TB Annual Report 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Buckinghamshire County Rugby Football Union Cup & Bowl Competitions
BUCKINGHAMSHIRE RUGBY FOOTBALL UNION LIMITED Season 2016 / 2017 H A N D B O O K bucksrfu.pitchero.com BUCKINGHAMSHIRE RUGBY FOOTBALL UNION LIMITED Registered Number: 28986 R website: bucksrfu.pitchero.com Buckinghamshire Rugby Football Union was founded on Friday, 16th July 1949 at a meeting held at the Red Lion Hotel in High Wycombe. Colours: Red & Black Chairman’s Foreword Welcome to the new County Handbook which I hope you will find to be a useful source of valuable information about our County and our Clubs. I hope that you find the fixture lists a useful feature, enabling you to support our Bucks Clubs. Please also refer to our Website: bucksrfu.pitchero.com This site holds all the relevant information and news about Bucks Rugby. Please contact the Webmaster if you have any information or news that needs to be shared. Remember, the website is only as good as its content so let’s all contribute! The season 2015/16 was again a huge success for Rugby in the County with the Bucks U 20 XV reaching the semi-final of the county plate competition and the senior XV also getting to the semi- final of their competition. This is the furthest either team have reached in the County’s history. As a County we seem to produce some very talented players, and this is very much down to the Clubs and Schools in our area being “Development” focused and ensuring that the most talented get the exposure they deserve. We intend as County to continue this theme every season and ensure that as many players as possible have the opportunity to play at their highest potential level. -

England Rugby Word Template
The Mini & Youth Rugby Blueprint Roadshow October – December 2013 Feedback Report Summary The Mini & Youth Rugby Blueprint Roadshow took place between October and December 2013. The roadshow visited 27 venues around the country and was attended by more than 500 people. The purpose of the roadshow was to give all rugby stakeholders a chance to share their views on how we shape the mini, junior and youth game in the lead up to Rugby World Cup 2015. In recent years a great deal of work has gone into considering how the game is played, delivered and organised for young people up to the age of 18. The Age Grade Competition Review has been in process for a couple of years, working on producing a recommended competition and playing framework across clubs, schools and colleges. The aim of the blueprint roadshow was to share recent evidence from players highlighting why they play and why they might have stopped playing and to research the views of stakeholders on the best way forward for the game. The challenge is to provide a game format, playing opportunities and support based on the needs and wants of young people. By getting this balance right we aim to ensure that more young people start, remain and choose a lifelong friendship with rugby union, strengthening our clubs and growing the game in the communities around them. Roadshow Format and Method At each roadshow event, the audience was given an opportunity to consider feedback from players aged 7 – 18 about why they play rugby union (and sport in general) and the reasons why they stop playing. -

An Investigation Into the Factors That Encourage Image and Performance Enhancing Drug Taking Behaviours in Adult Rugby Players in England
Stephen Watkins Brunel University London 1 An investigation into the factors that encourage Image and Performance Enhancing Drug taking behaviours in adult rugby players in England. Stephen R. Watkins A thesis submitted for the degree of Masters of Philosophy Brunel University Department of Life Sciences September 2019 COPYRIGHT Attention is drawn to the fact that copyright of this thesis rests with its author. A copy of this thesis has been supplied on condition that anyone who consults it is understood to recognise that its copyright rests with the author and they must not copy it or use material from it except as permitted by law or with the consent of the author. Stephen Watkins Brunel University London 2 ABSTRACT Pages Abstract 7 CHAPTER ONE - INTRODUCTION 9 1. Introduction 9 1.1 Introduction to IPED use in Rugby Union 9 1.2 Background to the World Anti-Doping Code 13 1.3 The need for research in Rugby Union 20 CHAPTER TWO – LITERATURE REVIEW 22 2. Review of Literature 22 2.1 Beginner or Young Person Studies 23 2.2 Gifted and Talented Studies 25 2.3 Performance Development Athlete and Performance Athlete Studies 26 2.4 Elite Athlete Level Studies – Attitudes and Prevalence of IPED use 27 2.5 Coach and Support Personnel Studies 33 2.6 Wider Society- Image & Performance Enhancing Drug Studies 38 2.7 Theoretical Concepts of Doping 40 2.7.1 The Push, Pull, Anti-Push, Anti-Pull Theory 41 2.7.2 The Gateway Use Theory of Doping 43 2.7.3 Moral Disengagement Theory 45 2.8 Literature Review Summary 50 2.8.1 Personal 51 2.8.2 Environmental 51 2.8.3 Performance 52 CHAPTER THREE - METHODOLOGY 53 3. -

Midlands Leagues Tree Season 2019-2020
MIDLANDS PREMIER (14) MIDLANDS LEAGUES TREE Bournville SEASON 2019-2020 Bridgnorth Broadstreet Bromsgrove (National Leagues first formed in 1987) Burton on Trent Doncaster Phoenix (N) Kettering Newport (Salop) Nuneaton Paviors MIDLANDS 1 WEST (14) Peterborough Lions MIDLANDS 1 EAST (14) Droitwich Sandbach (N) Derby Dudley Kingswinford Sheffield (N) Lutterworth Hereford South Leicester Market Harborough Kenilworth Melbourne Kidderminster Carolians Oadby Wyggestonian Lichfield Old Northamptonians IN OTHER DIVISIONS Ludlow (Level Transfers) Olney Newbold on Avon Bedford Athletic L5 L&SE Oundle Old Halesonians Banbury L6 SW Peterborough Stoke on Trent Luton L7 L&SE Rugby Lions Stourbridge Lions Shipston on Stour L7 SW Syston Sutton Coldfield Towcestrians Whitchurch Wellingborough Worcester West Bridgford MIDLANDS 2 WEST (N) (12) MIDLANDS 2 WEST (S) (12) MIDLANDS 2 EAST (N) (12) MIDLANDS 2 EAST (S) (12) Burntwood Barkers Butts Ashbourne Belgrave Camp Hill Earlsdon Ashfield Bugbrooke Crewe & Nantwich Evesham Coalville Leicester Forest Leek Leamington Dronfield Leighton Buzzard Longton Malvern Ilkeston Long Buckby Moseley Oak Nuneaton Old Edwardians Lincoln Market Bosworth Newcastle (Staffs) Old Laurentian Long Eaton Melton Mowbray Shrewsbury Pinley Loughborough Northampton Casuals Stafford Silhillians Market Rasen & Louth Northampton Old Scouts Tamworth Southam Matlock St Ives Walsall Spartans Newark Stewarts & Lloyds Wolverhampton Stratford upon Avon Nottingham Casuals Vipers MIDLANDS 3 WEST (N) (12) MIDLANDS 3 WEST (S) (12) MIDLANDS 3 EAST (N) (12) MIDLANDS 3 EAST (S) (12) Cleobury Mortimer Alcester Ashby Bourne Eccleshall Bedworth Bakewell Mannerians Daventry Edwardian Berkswell & Balsall Belper Dunstablians Handsworth Burbage Buxton Huntingdon & District Harborne Coventry Welsh Grimsby Northampton BBOB Linley & Kidsgrove Ledbury Kesteven Oakham Old Saltleians Manor Park Mansfield Queens Telford Hornets Old Coventrians Mellish Rushden & Higham Uttoxeter Old Leamingtonians Nottingham Moderns St. -

News of Buzzards' Hilarious Escapades and Drinking Stories
News Of Buzzards’ Hilarious Escapades And Drinking Stories Issue 19 - August 2018 [email protected] [email protected]@gmail.com Nobheads and GDPR As of 25th May new E.U. regulations came into force regarding the use and storage of personal data. The Chief Editor and all the staff at Nobheads would like to reassure all recipients that your contact details are all stored on a laptop Wright’s Meadow, Leighton Road, Stanbridge, Beds, LU7 9HR that cannot be accessed without knowledge of the requisite user password. Tel: 01525-371322 Should you wish your details to be deleted from the distribution lists your request www.buzzardrugby.co.uk will be dealt with immediately but ultimately ignored. Twitter: @buzzardrugby The views offered in this publication do not As luck would have it, the day before the legislation came into force I received an necessarily reflect official LBRFC policy. email from a very nice man called Obvious Bengewepne from Abuja in Nigeria. Photographs are often used without permission of He said he’d won the Nigerian lottery and wanted to move the money to Europe those photographed. The club logo is used without permission. There is a house in New but didn’t have an account so could I give him my bank details so he could send Orleans they call the Rising Sun. it to me. For this I would get a healthy cut of his winnings. I said that my current account is with TSB but as they have temporarily lost all of the shoe boxes in which they keep everybody’s money I wouldn’t be able to help. -

Rfu English Clubs Championship Midlands
RFU ENGLISH CLUBS CHAMPIONSHIP MIDLANDS DIVISION MIDLANDS OFFICIALS AND LEAGUE SECRETARIES 2019-2020 Midlands Division Organising Committee Paul Kaminski Chairman Green Paddocks, 21 Kingsway, Whitchurch, Shropshire. SY13 1EH North Midlands Tel: 01948 662536 (H) 01948 662889 (B) 07802 567049 (M) RFU Council Member email: [email protected] Roger Rees Secretary 2 Wain Close, Kinwarton, Alcester, Warwickshire. B49 6LA North Midlands Tel: 01789 400082 Midlands Rep RFU ACMSC email: [email protected] Henri Ginvert Treasurer 5 The Paddock, Markfield, Leicestershire. LE67 9RR Leicestershire Tel: 01530 242761 (H) 07785 724989 (M) email: [email protected] Keith Shurville East Midlands Rep 41 Churchill Avenue, Northampton. NN3 6NY Tel: 01604 494374 (H) 07721 368477 (M) email: [email protected] Steve Mounfield Leicestershire Rep 89 Curzon Avenue, Birstall, Leicestershire. LE4 4AG Tel: 0116 267 4410 (H) 07752 398507 (M) email: [email protected] Bill Worth North Midlands Rep 506 Chester Road, Kingshurst, Birmingham. B36 0LG Tel: 0121 770 5001 (H) 07926 447478 (M) email: [email protected] David Miller Notts.Lincs.& Derbys. Rep 37 Rosemary Drive, Alvaston, Derby. DE24 0TA Tel: 01332 755935 (H) 07976 193344 (M) e-mail: [email protected] Stuart Davies Staffordshire Rep Rowan Cottage, Offley Hay, Bishops Offley, Stafford. ST21 6HJ Tel: 01827 255610 (B) 07921 646705 (M) email: [email protected] Keith Brown Warwickshire Rep 20 Rosemary Way, Hinckley, Leicestershire. LE10 0LN Tel: 01455 446058 (H) 07852 746570 (M) email: [email protected] 25/10/19 RWR RFU ENGLISH CLUBS CHAMPIONSHIP Ex-Officio Members Bob Taylor Deputy Chairman 82 Bridgewater Drive, Northampton. NN3 3AG Past President RFU Tel: 01604 638626 (H) 07775 800391 (M) East Midlands email: [email protected] Midlands Leagues Secretaries Phil Green Midlands Premier 28 Longdon Croft, Copt Heath, Knowle, West Midlands. -
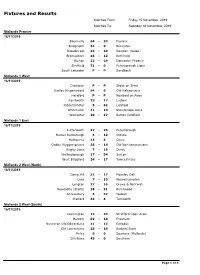
Fixtures and Results
Fixtures and Results Matches From: Friday 15 November, 2019 Matches To: Saturday 16 November, 2019 Midlands Premier 16/11/2019 Bournville 64 - 29 Paviors Bridgnorth 34 - 0 Nuneaton Broadstreet 33 - 40 Newport (Salop) Bromsgrove 48 - 12 Kettering Burton 22 - 29 Doncaster Phoenix Sheffield 71 - 0 Peterborough Lions South Leicester P - P Sandbach Midlands 1 West 16/11/2019 Droitwich P - P Stoke on Trent Dudley Kingswinford 54 - 0 Old Halesonians Hereford P - P Newbold on Avon Kenilworth 25 - 17 Ludlow Kidderminster 5 - 62 Lichfield Whitchurch 41 - 10 Stourbridge Lions Worcester 20 - 17 Sutton Coldfield Midlands 1 East 16/11/2019 Lutterworth 27 - 26 Peterborough Market Harborough 6 - 12 Oundle Melbourne 13 - 3 Olney Oadby Wyggestonians 26 - 14 Old Northamptonians Rugby Lions 7 - 19 Derby Wellingborough 17 - 54 Syston West Bridgford 24 - 17 Towcestrians Midlands 2 West (North) 16/11/2019 Camp Hill 31 - 17 Moseley Oak Leek 7 - 10 Wolverhampton Longton 27 - 16 Crewe & Nantwich Newcastle (Staffs) 18 - 21 Burntwood Shrewsbury 3 - 32 Walsall Stafford 32 - 6 Tamworth Midlands 2 West (South) 16/11/2019 Leamington 12 - 24 Stratford Upon Avon Malvern 82 - 18 Evesham Nuneaton Old Edwardians 41 - 12 Earlsdon Old Laurentians 28 - 19 Barkers Butts Pinley 0 - 0 Spartans (Midlands) Silhillians 45 - 0 Southam Page 1 of 4 Fixtures and Results Matches From: Friday 15 November, 2019 Matches To: Saturday 16 November, 2019 Midlands 2 East (North) 16/11/2019 Ashbourne 3 - 19 Long Eaton Dronfield 49 - 7 Nottingham Casuals Ilkeston 11 - 8 Coalville Lincoln P - P Ashfield -

Club History
Club History Inception: the 1950s and 1960s In 1956 a group of 15-year-old school leavers from Players School and Cottesmore School had nowhere to play so they formed their own club. Nottingham Moderns RFC was formed. The early matches were played on rented pitches around the city. With the help of old school masters and the youth service, steady progress was made. However, financing the new club was a problem. On most occasions the players would make their way to away matches by public transport, resulting in all day adventures to various parts of the East Midlands. A good relationship was formed with the local colleges and sports teachers, and with the Welsh Exiles. This led to a period of rapid growth that resulted in sustained fixtures with more established local sides and also games against the 2nd XV teams from the Midlands senior teams.[3] Settling down: The 1970s The year 1975 was momentous in the history of the club. The club finally secured a home at Wilford where they remain today. In the same year they became the first club from Nottinghamshire to win the Three Counties Cup (Nottinghamshire, Derbyshire & Lincolnshire). The 1st XV also reached the semi-final of the Midlands Clubs Championship. The most successful season in the club's history was probably 1974–75, with the 1st XV, 2nd XV, and 3rd XV losing just three games each all season.The 1st XV and 2nd XV also won the respective County Cup competitions. All of this was accomplished as a nomadic club, with no fixed home, playing on rented parks pitches, and drinking in numerous local public houses to entertain their opposition. -

North East England
North East England Extrait du AS Lagny Rugby http://www.aslagnyrugby.net/North-East-England.html North East England - Liens - Date de mise en ligne : dimanche 7 décembre 2014 Copyright © AS Lagny Rugby - Tous droits réservés Copyright © AS Lagny Rugby Page 1/10 North East England Cette page regroupe les clubs du Nord-Est de l'Angleterre (North East England) représentés par leurs couleurs (logo ou écusson si nous l'avons trouvé) et le lien vers leur site internet ou le blog qui leur est consacré. Ils sont regroupés selon les 4 comtés de cette région : Northumberland, Tyne and Wear, Durham et North Yorkshire (en partie). N'hésitez pas à nous contacter si vous constatez une erreur, un oubli, où si vous possédez le logo manquant d'un club, son adresse internet. Northumberland (Alnwick)Alnwick RFC [Alnwick Rugby Football Club] Copyright © AS Lagny Rugby Page 2/10 North East England (Ashington)Ashington JW RFC [Ashington Joint Welfare Rugby Football Club] (Berwick-upon-Tweed)Berwick RFC [Berwick Rugby Football Club] (Blyth)Blyth RFC [Blyth Rugby Football Club] (Corbridge)Tynedale RFC [Tynedale Rugby Football Club] (Kielder)Border Park RFC [Border Park Rugby Football Club] (Morpeth)Morpeth RFC [Morpeth Rugby Football Club] (Ponteland)Ponteland RFC [Ponteland Rugby Football Club] (Seghill)Seghill RFC [Seghill Rugby Football Club] (Stocksfield)Prudhoe & Stocksfield RUFC [Prudhoe & Stocksfield Rugby Union Football Club] Tyne and Wear (Gateshead)Gateshead RFC [Gateshead Rugby Football Club] Copyright © AS Lagny Rugby Page 3/10 North East England -

NEWARK RUGBY UNION FOOTBALL CLUB the First Seventy Five Years
NEWARK RUGBY UNION FOOTBALL CLUB The First Seventy Five Years A.J.COLEMAN Foreword. The first mention of Rugby in the Newark area is a paragraph in a book, Football the Rugby Union Game, published in 1891. This states that the Hull Club, formed in 1865, played a type of Rugby and amongst its opponents were Newark, whom they played four times a year. A search through the Newark Advertisers and Heralds of that time and an investigation by the R.F.U. cannot offer any information, but one possibility is that there may have been a Military Unit stationed in the area who played this handling game. Dr. Ernest Ringrose, a Rugby fanatic arrived at Newark in the 1880's. The "little" doctor as he was affectionately known, a talented player with Old Merchant Taylors Club soon tried to enthuse the people of Newark into the game of Rugby Football. On December 19th 1891, a challenge match took place on the Sconce Hills between a team from Newark and a team from Nottingham. The Newark team was composed from the people of Newark to "this side of Bingham". This match is assumed to be the first to be played in Newark although a press caption of several issues prior to the event states "that Newarkers do not often enjoy the chance of seeing Rugby Football" giving further claim that there had been a Military Unit playing a type of Rugby Football. The match details which were reported in both the local Newspapers (although they could not agree on the score) and allowing a little poetic licence went as follows: "Newark Rugby lads are a hardy lot for this game they played alongside a group of iceskaters. -
01A WRFU Handbook 2019-20 ADVERTS FRONT
Warwickshire Rugby Football Union & Warwickshire Society of Referees HANDBOOK SEASON 2019 - 2020 WARWICKSHIRE RUGBY FOOTBALL UNION Warwickshire Rugby Football Union Age Grade Rugby - Top Ten Tips 1. Review workforce list, ensure RFU DBS checks in place 2. Ensure workforce appropriately trained for their role 3. Ensure that a Safeguarding Offi cer is on duty during mini and junior training and match days 4. Report and record safeguarding incidents on the day 5. Ensure that a Rugby First Aider is on duty during mini and junior training and match days 6. Record and report accidents / injuries on the day 7. Obtain permissions / dispensations / undertake audit for players playing out of age grade 8. Festivals with CB permission with a written risk assessment in place 9. Tours with CB permission with a written risk assessment and tour code of conduct in place 10. Work within Regulations 9, 15 and 21, if not Regulation 19 applies! 2019 / 2020 Season WARWICKSHIRE RFU SENIOR MEN’S XV Bill Beaumont County Championship Level 2 Finalists, Twickenham, 27th May 2018 Season 2020 Be part of the County’s Senior XV this season TRAINING Every Tuesday and Thursday from start of April until the last championship match. CHAMPIONSHIP MATCHES - Dates TBC MAIN CONTACTS Senior Chairman Steve Wilkes 07526 523 323 Administrator Paul Harrison 07765 224 624 Team Manager Tim Douglas 07437 407 966 Information will be sent out to clubs during the season. This season it could be you playing at Twickenham! SECTION 1 Warwickshire Rugby Football Union Season 2019-2020 Contents 2. Offi cers and General Committee 5. -

Bishop's Stortford Rfc V Caldy
BSRFC OFFICIAL MATCH PROGRAMME THIS WEEKS FEATURES: NEW SEASON NEW CAPTAIN THE ROAD TO NATIONAL 1 THE NEW LAWS FOR THIS SEASON NATIONAL LEAGUE 1 BISHOP’S STORTFORD RFC V CALDY RFC £12 2 September 2017 Members £5 This beautiful programme has been produced using the very latest printing gizmos! It’s produced weekly... Designed Friday morning, Printed and finished Friday afternoon and in your good hands by Saturday lunchtime! Impressed? Give us a call to find out more 01279 757333 | proco.com - 2 - PRESIDENT’S WELCOME PERRY OLIVER WELCOME BACK TO SILVER LEYS FOR THE FIRST GAME OF THE 2017/18 SEASON AND OF COURSE OUR FIRST IN NATIONAL LEAGUE ONE. THE SUMMER, IF IT DESERVES TO BE CALLED THAT, SEEMS TO HAVE FLOWN BY BUT AT LEAST THE UNSEASONAL WEATHER HAS HELPED TUBBY WORK HIS MAGIC AND RESTORE ALL OF OUR PITCHES TO A1 CONDITION. I’d also like to extend a special welcome to the Thank you to everyone who helped us raise Players, Officials and Supporters of Caldy RFC the magnificent amount of £8374.43 for last on this first time our clubs would have met, and season’s Presidents Charity ‘Ellies Fund’. of course everyone associated with our Match This season we have decided to make The Day sponsors –Tees & Match Day Experience Essex & Herts Air Ambulance our club charity. sponsors - Russell Partnership. On the final weekend of last season as we Like ourselves, Caldy are new to National One. were all celebrating promotion and the Blues Like us they were promoted as Champions of winning the County cup, we learnt that one their National 2 league – the North, failing to of our youth players had sustained a serious win only 3 of their 30 games.