Researchmatters Abstracts on Clinical Use of Misonix Bonescalpel®
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modified Plate-Only Open-Door Laminoplasty Versus Laminectomy and Fusion for the Treatment of Cervical Stenotic Myelopathy
n Feature Article Modified Plate-only Open-door Laminoplasty Versus Laminectomy and Fusion for the Treatment of Cervical Stenotic Myelopathy LILI YANG, MD; YIFEI GU, MD; JUEQIAN SHI, MD; RUI GAO, MD; YANG LIU, MD; JUN LI, MD; WEN YUAN, MD, PHD abstract Full article available online at Healio.com/Orthopedics. Search: 20121217-23 The purpose of this study was to compare modified plate-only laminoplasty and lami- nectomy and fusion to confirm which of the 2 surgical modalities could achieve a better decompression outcome and whether a significant difference was found in postopera- tive complications. Clinical data were retrospectively reviewed for 141 patients with cervical stenotic myelopathy who underwent plate-only laminoplasty and laminectomy and fusion between November 2007 and June 2010. The extent of decompression was assessed by measuring the cross-sectional area of the dural sac and the distance of spinal cord drift at the 3 most narrowed levels on T2-weighted magnetic resonance imaging. Clinical outcomes and complications were also recorded and compared. Significant en- largement of the dural sac area and spinal cord drift was achieved and well maintained in both groups, but the extent of decompression was greater in patients who underwent Figure: T2-weighted magnetic resonance image laminectomy and fusion; however, a greater decompression did not seem to produce a showing the extent of decompression assessed by better clinical outcome. No significant difference was observed in Japanese Orthopaedic measuring the cross-sectional area of the dural sac Association and Nurick scores between the 2 groups. Patients who underwent plate-only (arrow). laminoplasty showed a better improvement in Neck Dysfunction Index and visual ana- log scale scores. -

Analysis of the Cervical Spine Alignment Following Laminoplasty and Laminectomy
Spinal Cord (1999) 37, 20± 24 ã 1999 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/99 $12.00 http://www.stockton-press.co.uk/sc Analysis of the cervical spine alignment following laminoplasty and laminectomy Shunji Matsunaga1, Takashi Sakou1 and Kenji Nakanisi2 1Department of Orthopaedic Surgery, Faculty of Medicine, Kagoshima University; 2Department of Mechanical Engineering, Faculty of Engineering, Kagoshima University, Sakuragaoka, Kagoshima, Japan Very little detailed biomechanical examination of the alignment of the cervical spine following laminoplasty has been reported. We performed a comparative study regarding the buckling- type alignment that follows laminoplasty and laminectomy to know the mechanical changes in the alignment of the cervical spine. Lateral images of plain roentgenograms of the cervical spine were put into a computer and examined using a program we developed for analysis of the buckling-type alignment. Sixty-four patients who underwent laminoplasty and 37 patients who underwent laminectomy were reviewed retrospectively. The subjects comprised patients with cervical spondylotic myelopathy (CSM) and those with ossi®cation of the posterior longitudinal ligament (OPLL). The postoperative observation period was 6 years and 7 months on average after laminectomy, and 5 years and 6 months on average following laminoplasty. Development of the buckling-type alignment was found in 33% of patients following laminectomy and only 6% after laminoplasty. Development of buckling-type alignment following laminoplasty appeared markedly less than following laminectomy in both CSM and OPLL patients. These results favor laminoplasty over laminectomy from the aspect of mechanics. Keywords: laminoplasty; laminectomy; buckling; kyphosis; swan-neck deformity Introduction In 1930, Eiselberg1 reported a case of postoperative of postoperative abnormal alignment from the aspect kyphosis of the spine following laminectomy from the of the presence or absence of buckling-type alignment. -
Spinal Cord Injury: Is Monitoring from the Injury Site the Future? Samira Saadoun and Marios C
Saadoun and Papadopoulos Critical Care (2016) 20:308 DOI 10.1186/s13054-016-1490-3 VIEWPOINT Open Access Spinal cord injury: is monitoring from the injury site the future? Samira Saadoun and Marios C. Papadopoulos* within 24 h compared with >24 h after cervical TSCI Abstract [4]. This study was underpowered, not randomized, and This paper challenges the current management of not blinded. In the UK [3] and internationally [2, 5] acute traumatic spinal cord injury based on our there is no consensus on the timing or even the role of experience with monitoring from the injury site in the surgery for TSCI. Below, we argue that early surgery is neurointensive care unit. We argue that the concept controversial because surgeons perform bony decom- of bony decompression is inadequate. The concept of pression, but fail to relieve the dural compression. optimum spinal cord perfusion pressure, which differs between patients, is introduced. Such variability Medical and nursing management suggests individualized patient treatment. Failing to There are no drugs that improve outcome after TSCI. The optimize spinal cord perfusion limits the entry of North American Spinal Cord Injury Studies suggested that systemically administered drugs into the injured cord. methylprednisolone given within 8 h after TSCI improves We conclude that monitoring from the injury site outcome [6, 7], but their findings have been criticized; helps optimize management and should be subjected methylprednisolone is no longer standard of care [3, 8, 9]. to a trial to determine whether it improves outcome. The optimum mean arterial pressure (MAP) after TSCI is Keywords: Blood pressure, CNS injury, Clinical trial, unknown. -

Acute High Cervical Disc Herniation: a Confounding Presentation and New Algorithm to Ensure Correct Diagnosis
Central Annals of Emergency Surgery Bringing Excellence in Open Access Case Report *Corresponding author Bijan J. Ameri, Department of Orthopaedic Surgery, Broward Health Medical Center, 1227 SW 19th Ave. Fort Acute High Cervical Disc Lauderdale, FL 33312, USA, Email: Submitted: 13 February 2018 Herniation: A Confounding Accepted: 27 February 2018 Published: 28 February 2018 Copyright Presentation and New © 2018 Ameri et al. ISSN: 2573-1017 Algorithm to Ensure Correct OPEN ACCESS Diagnosis Keywords William A. Kunkle1, Bijan J. Ameri2*, Michael O. Madden2, • Cervical disc; Cervical spine surgery; Discectomy; Spinal decompression surgery; Cervical disc 3 4 Stuart H. Hershman , and Justin J. Park herniation; Cervical; Spine; High disc herniation; 1Department of Orthopaedic Surgery, Oregon Health and Science University, USA Stroke; Dissection; CTA; MRA 2Department of Orthopaedic Surgery, Broward Health Medical Center, USA 3Department of Orthoapaedic Surgery, Massachussetts General Hospital, USA 4Department of Orthopaedic Surgery, Maryland Spine Center at Mercy Hospital, USA Abstract High cervical disc herniation (C2/3 and C3/4) is a rare and potentially debilitating injury. Most cervical disc herniations occur at C5/6, or C6/7; less than 1% occurs at C2/3 and only 4% to 8% at C3/4. Patients with a high cervical disc herniation can present with headache, neck pain, and unilateral numbness and weakness. Diagnostic tests such as non-contrast computed tomography (CT) of the brain and angiogram of the neck are commonly utilized to rule out cerebral vascular accident (CVA) and/or carotid artery dissection; these pathologies can present with similar symptoms, however these commonly obtained tests will often fail to diagnose a high cervical disc herniation. -
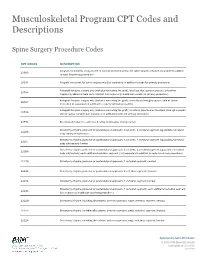
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Differences Between Subtotal Corpectomy and Laminoplasty for Cervical Spondylotic Myelopathy
Spinal Cord (2010) 48, 214–220 & 2010 International Spinal Cord Society All rights reserved 1362-4393/10 $32.00 www.nature.com/sc ORIGINAL ARTICLE Differences between subtotal corpectomy and laminoplasty for cervical spondylotic myelopathy S Shibuya1, S Komatsubara1, S Oka2, Y Kanda1, N Arima1 and T Yamamoto1 1Department of Orthopaedic Surgery, School of Medicine, Kagawa University, Kagawa, Japan and 2Oka Orthopaedic and Rehabilitation Clinic, Kagawa, Japan Objective: This study aimed to obtain guidelines for choosing between subtotal corpectomy (SC) and laminoplasty (LP) by analysing the surgical outcomes, radiological changes and problems associated with each surgical modality. Study Design: A retrospective analysis of two interventional case series. Setting: Department of Orthopaedic Surgery, Kagawa University, Japan. Methods: Subjects comprised 34 patients who underwent SC and 49 patients who underwent LP. SC was performed by high-speed drilling to remove vertebral bodies. Autologous strut bone grafting was used. LP was performed as an expansive open-door LP. The level of decompression was from C3 to C7. Clinical evaluations included recovery rate (RR), frequency of C5 root palsy after surgery, re-operation and axial pain. Radiographic assessments included sagittal cervical alignment and bone union. Results: Comparisons between the two groups showed no significant differences in age at surgery, preoperative factors, RR and frequency of C5 palsy. Progression of kyphotic changes, operation time and volumes of blood loss and blood transfusion were significantly greater in the SC (two- or three- level) group. Six patients in the SC group required additional surgery because of pseudoarthrosis, and four patients underwent re-operation because of adjacent level disc degeneration. -

Clinical Guidelines
CLINICAL GUIDELINES Interventional Pain Management Services Version 1.0.2019 Clinical guidelines for medical necessity review of comprehensive musculoskeletal management services. © 2019 eviCore healthcare. All rights reserved. Regence: Comprehensive Musculoskeletal Management Guidelines V1.0.2019 Interventional Pain Management CMM-200: Epidural Steroid Injections (ESI) 3 CMM-201: Facet Joint Injections/Medial Branch Blocks 17 CMM-202: Trigger Point Injections 21 CMM-203: Sacroiliac Joint Injections 32 CMM-204: Prolotherapy 37 CMM-207: Epidural Adhesiolysis 40 CMM-208: Radiofrequency Joint Ablations/Denervations 44 CMM-209: Regional Sympathetic Blocks 51 CMM 210: Implantable Intrathecal Drug Delivery Systems 57 CMM-211: Spinal Cord Stimulators 65 CMM-308: Thermal Intradiscal Procedures 66 CMM-310: Manipulation of the Spine Under Anesthesia 71 ______________________________________________________________________________________________________ © 2019 eviCore healthcare. All Rights Reserved. Page 2 of 73 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Regence: Comprehensive Musculoskeletal Management Guidelines V1.0.2019 CMM-200: Epidural Steroid Injections (ESI) CMM-200.1: Definitions 4 CMM-200.2: General Guidelines 5 CMM-200.3: Indications: Selective Nerve Root Block (SNRB) 6 CMM-200.4: Indications: Epidural Steroid Injections 7 CMM-200.5: Non-Indications: SNRB 8 CMM-200.6: Non-Indications: ESI 8 ® CMM-200.7: Procedure (CPT ) Codes 9 CMM-200.8: References 10 ______________________________________________________________________________________________________ -

TESSYS Technique with Small Grade of Facetectomy Has Potential Biomechanical Advantages Compared to the In-Out TED with Intact Articular Process : an In-Silico Study
TESSYS Technique With Small Grade of Facetectomy Has Potential Biomechanical Advantages Compared to the In-Out TED With Intact Articular Process : An In-Silico Study Jingchi Li West China Hospital/West China School of Medicine for Sichuan University Chen Xu Changzheng Hospital Aliated to the Naval Medical University Xiaoyu Zhang Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Zhipeng Xi Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Mengnan Liu Macau University of Science and Technology Zhongxin Fang Xihua University Nan Wang Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Lin Xie ( [email protected] ) Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Yueming Song West China Hospital/West China School of Medicine for Sichuan University Research Article Keywords: Biomechanical deterioration, Transforaminal endoscopic discectomy, Endoscopic dynamic drill, Facetectomy, Iatrogenic annulus injury Posted Date: April 26th, 2021 Page 1/27 DOI: https://doi.org/10.21203/rs.3.rs-429749/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Musculoskeletal Disorders on July 10th, 2021. See the published version at https://doi.org/10.1186/s12891-021-04504-1. Page 2/27 Abstract Background: The facetectomy was reported as an important procedure in both in-out and out-in (i.e. transforaminal endoscopic spine system (TESSYS)) techniques in the transforaminal endoscopic discectomy (TED), and which was also related to the deterioration of postoperative biomechanical environment and related poor prognosis. -

Priority Health Spine and Joint Code List
Priority Health Joint Services Code List Category CPT® Code CPT® Code Description Joint Services 23000 Removal of subdeltoid calcareous deposits, open Joint Services 23020 Capsular contracture release (eg, Sever type procedure) Joint Services 23120 Claviculectomy; partial Joint Services 23130 Acromioplasty or acromionectomy, partial, with or without coracoacromial ligament release Joint Services 23410 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; acute Joint Services 23412 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open;chronic Joint Services 23415 Coracoacromial ligament release, with or without acromioplasty Joint Services 23420 Reconstruction of complete shoulder (rotator) cuff avulsion, chronic (includes acromioplasty) Joint Services 23430 Tenodesis of long tendon of biceps Joint Services 23440 Resection or transplantation of long tendon of biceps Joint Services 23450 Capsulorrhaphy, anterior; Putti-Platt procedure or Magnuson type operation Joint Services 23455 Capsulorrhaphy, anterior;with labral repair (eg, Bankart procedure) Joint Services 23460 Capsulorrhaphy, anterior, any type; with bone block Joint Services 23462 Capsulorrhaphy, anterior, any type;with coracoid process transfer Joint Services 23465 Capsulorrhaphy, glenohumeral joint, posterior, with or without bone block Joint Services 23466 Capsulorrhaphy, glenohumeral joint, any type multi-directional instability Joint Services 23470 ARTHROPLASTY, GLENOHUMERAL JOINT; HEMIARTHROPLASTY ARTHROPLASTY, GLENOHUMERAL JOINT; TOTAL SHOULDER [GLENOID -

Medicure Instruments
MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-503 MI-502 MI-501 KOCHER’S MOSQUITO FORCEPS FORCEPS SPENCER WELLS ARTERY FORCEPS STAINLESS STEEL STRAIGHT ARTERY MI-504 MI-505 MI-506 MI-507 MI-508 KOCHER’S DISSECTING FORCEPS DISSECTING FORCEPS RUSSIAN DISSECTING FINE DISSECTING FORCEPS STAINLESS STEEL - PLAIN STAINLESS STEEL - TOOTH FORCEPS FORCEPS - PLAIN CURVED ARTERY MI-509 MI-510 MI-511 TOWEL CLIP FINE DISSECTING DENNIS BROWNE TOWEL FORCEPS CROSS-ACTION FORCEPS - TOOTH DISSECTING FORCEPS BACKHAUS GENERAL SURGERY INSTRUMENTS MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-512 MI-513 MI-513 MI-514 LISTER SINUS B.P. HANDLE NO. 3 B.P. HANDLE NO. 4 B.P. HANDLE NO. 7 MALLEBLE PROBE DRESSING FORCEPS WITH EYE MI-515 MI-5164 MI-514 BOZEMANN KILNER MI-517 MAYO HEGARS NEEDLE HOLDERS NEEDLE HOLDERS FINE DRESSING SCISSORS NEEDLE HOLDERS STRAIGHT STRAIGHT STRAIGHT (SHARP x BLUNT) STRAIGHT STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL MI-521 MI-518 MI-519 MI-520 STITCH RIBBON SCISSORS DRESSING SCISSORS IRIS SCISSORS KNAPP SCISSORS STRAIGHT STRAIGHT (SHARP x SHARP) STRAIGHT STRAIGHT STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL STAINLESS STEEL GENERAL SURGERY INSTRUMENTS MEDICURE edicure Instruments MED CURE MedicurM e Instruments MI-523 MI-524 MI-525 STEVENS SCISSORS MAYO SCISSORS GREEN BERG SCISSORS MI-522 STRAIGHT STRAIGHT (KILNER) METZENBAUM SCISSORS STAINLESS STEEL STRAIGHT STAINLESS STEEL STRAIGHT STAINLESS STEEL STAINLESS STEEL MI-528 MI-529 ALLIS TISSUE POTT’S ANGLED GRASPING FORCEPS MI-526 -

Biomechanical Analysis of Posterior Ligaments of Cervical Spine and Laminoplasty
applied sciences Article Biomechanical Analysis of Posterior Ligaments of Cervical Spine and Laminoplasty Norihiro Nishida 1 , Muzammil Mumtaz 2, Sudharshan Tripathi 2, Amey Kelkar 2, Takashi Sakai 1 and Vijay K. Goel 2,* 1 Department of Orthopedic Surgery, Yamaguchi University Graduate School of Medicine, 1-1-1 Minami-Kogushi, Ube, Yamaguchi Prefecture 755-8505, Japan; [email protected] (N.N.); [email protected] (T.S.) 2 Engineering Center for Orthopaedic Research Excellence (E-CORE), Departments of Bioengineering and Orthopaedics, The University of Toledo, Toledo, OH 43606, USA; [email protected] (M.M.); [email protected] (S.T.); [email protected] (A.K.) * Correspondence: [email protected]; Tel.: +1-(419)-530-8035 Abstract: Cervical laminoplasty is a valuable procedure for myelopathy but it is associated with complications such as increased kyphosis. The effect of ligament damage during cervical lamino- plasty on biomechanics is not well understood. We developed the C2–C7 cervical spine finite element model and simulated C3–C6 double-door laminoplasty. Three models were created (a) in- tact, (b) laminoplasty-pre (model assuming that the ligamentum flavum (LF) between C3–C6 was preserved during surgery), and (c) laminoplasty-res (model assuming that the LF between C3–C6 was resected during surgery). The models were subjected to physiological loading, and the range of motion (ROM), intervertebral nucleus stress, and facet contact forces were analyzed under flex- ion/extension, lateral bending, and axial rotation. The maximum change in ROM was observed Citation: Nishida, N.; Mumtaz, M.; under flexion motion. Under flexion, ROM in the laminoplasty-pre model increased by 100.2%, Tripathi, S.; Kelkar, A.; Sakai, T.; Goel, 111.8%, and 98.6% compared to the intact model at C3–C4, C4–C5, and C5–C6, respectively. -

Indications for Fusion Following Decompression for Lumbar Spinal Stenosis
Neurosurg Focus 3 (2): Article 2, 1997 Indications for fusion following decompression for lumbar spinal stenosis Mark W. Fox, M.D., and Burton M. Onofrio, M.D. Neurosurgery Associates, Limited, St. Paul, Minnesota; and Department of Neurosurgery, The Mayo Clinic, Rochester, Minnesota Degenerative lumbar spinal stenosis is a common condition affecting middle-aged and elderly people. Significant controversy exists concerning the appropriate indications for fusion following decompressive surgery. The purpose of this report is to compare the clinical outcomes of patients who were and were not treated with fusion following decompressive laminectomy for spinal stenosis and to identify whether fusion was beneficial. The authors conclude that patients in whom concomitant fusion procedures were performed fared better than patients who were treated by means of decompression alone when evidence of radiological instability existed preoperatively. Key Words * lumbar spinal stenosis * laminectomy * fusion * indication The decision to perform fusion following decompression for degenerative lumbar spinal stenosis has been studied by many authors.[14,16,30,52,69] Unfortunately, no clear consensus has been reached to determine which patients are most likely to benefit from a concomitant lumbar fusion. Patient satisfaction following lumbar decompression alone ranges from 59 to 96%, with early surgical failures resulting from inadequate decompression and preoperative lumbar instability.[2,4,8,12,21,22,26,29,31,34,65] Late recurrence of back or leg problems may also result from acquired spinal instability. The goal of this study was to analyze clinical outcomes in patients treated with and without fusion following lumbar decompression to determine which patients benefited most. The ability to identify predictive factors for successful surgery with fusion would improve overall clinical results and decrease both early and late failures caused by persistent or acquired spinal instability.