministry of Environment, Forest and Climate Change WBPCB – West Bengal Pollution Control Board NOC – No Objection Certificate PHED – Public Health Engineering Department PIU – Project Implementation Unit PMC – Project Management Consultant PMU – Project Management Unit PWSS - Pied Water Supply Scheme PPTA – Project Preparatory Technical Assistance REA – Rapid Environmental Assessment ROW – right of way SPS – Safeguard Policy Statement WHO – World Health Organization WTP – water treatment plant WBDWSIP – West Bengal Drinking Water Sector Improvement Project WEIGHTS AND MEASURES m3/hr cubic meter per hour dBA decibel °C degree Celsius ha hectare km kilometre lpcd liters per capita per day m meter mbgl meters below ground level mgd million gallons per day MLD million liters per day mm millimeter km2 square kilometer NOTES In this report, "$" refers to United States dollars. CURRENCY EQUIVALENTS (as of 17 August, 2018) Currency unit = Rupee (INR) INR 1.00 = 0.014 USD USD 1.00 = 69.80 INR This initial environmental examination is a document of the borrower. -

District BLO-Supervisors Information Icw SSR-20 Ason 121219.Xlsx
BLO Information District AC No AC Name PS No Name of PS Name of BLO Contact No BANKURA 247 Saltora (SC) 1 Chhatar Kanali Prathamik Vidyalaya SUPRIYA MONDAL 8001964984 BANKURA 247 Saltora (SC) 2 Banspitali Prathamik Vidyalaya SUNARAM HANSDA 8145314905 BANKURA 247 Saltora (SC) 3 Saburbandh Junior Uchcha Vidyalaya (Room-1) RAMJIBAN MONDAL 9564625918 BANKURA 247 Saltora (SC) 4 Saburbandh Junior Uchcha Vidyalaya (Room-2) KARABI SIKDAR 8145642372 BANKURA 247 Saltora (SC) 5 Bamuntore Uchcha Vidyalaya (Room-1) PRADIP LAYEK 9647604039 BANKURA 247 Saltora (SC) 6 Bamuntore Uchcha Vidyalaya (Room-2) SUMITA LAYEK 7407845220 BANKURA 247 Saltora (SC) 7 Salbedia Prathamik Vidyalaya MITHU MUKHERJEE 9647597152 BANKURA 247 Saltora (SC) 8 Bihari Prathamik Vidyalaya MANOTOSH MONDAL 9647604087 BANKURA 247 Saltora (SC) 9 Shirpura Ramshankar Madhyamik Shiksha Kendra (Room-1) KRISHNA ACHARJEE 9635484324 BANKURA 247 Saltora (SC) 10 Shirpura Ramshankar Madhyamik Shiksha Kendra (Room-2) MUNMUN DAS 9932509045 BANKURA 247 Saltora (SC) 11 Tentularakh Prathamik Vidyalaya SANALI MONDAL 9679717129 BANKURA 247 Saltora (SC) 12 Rautora Prathamik Vidyalaya ASHA MAJI 8145464098 BANKURA 247 Saltora (SC) 13 Ketchka Prathamik Vidyalaya SUSHIL KUMAR GANGOPADHYAY 8338568397 BANKURA 247 Saltora (SC) 14 Iswarda Prathamik Vidyalaya ACHINTA SENGUPTA 9635965903 BANKURA 247 Saltora (SC) 15 Aanandapur Prathamik Vidyalaya MUKTA BANERJEE 9641880540 BANKURA 247 Saltora (SC) 16 Ilambazar Primary School MILAN KR. GHANTI 9732028702 BANKURA 247 Saltora (SC) 17 Kukhrakuri Prathamik Vidyalaya -
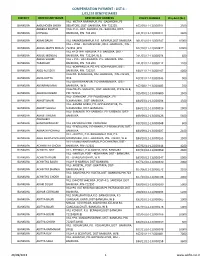
Compensation Payment : List-1 : 1,03,133 Beneficiaries
COMPENSATION PAYMENT : LIST-1 : 1,03,133 BENEFICIARIES DISTRICT BENEFICIARY NAME BENEFICIARY ADDRESS POLICY NUMBER Chq.Amt (Rs.) VILL- METIYA NARANPUR, PO- GADARDIHI, PS- BANKURA AABUHOSEN SHEKH BELIATORE, DIST- BANKURA, PIN- 722203. 107/09/11-12/000391 2500 ABABILA KHATUN VILL+ P.O.- HAT- ASHURIA, PS.- BARJORA, DIST- BANKURA MONDAL BANKURA, PIN- 722 204 241/01/12-13/000011 2400 BANKURA ABANI BAURI VILL-RAMKRISHNAPUR,P.O- RANIPUR,DIST-BANKURA 081/01/10-11/000247 10000 VILL + POST - NUTAN GRAM , DIST - BANKURA , PIN - BANKURA ABDUL MATIN MOLLA 722152 ,W.B 107/10/11-12/000877 10000 VILL.+P.O- HAT ASHURIA, P.S- BARJORA, DIST.- BANKURA ABDUL MONDAL BANKURA, PIN- 722204, W.B. 241/03/12-13/000074 600 ABDUL SALAM VILL + P.O.- HAT ASHURIA, P.S.- BARJORA, DIST- BANKURA TARAFDAR BANKURA, PIN- 722 204 241/01/12-13/000112 1200 VILL.-BONPARULIA, PO.+PS.-SONAMUKHI, DIST.- BANKURA ABED ALI SEKH BANKURA, PIN.-722207. 184/11/12-13/000167 4000 VILL+PO- KENJAKURA, DIST-BANKURA, PIN-722139, BANKURA ABHA DUTTA W.B 107/01/12-13/000545 900 VILL-JOYKRISHNAPUR, P.O-BARABENDYA, DIST- BANKURA ABHARANI MAN BANKURA, W.B 107/08/12-13/000485 700 VILL+PO+PS- SIMLAPAL, DIST- BANKURA, STATE-W.B, BANKURA ABHAYA DHIBAR PIN-722151 025/09/12-13/000680 1500 VILL- JOYNAGAR , PO- PALASDANGA , PS- BANKURA ABHIJIT BAURI SONAMUKHI , DIST- BANKURA . 184/03/11-12/000034 1300 VILL.-KAMAR GORIA, PO.-GOPIKANTAPUR, PS.- BANKURA ABHIJIT GHOSH SONAMUKHI, DIST.-BANKURA. 184/12/12-13/000016 2000 VILL- SARENGA. PO- SARENGA. PS- SARENGA. DIST- BANKURA ABHIJIT KHILARI BANKURA. -

District Disaster Management Plan Bankura ( 2020-2021 )
DISTRICT DISASTER MANAGEMENT PLAN BANKURA ( 2020-2021 ) Prepared by: DISTRICT DISASTER MANAGEMENT CELL, BANKURA WEST BENGAL INDEX CHAPTER No. CONTENT Page No. Chapter 1 Introduction 1 -13 Chapter 2 Hazard, Vulnerability, Capacity and Risk Assessment (HVCRA) 14 – 24 Chapter 3 Institutional Arrangement for Disaster Management (DM) 25 – 27 Chapter 4 Prevention and Mitigation Measures 28 – 34 Chapter 5 Preparedness Measures 35 - 50 Chapter 6 Capacity Building and Training Measures 51 – 57 Chapter 7 Response and Relief Measures 58 – 71 Chapter 8 Reconstruction, Rehabilitation and Recovery 72 – 76 Chapter 9 Financial Resources for Implementation of DDMP 77 Chapter 10 Procedure and Methodology for Monitoring, Evaluation, Updation and 78 – 79 Maintenance of DDMP Chapter 11 Co-ordination Mechanism for Implementation of DDMP 80 – 82 Chapter 12 Standard Operating Procedures (SOPs ) and Check List 83 – 99 Chapter 13 Important Telephone Numbers 100 - 104 AnnexURE List of Events or Melas where large crowds gather with event date and Annexure 1 location 105 - 107 Annexure 2 List of Petrol Pump 108 - 109 Annexure 3 List of LPG go-down 110 - 111 Annexure 4 List of Inflammable Industry 112 - 115 Annexure 5 Vulnerability Report 116 Annexure 6 Large Crowd 117-119 Annexure 7 Heritage Building 120 Annexure 8 MAJOR DISASTER & FINANCIAL LOSS DURING LAST FINANCIAL YEAR 121 Annexure 9 LIST OF EQUPMENTS WHICH MAY BE PROCURED IN THE NEXT YEAR 122 CHAPTER-1 INTRODUCTION Bankura though being a rain fed district, it is widely known as the drought prone district of the State. Drought is a regular feature in the North-West part of the district covering Chhatna, Saltora, Gangajalghati, Barjora, Bankura-I, Bankura-II, Mejia, Indpur, Hirbandh & Ranibandh Blocks. -

Dpbankura58820.Pdf
Sl. No. CONTENT Page No. 1 Introduction 1 2 Administrative Map of the District 2 – 5 3 District Profile 6 – 12 4 Preparedness – District Disaster Management Cell Emergency Contingency Plan 13 – 17 Stock position of relief materials 18 Identification of temporary cyclone / flood shelters 19 – 23 5 Preparedness – CIVIL DEFENCE 24 - 28 6 Preparedness – HEALTH 29 – 56 7 Preparedness – IRRIGATION 57 – 62 8 Preparedness – AGRICULTURE 63 – 69 9 Preparedness – ANIMAL RESOURCES 70 – 78 DEVELOPMENT 10 Preparedness – WBSEDCL 79 – 81 11 Preparedness – SP (DIB) 82 – 92 12 Preparedness – FOOD & SUPPLY 93 - 94 13 Preparedness – PUBLIC HEALTH ENGINEERING 95 – 98 14 Preparedness – HORTICULTURE 99 – 102 15 Dam Safety – KANSABATI DIVISION-II 103 - 106 16 Important Telephone Numbers and e-mails 107 – 110 17 Preparedness Checklist for Various Departments 111 - 115 INTRODUCTION Bankura though being a rain fed district, it is widely known as the drought prone district of the State. Drought is a regular feature in the North-West part of the district covering Chhatna, Saltora, Gangajalghati, Barjora, Bankura-I, Bankura-II, Mejia, Indpur, Hirbandh & Ranibandh Blocks. Though this district receives good amount of rainfall, around 1400 mm. annually, is received per year yet cultivation and production of crop primarily depends on constricted period of erratic rainfall. About 80% to 90% rainfall is generally received by the district from June to September depending on the onset of monsoon. A conspicuous feature of this district is the absence of significant rainfall in the month of September and October. High runoff rate of rain water, inadequate storage facilities of the surface – runoff and low water holding capacity of the soil accelerate the drought situation.