Use of Corticosteroids
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Drugs List
^ ^ ^ ^ ^[ ^ The National Drugs List Of Syrian Arab Republic Sexth Edition 2006 ! " # "$ % &'() " # * +$, -. / & 0 /+12 3 4" 5 "$ . "$ 67"5,) 0 " /! !2 4? @ % 88 9 3: " # "$ ;+<=2 – G# H H2 I) – 6( – 65 : A B C "5 : , D )* . J!* HK"3 H"$ T ) 4 B K<) +$ LMA N O 3 4P<B &Q / RS ) H< C4VH /430 / 1988 V W* < C A GQ ") 4V / 1000 / C4VH /820 / 2001 V XX K<# C ,V /500 / 1992 V "!X V /946 / 2004 V Z < C V /914 / 2003 V ) < ] +$, [2 / ,) @# @ S%Q2 J"= [ &<\ @ +$ LMA 1 O \ . S X '( ^ & M_ `AB @ &' 3 4" + @ V= 4 )\ " : N " # "$ 6 ) G" 3Q + a C G /<"B d3: C K7 e , fM 4 Q b"$ " < $\ c"7: 5) G . HHH3Q J # Hg ' V"h 6< G* H5 !" # $%" & $' ,* ( )* + 2 ا اوا ادو +% 5 j 2 i1 6 B J' 6<X " 6"[ i2 "$ "< * i3 10 6 i4 11 6! ^ i5 13 6<X "!# * i6 15 7 G!, 6 - k 24"$d dl ?K V *4V h 63[46 ' i8 19 Adl 20 "( 2 i9 20 G Q) 6 i10 20 a 6 m[, 6 i11 21 ?K V $n i12 21 "% * i13 23 b+ 6 i14 23 oe C * i15 24 !, 2 6\ i16 25 C V pq * i17 26 ( S 6) 1, ++ &"r i19 3 +% 27 G 6 ""% i19 28 ^ Ks 2 i20 31 % Ks 2 i21 32 s * i22 35 " " * i23 37 "$ * i24 38 6" i25 39 V t h Gu* v!* 2 i26 39 ( 2 i27 40 B w< Ks 2 i28 40 d C &"r i29 42 "' 6 i30 42 " * i31 42 ":< * i32 5 ./ 0" -33 4 : ANAESTHETICS $ 1 2 -1 :GENERAL ANAESTHETICS AND OXYGEN 4 $1 2 2- ATRACURIUM BESYLATE DROPERIDOL ETHER FENTANYL HALOTHANE ISOFLURANE KETAMINE HCL NITROUS OXIDE OXYGEN PROPOFOL REMIFENTANIL SEVOFLURANE SUFENTANIL THIOPENTAL :LOCAL ANAESTHETICS !67$1 2 -5 AMYLEINE HCL=AMYLOCAINE ARTICAINE BENZOCAINE BUPIVACAINE CINCHOCAINE LIDOCAINE MEPIVACAINE OXETHAZAINE PRAMOXINE PRILOCAINE PREOPERATIVE MEDICATION & SEDATION FOR 9*: ;< " 2 -8 : : SHORT -TERM PROCEDURES ATROPINE DIAZEPAM INJ. -

Docetaxel with Prednisone Or Prednisolone for the Treatment of Prostate Cancer ISSN 1366-5278 Feedback Your Views About This Report
Health Technology Assessment Health Technology Health Technology Assessment 2007; Vol. 11: No. 2 2007; 11: No. 2 Vol. Docetaxel with prednisone or prednisolone for the treatment of prostate cancer A systematic review and economic model of the clinical effectiveness and cost-effectiveness of docetaxel in combination with prednisone or prednisolone for the treatment of hormone-refractory metastatic prostate cancer Feedback The HTA Programme and the authors would like to know R Collins, E Fenwick, R Trowman, R Perard, your views about this report. The Correspondence Page on the HTA website G Norman, K Light, A Birtle, S Palmer (http://www.hta.ac.uk) is a convenient way to publish and R Riemsma your comments. If you prefer, you can send your comments to the address below, telling us whether you would like us to transfer them to the website. We look forward to hearing from you. January 2007 The National Coordinating Centre for Health Technology Assessment, Mailpoint 728, Boldrewood, Health Technology Assessment University of Southampton, NHS R&D HTA Programme Southampton, SO16 7PX, UK. HTA Fax: +44 (0) 23 8059 5639 Email: [email protected] www.hta.ac.uk http://www.hta.ac.uk ISSN 1366-5278 HTA How to obtain copies of this and other HTA Programme reports. An electronic version of this publication, in Adobe Acrobat format, is available for downloading free of charge for personal use from the HTA website (http://www.hta.ac.uk). A fully searchable CD-ROM is also available (see below). Printed copies of HTA monographs cost £20 each (post and packing free in the UK) to both public and private sector purchasers from our Despatch Agents. -

Prednisolone Versus Dexamethasone for Croup: a Randomized Controlled Trial Colin M
Prednisolone Versus Dexamethasone for Croup: a Randomized Controlled Trial Colin M. Parker, MBChB, DCH, MRCPCH, FACEM,a,b Matthew N. Cooper, BCA, BSc, PhDc OBJECTIVES: The use of either prednisolone or low-dose dexamethasone in the treatment of abstract childhood croup lacks a rigorous evidence base despite widespread use. In this study, we compare dexamethasone at 0.6 mg/kg with both low-dose dexamethasone at 0.15 mg/kg and prednisolone at 1 mg/kg. METHODS: Prospective, double-blind, noninferiority randomized controlled trial based in 1 tertiary pediatric emergency department and 1 urban district emergency department in Perth, Western Australia. Inclusions were age .6 months, maximum weight 20 kg, contactable by telephone, and English-speaking caregivers. Exclusion criteria were known prednisolone or dexamethasone allergy, immunosuppressive disease or treatment, steroid therapy or enrollment in the study within the previous 14 days, and a high clinical suspicion of an alternative diagnosis. A total of 1252 participants were enrolled and randomly assigned to receive dexamethasone (0.6 mg/kg; n = 410), low-dose dexamethasone (0.15 mg/kg; n = 410), or prednisolone (1 mg/kg; n = 411). Primary outcome measures included Westley Croup Score 1-hour after treatment and unscheduled medical re-attendance during the 7 days after treatment. RESULTS: Mean Westley Croup Score at baseline was 1.4 for dexamethasone, 1.5 for low-dose dexamethasone, and 1.5 for prednisolone. Adjusted difference in scores at 1 hour, compared with dexamethasone, was 0.03 (95% confidence interval 20.09 to 0.15) for low-dose dexamethasone and 0.05 (95% confidence interval 20.07 to 0.17) for prednisolone. -

Penetration of Synthetic Corticosteroids Into Human Aqueous Humour
Eye (1990) 4, 526--530 Penetration of Synthetic Corticosteroids into Human Aqueous Humour C. N. 1. McGHEE,1.3 D. G. WATSON, 3 1. M. MIDGLEY, 3 M. 1. NOBLE, 2 G. N. DUTTON, z A. I. FERNl Glasgow Summary The penetration of prednisolone acetate (1%) and fluorometholone alcohol (0.1%) into human aqueous humour following topical application was determined using the very sensitive and specific technique of Gas Chromatography with Mass Spec trometry (GCMS). Prednisolone acetate afforded peak mean concentrations of 669.9 ng/ml within two hours and levels of 28.6 ng/ml in aqueous humour were detected almost 24 hours post application. The peak aqueous humour level of flu orometholone was S.lng/ml. The results are compared and contrasted with the absorption of dexamethasone alcohol (0.1%), betamethasone sodium phosphate (0.1 %) and prednisolone sodium phosphate (0.5%) into human aqueous humour. Topical corticosteroid preparations have been prednisolone acetate (1.0%) and fluorometh used widely in ophthalmology since the early alone alcohol (0.1 %) (preliminary results) 1960s and over the last 10 years the choice of into the aqueous humour of patients under preparations has become larger and more going elective cataract surgery. varied. Unfortunately, data on the intraocular penetration of these steroids in humans has SUbjects and Methods not paralleled the expansion in the number of Patients who were scheduled to undergo rou available preparations; indeed until recently, tine cataract surgery were recruited to the estimation of intraocular penetration has study and informed consent was obtained in been reliant upon extrapolation of data from all cases (n=88), Patients with corneal disease animal models (see Watson et ai., 1988, for or inflammatory ocular conditions which bibliography). -

Mifepristone
1. NAME OF THE MEDICINAL PRODUCT Mifegyne 200 mg tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 200-mg mifepristone. For the full list of excipients, see section 6.1 3. PHARMACEUTICAL FORM Tablet. Light yellow, cylindrical, bi-convex tablets, with a diameter of 11 mm with “167 B” engraved on one side. 4. CLINICAL PARTICULARS For termination of pregnancy, the anti-progesterone mifepristone and the prostaglandin analogue can only be prescribed and administered in accordance with New Zealand’s abortion laws and regulations. 4.1 Therapeutic indications 1- Medical termination of developing intra-uterine pregnancy. In sequential use with a prostaglandin analogue, up to 63 days of amenorrhea (see section 4.2). 2- Softening and dilatation of the cervix uteri prior to surgical termination of pregnancy during the first trimester. 3- Preparation for the action of prostaglandin analogues in the termination of pregnancy for medical reasons (beyond the first trimester). 4- Labour induction in fetal death in utero. In patients where prostaglandin or oxytocin cannot be used. 4.2 Dose and Method of Administration Dose 1- Medical termination of developing intra-uterine pregnancy The method of administration will be as follows: • Up to 49 days of amenorrhea: 1 Mifepristone is taken as a single 600 mg (i.e. 3 tablets of 200 mg each) oral dose, followed 36 to 48 hours later, by the administration of the prostaglandin analogue: misoprostol 400 µg orally or per vaginum. • Between 50-63 days of amenorrhea Mifepristone is taken as a single 600 mg (i.e. 3 tablets of 200 mg each) oral dose, followed 36 to 48 hours later, by the administration of misoprostol. -

Endocrine Drugs
PharmacologyPharmacologyPharmacology DrugsDrugs thatthat AffectAffect thethe EndocrineEndocrine SystemSystem TopicsTopicsTopics •• Pituitary Pituitary DrugsDrugs •• Parathyroid/Thyroid Parathyroid/Thyroid DrugsDrugs •• Adrenal Adrenal DrugsDrugs •• Pancreatic Pancreatic DrugsDrugs •• Reproductive Reproductive DrugsDrugs •• Sexual Sexual BehaviorBehavior DrugsDrugs FunctionsFunctionsFunctions •• Regulation Regulation •• Control Control GlandsGlandsGlands ExocrineExocrine EndocrineEndocrine •• Secrete Secrete enzymesenzymes •• Secrete Secrete hormoneshormones •• Close Close toto organsorgans •• Transport Transport viavia bloodstreambloodstream •• Require Require receptorsreceptors NervousNervous EndocrineEndocrine WiredWired WirelessWireless NeurotransmittersNeurotransmitters HormonesHormones ShortShort DistanceDistance LongLong Distance Distance ClosenessCloseness ReceptorReceptor Specificity Specificity RapidRapid OnsetOnset DelayedDelayed Onset Onset ShortShort DurationDuration ProlongedProlonged Duration Duration RapidRapid ResponseResponse RegulationRegulation MechanismMechanismMechanism ofofof ActionActionAction HypothalamusHypothalamusHypothalamus HypothalamicHypothalamicHypothalamic ControlControlControl PituitaryPituitaryPituitary PosteriorPosteriorPosterior PituitaryPituitaryPituitary Target Actions Oxytocin Uterus ↑ Contraction Mammary ↑ Milk let-down ADH Kidneys ↑ Water reabsorption AnteriorAnteriorAnterior PituitaryPituitaryPituitary Target Action GH Most tissue ↑ Growth TSH Thyroid ↑ TH secretion ACTH Adrenal ↑ Cortisol Cortex -

Opposing Effects of Dehydroepiandrosterone And
European Journal of Endocrinology (2000) 143 687±695 ISSN 0804-4643 EXPERIMENTAL STUDY Opposing effects of dehydroepiandrosterone and dexamethasone on the generation of monocyte-derived dendritic cells M O Canning, K Grotenhuis, H J de Wit and H A Drexhage Department of Immunology, Erasmus University Rotterdam, The Netherlands (Correspondence should be addressed to H A Drexhage, Lab Ee 838, Department of Immunology, Erasmus University, PO Box 1738, 3000 DR Rotterdam, The Netherlands; Email: [email protected]) Abstract Background: Dehydroepiandrosterone (DHEA) has been suggested as an immunostimulating steroid hormone, of which the effects on the development of dendritic cells (DC) are unknown. The effects of DHEA often oppose those of the other adrenal glucocorticoid, cortisol. Glucocorticoids (GC) are known to suppress the immune response at different levels and have recently been shown to modulate the development of DC, thereby influencing the initiation of the immune response. Variations in the duration of exposure to, and doses of, GC (particularly dexamethasone (DEX)) however, have resulted in conflicting effects on DC development. Aim: In this study, we describe the effects of a continuous high level of exposure to the adrenal steroid DHEA (1026 M) on the generation of immature DC from monocytes, as well as the effects of the opposing steroid DEX on this development. Results: The continuous presence of DHEA (1026 M) in GM-CSF/IL-4-induced monocyte-derived DC cultures resulted in immature DC with a morphology and functional capabilities similar to those of typical immature DC (T cell stimulation, IL-12/IL-10 production), but with a slightly altered phenotype of increased CD80 and decreased CD43 expression (markers of maturity). -
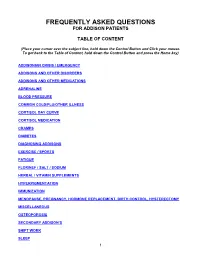
Frequently Asked Questions for Addison Patients
FREQUENTLY ASKED QUESTIONS FOR ADDISON PATIENTS TABLE OF CONTENT (Place your cursor over the subject line, hold down the Control Button and Click your mouse. To get back to the Table of Content, hold down the Control Button and press the Home key) ADDISONIAN CRISIS / EMERGENCY ADDISONS AND OTHER DISORDERS ADDISONS AND OTHER MEDICATIONS ADRENALINE BLOOD PRESSURE COMMON COLD/FLU/OTHER ILLNESS CORTISOL DAY CURVE CORTISOL MEDICATION CRAMPS DIABETES DIAGNOSING ADDISONS EXERCISE / SPORTS FATIGUE FLORINEF / SALT / SODIUM HERBAL / VITAMIN SUPPLEMENTS HYPERPIGMENTATION IMMUNIZATION MENOPAUSE, PREGNANCY, HORMONE REPLACEMENT, BIRTH CONTROL, HYSTERECTOMY MISCELLANEOUS OSTEOPOROSIS SECONDARY ADDISON’S SHIFT WORK SLEEP 1 STRESS DOSING SURGICAL, MEDICAL, DENTAL PROCEDURES THYROID TRAVEL WEIGHT GAIN 2 ADDISONIAN CRISIS / EMERGENCY How do you know when to call an ambulance? If you are careful, you should not have to call an ambulance. If someone with adrenal insufficiency has gastrointestinal problems and is unable to keep down their cortisol or other glucocorticoid for more than 24 hrs, they should be taken to an emergency department so they can be given intravenous solucortef and saline. It is not appropriate to wait until they are so ill that they cannot be taken to the hospital by a family member. If the individual is unable to retain anything by mouth and is very ill, or if they have had a sudden stress such as a fall or an infection, then it would be necessary for them to go by ambulance as soon as possible. It is important that you should have an emergency kit at home and that someone in the household knows how to use it. -

6. Endocrine System 6.1 - Drugs Used in Diabetes Also See SIGN 116: Management of Diabetes, 2010
1 6. Endocrine System 6.1 - Drugs used in Diabetes Also see SIGN 116: Management of Diabetes, 2010 http://www.sign.ac.uk/guidelines/fulltext/116 Insulin Prescribing Guidance in Type 2 Diabetes http://www.fifeadtc.scot.nhs.uk/media/6978/insulin-prescribing-in-type-2-diabetes.pdf 6.1.1 Insulins (Type 2 Diabetes) 6.1.1.1 Short Acting Insulins 1st Choice S – Insuman ® Rapid (Human Insulin) S – Humulin S ® S – Actrapid ® 2nd Choice S – Insulin Aspart (NovoRapid ®) (Insulin Analogues) S – Insulin Lispro (Humalog ®) 6.1.1.2 Intermediate and Long Acting Insulins 1st Choice S – Isophane Insulin (Insuman Basal ®) (Human Insulin) S – Isophane Insulin (Humulin I ®) S – Isophane Insulin (Insulatard ®) 2nd Choice S – Insulin Detemir (Levemir ®) (Insulin Analogues) S – Insulin Glargine (Lantus ®) Biphasic Insulins 1st Choice S – Biphasic Isophane (Human Insulin) (Insuman Comb ® ‘15’, ‘25’,’50’) S – Biphasic Isophane (Humulin M3 ®) 2nd Choice S – Biphasic Aspart (Novomix ® 30) (Insulin Analogues) S – Biphasic Lispro (Humalog ® Mix ‘25’ or ‘50’) Prescribing Points For patients with Type 1 diabetes, insulin will be initiated by a diabetes specialist with continuation of prescribing in primary care. Insulin analogues are the preferred insulins for use in Type 1 diabetes. Cartridge formulations of insulin are preferred to alternative formulations Type 2 patients who are newly prescribed insulin should usually be started on NPH isophane insulin, (e.g. Insuman Basal ®, Humulin I ®, Insulatard ®). Long-acting recombinant human insulin analogues (e.g. Levemir ®, Lantus ®) offer no significant clinical advantage for most type 2 patients and are much more expensive. In terms of human insulin. The Insuman ® range is currently the most cost-effective and preferred in new patients. -

Systolic Blood Pressure
Iatrogenic Cushing’s Syndrome secondary to the Combined Oral Contraceptive Pill in a patient with Congenital Adrenal Hyperplasia Satish Artham, Yaasir Mamoojee, Simon Ashwell. Department of Diabetes and Endocrinology, The James cook University Hospital, Middlesbrough, UK Introduction: Systolic blood pressure: Congenital Adrenal Hyperplasia (CAH) is a rare genetic disorder characterised by deficiency of cortisol and/or mineralocorticoid hormones with over production of sex steroids. 21-hydroxylase deficiency is the commonest cause of CAH accounting for 95% of cases1,2. Severe form of classic CAH occurs in 1 in 15,000 livebirths worldwide3,4. The goals of treating 21-hydroxylase deficiency in women is to replace the deficient steroid hormones, to lower the adrenal precursors and sex steroids. Most commonly used regimens are prednisolone once a day or hydrocortisone split into two or three doses. Case: Discussion: A 30 year old women with CAH diagnosed at birth was on replacement with hydrocortisone and fludrocortisone. She was investigated for ongoing diarrhoea Cortisol is the main glucocorticoid hormone, the majority of by the gastroenterologist and was subsequently diagnosed with Irritable Bowel which is circulated bound to Cortisol Binding Globulin (CBG). Syndrome (IBS). She was then started on buscopan and codeine phosphate for Only about 5% of the circulating cortisol is free. Cortisol action symptom relief. However during her menstrual cycle her abdominal symptoms is terminated by conversion into inactive forms by various were not sufficiently controlled. She was thus commenced on Microgynon, enzymes. It is mainly metabolised in the liver. It is reduced, a Combined Oral Contraceptive Pill (COCP). Within a year of initiation she oxidised and hydroxylated, the products of which are made developed cushingoid features, became hypertensive and started gaining weight. -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid.