Neopágina Diciembre 2018
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Need to Put Header/Logo In
IN THIS ISSUE: EDITOR’S NOTE EDITOR’S CHOICE NATIONAL NEWS STATE NEWS Dear Wetlanders, WETLAND SCIENCE The news stories over the past month have been overwhelming focused on the new NEWS Administration and political appointments. In my visits and phone conversations with RESOURCES & various federal, state, and local government staff, the one thing folks are unanimous PUBLICATIONS about is that we really just don’t know what to expect. So for now, we play a game of wait and see while internally strategizing new ways to continue moving our various POTPOURRI missions forward. CALENDAR OF EVENTS I personally predict a flurry of lawsuits over the next few years as we are experiencing a INDEX level of divisiveness in this country that we have not seen in several decades. Wetland regulations and jurisdictional determinations have a long history of being contested in the legal system – and I expect we’ll see new challenges on many fronts to existing policies as well as new ones such as the reissued Section 404 Nationwide Permits just To view the January released by the U.S. Army Corps of Engineers (see story in Editor’s Choice). issue of Wetland Breaking News as well as In the Editor’s Choice section this month, I have included a couple of stories regarding past issues on our U.S. Supreme Court cases. The first is a story about the dispute over which lower website, please click courts have jurisdiction to hear challenges to the Obama administration's Clean Water here. Rule. The second story is about a case where a couple from South Dakota challenged a USDA wetlands designation. -

National Marine Fisheries Service Endangered Species Act Section 7 Biological Opinion
NATIONAL MARINE FISHERIES SERVICE ENDANGERED SPECIES ACT SECTION 7 BIOLOGICAL OPINION Title: Biological Opinion on the U.S. Geological Survey's Marine Geophysical Survey by the RIV Hugh R. Sharp in the Northwest Atlantic Ocean and National Marine Fisheries Service Permits and Conservation Division's Issuance of an Incidental Harassment Authorization pursuant to Section 101(a)(5)(D) of the Marine Mammal Protection Act Consultation Conducted By: Endangered Species Act Interagency Cooperation Division, Office of Protected Resources, National Marine Fisheries Service, National Oceanic and Atmospheric Administration, U.S. Department of Commerce Action Agency: U.S. Geological Survey; Resource Evaluation Division; Bureau of Ocean Energy Management, U.S. Department of Interior; National Energy Te€hnology Laboratory, U.S. Department of Energy; and Permits and Conservation Division, Office of Protected Resources, National Marine Fisheries Service, National Oceanic and Atmospheric Administration, U.S. Department of Commerce Publisher: Office of Protected Resources, National Marine Fisheries Service, National Oceanic and Atmospheric Administration, U.S. Department of Commerce Approved: Donna S. Wieting Director, Office of Protected Resourc s Date: AUG a6 2018 Consultation Tracking number: FPR-2018-9263 Digital Object Identifier (DOI): This page left blank intentionally Biological Opinion for U.S. Geological Survey Seismic Survey in the Atlantic Ocean 2018 Tracking No. 2018-9263 TABLE OF CONTENTS Page 1 Introduction .......................................................................................................................... -
Forging a New Path
FORGING A NEW PATH, SWEET BRIAR TURNS TO THE FUTURE Dear Sweet Briar Alumnae, Throughout this spring semester, distinguished women musicians, writers and policy makers have streamed to the campus, in a series dubbed “At the Invitation of the President.” As you will read in this issue, the series started in January with a remarkable all-women ensemble of scholar-performers dedicated to excavating little-known string trios from the 17th and 18th century, and it ended the semester with a lecture by Bettina Ring, the secretary of agriculture and forestry for the Commonwealth. Sweet Briar was a working farm for most of its history, a fact that does not escape the secretary, both as an important legacy we share and cherish, but also as a resurgent possibility for the future — for Sweet Briar and Central Virginia. Through this series, one learns stunning things about women who shape history. A gradu- ate of Sweet Briar, Delia Taylor Sinkov ’34 was a top code breaker who supervised a group of women who worked silently — under an “omerta” never to be betrayed in one’s lifetime — to break the Japanese navy and army codes and eventually to help win the Battle of Midway. Ultimately, the number of code breakers surpassed 10,000. While America is a country that loves and shines light on its heroes, women have often stayed in the shadow of that gleaming light; they are history’s greatest omission. “Do you like doing the crossword puzzle?” Navy recruiters would ask the potential code breakers. “And are you engaged to be married?” If the answer to the former was a “yes” and to the lat- ter a “no,” then the women were recruited to the first wave of large-scale intelligence work upon which the nation would embark. -

4–6–01 Vol. 66 No. 67 Friday April 6, 2001 Pages 18185–18394
4–6–01 Friday Vol. 66 No. 67 April 6, 2001 Pages 18185–18394 VerDate 11-MAY-2000 18:47 Apr 05, 2001 Jkt 194001 PO 00000 Frm 00001 Fmt 4710 Sfmt 4710 E:\FR\FM\06APWS.LOC pfrm10 PsN: 06APWS 1 II Federal Register / Vol. 66, No. 67 / Friday, April 6, 2001 The FEDERAL REGISTER is published daily, Monday through SUBSCRIPTIONS AND COPIES Friday, except official holidays, by the Office of the Federal Register, National Archives and Records Administration, PUBLIC Washington, DC 20408, under the Federal Register Act (44 U.S.C. Subscriptions: Ch. 15) and the regulations of the Administrative Committee of Paper or fiche 202–512–1800 the Federal Register (1 CFR Ch. I). The Superintendent of Assistance with public subscriptions 512–1806 Documents, U.S. Government Printing Office, Washington, DC 20402 is the exclusive distributor of the official edition. General online information 202–512–1530; 1–888–293–6498 Single copies/back copies: The Federal Register provides a uniform system for making available to the public regulations and legal notices issued by Paper or fiche 512–1800 Federal agencies. These include Presidential proclamations and Assistance with public single copies 512–1803 Executive Orders, Federal agency documents having general FEDERAL AGENCIES applicability and legal effect, documents required to be published Subscriptions: by act of Congress, and other Federal agency documents of public interest. Paper or fiche 523–5243 Assistance with Federal agency subscriptions 523–5243 Documents are on file for public inspection in the Office of the Federal Register the day before they are published, unless the issuing agency requests earlier filing. -

28Th-Annual-Surgery-Research-Symposium.Pdf
Agenda 7:25 AM Welcome Room 1222 Oral Presentation 1: Top Four Abstracts - Moderators: Richard Perez, Christine Cocanour Room 1222 7:30 AM Sandra K Kabagambe: Placental Mesenchymal Stromal Cells seeded on Clinical Grade Page 9 Extracellular Matrix Improves Ambulation in Ovine Myelomeningocele 7:45 AM James Clark: Personalized Prediction of Survival for Advanced Stage Non-small Cell Page 10 Lung Cancer 8:00 AM Stacey Leventhal: De novo somatic mutation in superantigen genes of endogenous Page 11 retroviruses in the C57BL/6J inbred mice and its implication in the immune system 8:15 AM Emily M. Tibbits: Effect of Aortic Occlusion on Brain Injury Page 12 8:30 AM Faculty Presentation: Aijun Wang- Engineering Artificial Matrix for Vascular Regeneration Room 1222 Poster Session 1 - Moderators: Kiho Cho, Chandrasekar Santhanakrishnan Room 2204 9:00 AM Poster 1 - Melissa Loja: Page 13 The managed extremity score and amputation: Time for a revision 9:15 AM Poster 2 - James Becker: Page 14 Clamping Trials Prior to Thoracostomy Tube Removal and the Need for Subsequent Invasive Pleural Drainage 9:30 AM Poster 3 – Anders J. Davidson: Page 15 Incremental balloon deflation following complete REBOA results in steep inflection of flow and reperfusion in large animal model of shock 9:45 AM Poster 4 - Alicia Gingrich: Page 16 Neoadjuvant radiotherapy is independently associated with R0 resection in extremity soft tissue sarcoma: A NCDB analysis 10:00 AM Poster 5 - Erik DeSoucy: Page 17 Review of 54 Cases of Prolonged Field Care Poster Session 1 - Moderators: Michael S. Wong, Payam Saadai Room 2205 9:00 AM Poster 6 - Ivonne Palma: Page 18 Twelve Hour Ex Vivo Normothermic Perfusion (EVNP) for the Assessment of High- Risk Discarded Deceased Donor Kidneys 9:15 AM Poster 7 - Derek Asserson: Page 19 Osteogenic Differentiation of Adipose-Derived Stem Cells: A Review of the Involved Pathways 9:30 AM Poster 8 - Sarah B. -

Unspoiled Beaches Nearby. Just Because I Cannot Go There To
Locklin, Linda@Coastal Flom: Christine Fimbres <[email protected]> Sent: Wednesday, April 17, 201.9 l-2:28 PM To: Coastal Hollister Ranch Subject: Hollister For 70 years I have loved the beach since going as a child to contemplate the beauty and meaning in life--especially impactful was gazing at the horizon meeting the sea. Now I view most beaches in sorrow at the wanton trashing by my compatriots. Look anywhere, the carelessness and filth spread by so many people is undeniable, despite Susan Jordan's claim that "we all care about the environmentrr. The Coastal Commission may "have decades of experience" protecting "balance" at Big Sur precisely because it is so remote. To describe the public's activities at Joshua Tree and Elsinore is NOT demonization, -iust admission of obvious fact. Perhaps the Coastal Comm thinks those "elites" at Hollister are "no better than any other human being," but they are obviously cleaner and better stewards than the general public. I am grateful there are still some unspoiled beaches nearby. Just because I cannot go there to "enjoy" (with all the traipsing about involved), the idea that such places exist: it is reassuring and nourishing to the spirit. I Tlre Crty d{h Prolecl v.l8r.qlyf r0rrirclL:a.cr,l April 15,2019 John Ainsworth, Executive Director, California Coastal Commission Sam Schuchat, Execulive Officer, California State Coastal Conservancy Jennifer Lucchesi, Executive Officer, California State Lands Commission Lisa Mangat, Director, California Department of Parks and Recreation V ia e m a il Hol I iste r@coa sta l. -

2016 Appalachian Student Research Forum Page 1
2016 Appalachian Student Research Forum April 6 - 7, 2016 D. P. Culp Center at ETSU • Johnson City, TN _________________________ coordinated by The Office of Research and Sponsored Programs Table of Contents Schedule of Events ........................................................................................ 1 Keynote Presentation .................................................................................... 2 ASRF Task Force Members ......................................................................... 3 ASRF Judges ................................................................................................. 4 ASRF Sponsors ............................................................................................. 5 Special Thanks .............................................................................................. 6 Exhibitors ...................................................................................................... 7 Presentations Oral Master’s & Doctoral Candidates: Biomedical and Health Sciences ...... 8 Master’s Candidates: Society, Behavior and Learning ........................ 16 Master’s Candidates: Natural Sciences ................................................ 28 Doctoral Candidates: Social and Behavioral Sciences ......................... 34 Medical Residents, Clinical Fellows Medical Students and Pharmacy Students ....................................... 41 Poster Undergraduates Society, Behavior, Learning, Humanities, and Engineering......................45 Natural Sciences ........................................................................................61 -

Surgical Resident Manual 2021-2022
University of Louisville Hiram C. Polk, Jr., M.D. Department of Surgery 2021-2022 SURGICAL RESIDENT MANUAL University of Louisville Hiram C. Polk, Jr., M.D. Department of Surgery University of Louisville’s Pioneers in Surgical Education Kelly M. McMasters, M.D. Chair, 2005-Present Under Dr. McMasters’ leadership, the nationally regarded surgery residency program boasts unsurpassed depth and breadth of operative and patient experience. A renowned surgical oncologist with a robust clinical practice, McMasters is a prolific researcher who directs a basic and translational science laboratory studying adenovirus-mediated cancer gene therapy and melanoma biomarkers. McMasters initiated The Sunbelt Melanoma Trial, at the time the world’s largest melanoma study (involving more than 3,600 patients). Hiram C. Polk, Jr., M.D. Chair, 1971-2005 As chair, Dr. Polk’s leadership ushered in a period of advanced surgical research and practice in the fields of Surgical Infection, Cardiac Surgery, Hand Surgery, Microsurgery, Trauma Service and Surgical Oncology. R. Arnold Griswold, M.D. Chair, 1938-1952 Established the country’s first “Accident Service” at Louisville City Hospital. He trained and equipped police to give emergency care en route to the hospital. Griswold also developed autotransfusion and was innovative in the treatment of fractures. David Wendel Yandell, M.D. Chair, 1873-1896 A protégé of Dr. Gross and one of the South’s most prominent surgeons, he created the West’s first clinic - the “Stokes Free Dispensary.” The clinic treated indigent patients and educated students. Yandell was an early promoter of antiseptic techniques. Samuel David Gross, M.D. Chair, 1841-1856 North America’s most influential and respected surgeon in the 19th century. -

Horticulture
Macomb County 2013 ANNUAL REPORT Message from the District Coordinator In 2013, the state invested more than $54 million in MSU Extension and AgBioResearch. In the past three years, MSU Extension and AgBioResearch have been able to leverage every dollar Mission invested into $2.19 in additional funding and have generated more than $818 million for Michigan Michigan State residents, resulting in a cost/benefit ratio of 15 to 1. This means, in Macomb County, MSU University helps people Extension is able to help the health and growth of Michigan’s people and economy. improve their lives Your support of MSU Extension 4-H Youth Development allows over 4.000 Macomb youth through an educational per year learn lifelong skills, develop leadership abilities and discover the value of community process that applies service. And MSU Extension’s early childhood education programs are preparing thousands of knowledge to critical Michigan’s youngest children for scholastic success. issues, needs and When you support MSU Extension, residents learn about the safety, security and affordability opportunities. of local fresh foods, how to use them, where to find them, or how to start a cottage food business of your own. Your support of MSU Extension food safety programs allows participating individuals to use safer food handling, preparation, storage and preservation methods, which lead to a reduction in foodborne illnesses and their costs. Your support of MSU Extension nutrition and physical activity programs allowed over 5,500 Macomb County residents to improve the quality of their diets and become more active which reduces the risks of chronic conditions and moderates the increase in associated healthcare costs. -
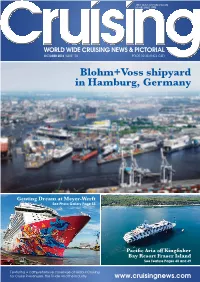
October 2016 Issue 103 Price $9.35 (Incl Gst)
19TH YEAR OF PUBLICATION ESTABLISHED 1998 OCTOBER 2016 ISSUE 103 PRICE $9.35 (INCL GST) Blohm+Voss shipyard in Hamburg, Germany Genting Dream at Meyer-Werft See Photo Gallery Page 55 Pacific Aria off Kingfisher Bay Resort Fraser Island See Feature Pages 48 and 49 Featuring a comprehensive coverage of Global Cruising for Cruise Passengers, the Trade and the Industry www.cruisingnews.com discover the magic of Australia and the South Pacific FIJI & SOUTH PACIFIC 13 TASMANIA 8 Dawn Princess®, Emerald Princess®, Sun Princess® & Golden Princess® Nights Dawn Princess® & Emerald Princess® Nights VANUATU Lautoka Sydney South Pacific Mystery Island Savusavu Ocean AUSTRALIA NEW CALEDONIA FIJI Suva Melbourne Nouméa Dravuni Overnight stay AUSTRALIA Island Indian Wineglass & Ocean Oyster Bays South Pacific Scenic cruising Ocean TASMANIA Tasman Sea Hobart Sydney Port Arthur ► Roundtrip from Sydney ► Roundtrip from Sydney 2016 Departure Dates 2017 Departure Dates 2016 Departure Dates 2017 Departure Dates Nov 6A Nov 28A Apr 21 May 7A Nov 1A Nov 20B Dec 12C Jan 2 Jan 29C Interior* Oceanview* Balcony* Mini-Suite* Interior* Oceanview* Balcony* Mini-Suite* LAUNCH FARES FROM~ $2,049 $2,649 $3,049 $3,749 LAUNCH FARES FROM~ $1,579 $1,889 $2,099 $2,419 SALE FARES FROM $1,549 $1,949 $2,499 $2,999 YOUR FARES FROM $1,399 $1,699 $1,899 Limited 3rd and 4th guest from $649 per person< 3rd and 4th guest from $499 per person< +Fares are per person twin share based on 21/04/17 sailing. Higher fares may apply to other departures. +Fares are per person twin share based on 02/01/17 sailing. -

"G" S Circle 243 Elrod Dr Goose Creek Sc 29445 $5.34
Unclaimed/Abandoned Property FullName Address City State Zip Amount "G" S CIRCLE 243 ELROD DR GOOSE CREEK SC 29445 $5.34 & D BC C/O MICHAEL A DEHLENDORF 2300 COMMONWEALTH PARK N COLUMBUS OH 43209 $94.95 & D CUMMINGS 4245 MW 1020 FOXCROFT RD GRAND ISLAND NY 14072 $19.54 & F BARNETT PO BOX 838 ANDERSON SC 29622 $44.16 & H COLEMAN PO BOX 185 PAMPLICO SC 29583 $1.77 & H FARM 827 SAVANNAH HWY CHARLESTON SC 29407 $158.85 & H HATCHER PO BOX 35 JOHNS ISLAND SC 29457 $5.25 & MCMILLAN MIDDLETON C/O MIDDLETON/MCMILLAN 227 W TRADE ST STE 2250 CHARLOTTE NC 28202 $123.69 & S COLLINS RT 8 BOX 178 SUMMERVILLE SC 29483 $59.17 & S RAST RT 1 BOX 441 99999 $9.07 127 BLUE HERON POND LP 28 ANACAPA ST STE B SANTA BARBARA CA 93101 $3.08 176 JUNKYARD 1514 STATE RD SUMMERVILLE SC 29483 $8.21 263 RECORDS INC 2680 TILLMAN ST N CHARLESTON SC 29405 $1.75 3 E COMPANY INC PO BOX 1148 GOOSE CREEK SC 29445 $91.73 A & M BROKERAGE 214 CAMPBELL RD RIDGEVILLE SC 29472 $6.59 A B ALEXANDER JR 46 LAKE FOREST DR SPARTANBURG SC 29302 $36.46 A B SOLOMON 1 POSTON RD CHARLESTON SC 29407 $43.38 A C CARSON 55 SURFSONG RD JOHNS ISLAND SC 29455 $96.12 A C CHANDLER 256 CANNON TRAIL RD LEXINGTON SC 29073 $76.19 A C DEHAY RT 1 BOX 13 99999 $0.02 A C FLOOD C/O NORMA F HANCOCK 1604 BOONE HALL DR CHARLESTON SC 29407 $85.63 A C THOMPSON PO BOX 47 NEW YORK NY 10047 $47.55 A D WARNER ACCOUNT FOR 437 GOLFSHORE 26 E RIDGEWAY DR CENTERVILLE OH 45459 $43.35 A E JOHNSON PO BOX 1234 % BECI MONCKS CORNER SC 29461 $0.43 A E KNIGHT RT 1 BOX 661 99999 $18.00 A E MARTIN 24 PHANTOM DR DAYTON OH 45431 $50.95 -

A Comparison of Continuous Renal Replacement Therapy to Intermittent Dialysis in the Management of Renal Insufficiency in the Acutely III Surgical Patient
A Comparison of Continuous Renal Replacement Therapy to Intermittent Dialysis in the Management of Renal Insufficiency in the Acutely III Surgical Patient JIMMY WALDROP, M.D.,* DAVID L. CIRAULO, D.O.,t TIMOTHY P. MILNER, M.D.,* DOUGLAS GREGORI, IV, B.S.,* AARON S. KENDRICK, D.O.,* CHARLES M. RICHART, M.D.,t ROBERT A. MAXWELL, M.D.,* DONALD E. BARKER, M.D.* From the *Department of Surgery, UT College of Medicine, Chattanooga, Tennessee; fDepartment of Surgery, Maine Medical Center, Portland, Maine; and f Saint Luke's Surgical Specialists, Saint Luke's Hospital of Kansas City, Kansas City, Missouri Acute renal failure (ARF) occurs in 10 per cent to 23 per cent of intensive care unit patients with mortality ranging from 50 per cent to 90 per cent. ARF is characterized by an acute decline in renal function as measured by urine output (UOP), serum creatinine, and blood urea nitrogen (BUN). Causes may be prerenal, intrarenal, or postrenal. Treatment consists of renal replacement therapy (RRT), either intermittent (ID) or continuous (CRRT). Indications for initiation of dialysis include oliguria, acidemia, azotemia, hyperkalemia, uremic complications, or significant edema. Overall, the literature comparing CRRT to ID is poor. No studies of only surgical/trauma patients have been published. We hypothesize that renal function and hemodynamic stability in trauma/ surgical critical care patients are better preserved by CRRT than by ID. We performed a retro- spective review of trauma/surgical critical care patients requiring renal supportive therapy. Thirty patients received CRRT and 27 patients received ID. The study was controlled for severity of illness and demographics.