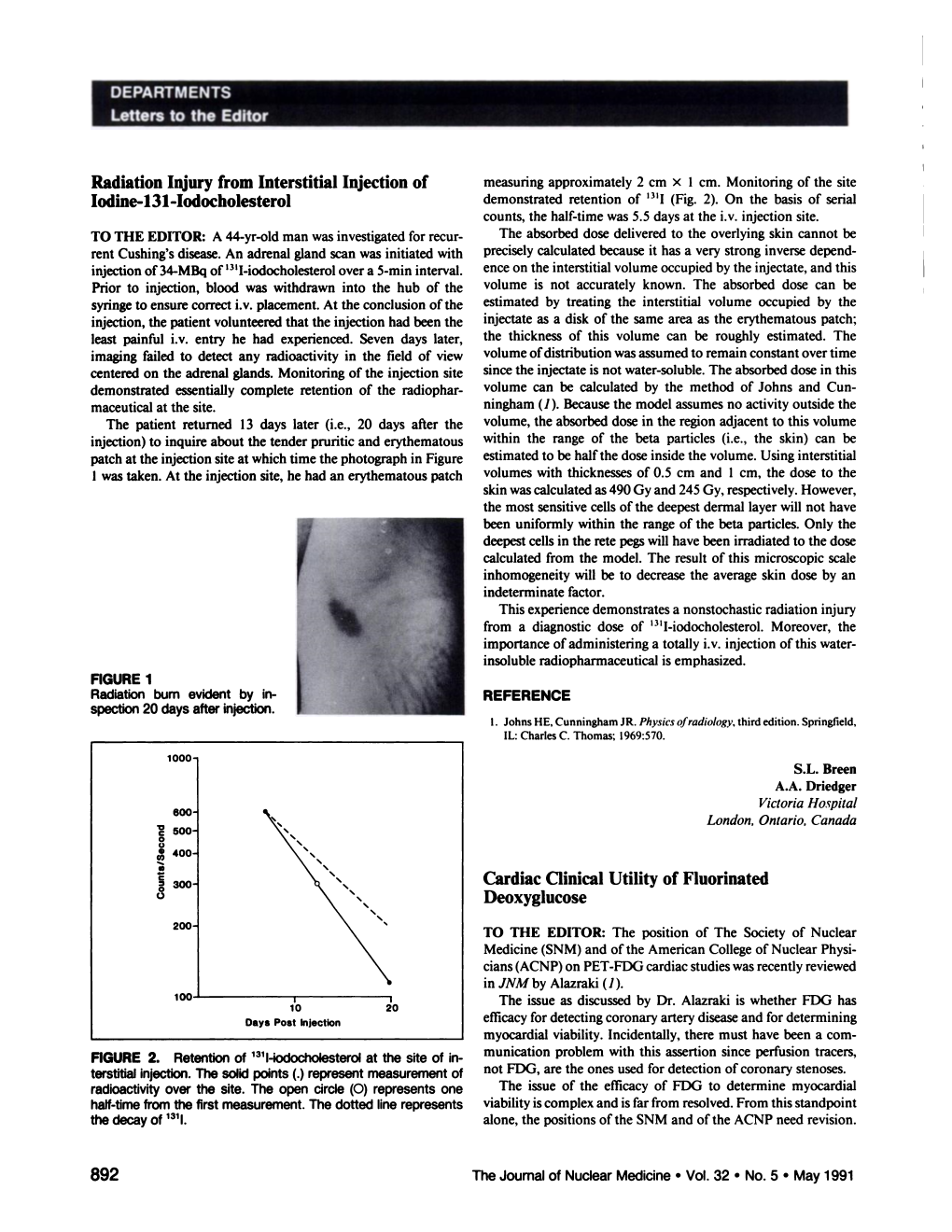
Lettirs to Th Editor Radiation Injury from Interstitial Injection Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PET Imaging of Occult Tumours by Temporal Integration of Tumour-Acidosis Signals from Ph-Sensitive 64Cu-Labelled Polymers
ARTICLES https://doi.org/10.1038/s41551-019-0416-1 PET imaging of occult tumours by temporal integration of tumour-acidosis signals from pH-sensitive 64Cu-labelled polymers Gang Huang 1, Tian Zhao1, Chensu Wang 1, Kien Nham2, Yahong Xiong2, Xiaofei Gao3, Yihui Wang3, Guiyang Hao 2, Woo-Ping Ge3, Xiankai Sun2, Baran D. Sumer 4* and Jinming Gao 1,4* Owing to the diversity of cancer types and the spatiotemporal heterogeneity of tumour signals, high-resolution imaging of occult malignancy is challenging. 18F-fluorodeoxyglucose positron emission tomography allows for near-universal cancer detec- tion, yet in many clinical scenarios it is hampered by false positives. Here, we report a method for the amplification of imaging contrast in tumours via the temporal integration of the imaging signals triggered by tumour acidosis. This method exploits the catastrophic disassembly, at the acidic pH of the tumour milieu, of pH-sensitive positron-emitting neutral copolymer micelles into polycationic polymers, which are then internalized and retained by the cancer cells. Positron emission tomography imaging of the 64Cu-labelled polymers detected small occult tumours (10–20 mm3) in the brain, head, neck and breast of mice at much higher contrast than 18F-fluorodeoxyglucose, 11C-methionine and pH-insensitive 64Cu-labelled nanoparticles. We also show that the pH-sensitive probes reduce false positive detection rates in a mouse model of non-cancerous lipopolysaccharide-induced inflammation. This macromolecular strategy for integrating tumour acidosis should enable improved cancer detection, surveil- lance and staging. ancer exhibits diverse genetic and histological differences tumours over the surrounding normal tissues often leads to false from normal tissues1. -

Nuclear Medicine for Medical Students and Junior Doctors
NUCLEAR MEDICINE FOR MEDICAL STUDENTS AND JUNIOR DOCTORS Dr JOHN W FRANK M.Sc, FRCP, FRCR, FBIR PAST PRESIDENT, BRITISH NUCLEAR MEDICINE SOCIETY DEPARTMENT OF NUCLEAR MEDICINE, 1ST MEDICAL FACULTY, CHARLES UNIVERSITY, PRAGUE 2009 [1] ACKNOWLEDGEMENTS I would very much like to thank Prof Martin Šámal, Head of Department, for proposing this project, and the following colleagues for generously providing images and illustrations. Dr Sally Barrington, Dept of Nuclear Medicine, St Thomas’s Hospital, London Professor Otakar Bělohlávek, PET Centre, Na Homolce Hospital, Prague Dr Gary Cook, Dept of Nuclear Medicine, Royal Marsden Hospital, London Professor Greg Daniel, formerly at Dept of Veterinary Medicine, University of Tennessee, currently at Virginia Polytechnic Institute and State University (Virginia Tech), Past President, American College of Veterinary Radiology Dr Andrew Hilson, Dept of Nuclear Medicine, Royal Free Hospital, London, Past President, British Nuclear Medicine Society Dr Iva Kantorová, PET Centre, Na Homolce Hospital, Prague Dr Paul Kemp, Dept of Nuclear Medicine, Southampton University Hospital Dr Jozef Kubinyi, Institute of Nuclear Medicine, 1st Medical Faculty, Charles University Dr Tom Nunan, Dept of Nuclear Medicine, St Thomas’s Hospital, London Dr Kathelijne Peremans, Dept of Veterinary Medicine, University of Ghent Dr Teresa Szyszko, Dept of Nuclear Medicine, St Thomas’s Hospital, London Ms Wendy Wallis, Dept of Nuclear Medicine, Charing Cross Hospital, London Copyright notice The complete text and illustrations are copyright to the author, and this will be strictly enforced. Students, both undergraduate and postgraduate, may print one copy only for personal use. Any quotations from the text must be fully acknowledged. It is forbidden to incorporate any of the illustrations or diagrams into any other work, whether printed, electronic or for oral presentation. -

A Technique for Standardized Central Analysis of 6-18F-Fluoro-L-DOPA PET Data from a Multicenter Study
A Technique for Standardized Central Analysis of 6-18F-Fluoro-L-DOPA PET Data from a Multicenter Study Alan L. Whone, MRCP1; Dale L. Bailey, PhD2; Philippe Remy, PhD3; Nicola Pavese, MD1; and David J. Brooks, DSc1 1Division of Neuroscience and MRC Clinical Sciences Centre, Faculty of Medicine, Imperial College, Hammersmith Hospital, London, United Kingdom; 2Department of Nuclear Medicine, Royal North Shore Hospital, Sydney, Australia; and 3CEA-Centre National de la Recherche Scientifique Unite´ de Recherche Associe´e 2210, Service Hospitalier Frederic Joliot, Orsay, France tralized analysis offers the potential for improved detection of We have recently completed a large 6-18F-fluoro-L-DOPA (18F- outcomes due to the standardization of the analytic approach DOPA) PET study comparing rates of loss of dopamine terminal and allows the analysis of large numbers of PET studies. function in Parkinson’s disease (PD) patients taking either the Key Words: PET; 18F-DOPA; Parkinson’s disease; progression; dopamine agonist ropinirole or L-DOPA. This trial involved a central analysis “distributed acquisition/centralized analysis” method, in which J Nucl Med 2004; 45:1135–1145 18F-DOPA images were acquired at 6 different PET centers around the world and then analyzed at a single site. To our knowledge, this is the first time such a centralized approach has been employed with 18F-DOPA PET and this descriptive basic science article outlines the methods used. Methods: One hun- With rapid advances in molecular medicine, the pro- dred eighty-six PD patients were randomized (1:1) to ropinirole duction of neuroprotective or neurorestorative agents that or L-DOPA therapy, and 18F-DOPA PET was performed at base- affect the progression of degenerative conditions such as line and again at 2 y. -
![[123I]FP-CIT SPECT in Atypical Degenerative Parkinsonism](https://docslib.b-cdn.net/cover/2351/123i-fp-cit-spect-in-atypical-degenerative-parkinsonism-242351.webp)
[123I]FP-CIT SPECT in Atypical Degenerative Parkinsonism
CONTRAST AGENT EVALUATION [123I]FP-CIT SPECT in atypical degenerative parkinsonism One of the most widely used techniques to support the clinical diagnosis of Parkinson’s disease is the SPECT scan with [123I]FP-CIT. This tracer binds reversibly and visualizes the striatal presynaptic dopamine transporters. Several uncertainties remain on the value of [123I]FP-CIT and SPECT in atypical degenerative parkinsonian syndromes. In this concise review, we discuss the contribution of SPECT and [123I]FP-CIT in supporting the clinical diagnosis of Parkinson’s disease and their role in the differential diagnosis of Parkinson’s disease and atypical degenerative parkinsonism. The chemistry, pharmacodynamics and pharmacokinetics of [123I]FP-CIT are also discussed. 1,2,3 KEywordS: atypical degenerative parkinsonism n FP-CIT n ioflupane n SPECT Ioannis U Isaias* , Giorgio Marotta4, Gianni Pezzoli2, Parkinson’s disease (PD) is the second most dystonic tremor [15] and psychogenic parkin- Osama Sabri5 [1] [16,17] 5,6 common neurodegenerative disorder , yet sonism . In this concise review, we will & Swen Hesse 123 early accurate diagnosis remains challenging. discuss the role of SPECT and [ I]FP-CIT in 1Università degli Studi di Milano, The estimated prevalence of PD is 0.5–1% in supporting the clinical diagnosis of PD and its Dipartimento di Fisiologia Umana, those aged 65–69 years and 1–3% in those aged differential diagnosis with ADP. Milano, Italy 2Centro per la Malattia di Parkinson e i ≥80 years [1]. Although the clinical diagnosis of Disturbi del Movimento, -

DICOM Conformance Template
g GE Heathcare Technical Publications Direction 5507068-1EN (DOC1584283) Revision 1 DaTQUANT Application™ DICOM CONFORMANCE STATEMENT Copyright 2015 by General Electric Co. Do not duplicate g GE Heathcare LIST OF REVISIONS REV DATE DESCRIPTION PAGES APPR. 1 May 2015 Initial Release All M. Mesh DATQUANT APPLICATION GE Healthcare DICOM CONFORMANCE STATEMENT DIR 5507068-1EN (DOC1584283) REV 1 THIS PAGE LEFT INTENTIONALLY BLANK DATQUANT APPLICATION GE Healthcare DICOM CONFORMANCE STATEMENT DIR 5507068-1EN (DOC1584283) REV 1 CONFORMANCE STATEMENT OVERVIEW DaTQUANT application is an application that uses NM and CT images and creates NM, SC and MFSC images. Table 0.1 provides an overview of the network services supported by the DaTQUANT application. Table 0.1 – APPLICATION SOP Classes User of Object Creator of Instances Object Instances Transfer Secondary Capture Image Storage No Yes Multi-frame True Color Secondary Capture Image Storage No Yes Nuclear Medicine Image Storage Yes Yes Computerized Tomography Image Storage Yes No 4 DATQUANT APPLICATION GE Healthcare DICOM CONFORMANCE STATEMENT DIR 5507068-1EN (DOC1584283) REV 1 1. INTRODUCTION ............................................................................................................... 8 1.1 Overview ..................................................................................................................................................................... 8 1.2 Overall DICOM Conformance Statement Document Structure .......................................................................... -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Auger Electrons for Cancer Therapy – a Review Anthony Ku1†, Valerie J
Ku et al. EJNMMI Radiopharmacy and Chemistry (2019) 4:27 EJNMMI Radiopharmacy https://doi.org/10.1186/s41181-019-0075-2 and Chemistry REVIEW Open Access Auger electrons for cancer therapy – a review Anthony Ku1†, Valerie J. Facca1†, Zhongli Cai1 and Raymond M. Reilly1,2,3,4* * Correspondence: raymond.reilly@ utoronto.ca Abstract †Anthony Ku and Valerie J. Facca contributed equally to this work. Background: Auger electrons (AEs) are very low energy electrons that are emitted 111 67 99m 195m 125 1Department of Pharmaceutical by radionuclides that decay by electron capture (e.g. In, Ga, Tc, Pt, I Sciences, University of Toronto, and 123I). This energy is deposited over nanometre-micrometre distances, resulting in Toronto, ON, Canada 2Department of Medical Imaging, high linear energy transfer (LET) that is potent for causing lethal damage in cancer University of Toronto, Toronto, ON, cells. Thus, AE-emitting radiotherapeutic agents have great potential for treatment of Canada cancer. In this review, we describe the radiobiological properties of AEs, their Full list of author information is available at the end of the article radiation dosimetry, radiolabelling methods, and preclinical and clinical studies that have been performed to investigate AEs for cancer treatment. Results: AEs are most lethal to cancer cells when emitted near the cell nucleus and especially when incorporated into DNA (e.g. 125I-IUdR). AEs cause DNA damage both directly and indirectly via water radiolysis. AEs can also kill targeted cancer cells by damaging the cell membrane, and kill non-targeted cells through a cross-dose or bystander effect. The radiation dosimetry of AEs considers both organ doses and cellular doses. -
Brain Imaging
Publications · Brochures Brain Imaging A Technologist’s Guide Produced with the kind Support of Editors Fragoso Costa, Pedro (Oldenburg) Santos, Andrea (Lisbon) Vidovič, Borut (Munich) Contributors Arbizu Lostao, Javier Pagani, Marco Barthel, Henryk Payoux, Pierre Boehm, Torsten Pepe, Giovanna Calapaquí-Terán, Adriana Peștean, Claudiu Delgado-Bolton, Roberto Sabri, Osama Garibotto, Valentina Sočan, Aljaž Grmek, Marko Sousa, Eva Hackett, Elizabeth Testanera, Giorgio Hoffmann, Karl Titus Tiepolt, Solveig Law, Ian van de Giessen, Elsmarieke Lucena, Filipa Vaz, Tânia Morbelli, Silvia Werner, Peter Contents Foreword 4 Introduction 5 Andrea Santos, Pedro Fragoso Costa Chapter 1 Anatomy, Physiology and Pathology 6 Elsmarieke van de Giessen, Silvia Morbelli and Pierre Payoux Chapter 2 Tracers for Brain Imaging 12 Aljaz Socan Chapter 3 SPECT and SPECT/CT in Oncological Brain Imaging (*) 26 Elizabeth C. Hackett Chapter 4 Imaging in Oncological Brain Diseases: PET/CT 33 EANM Giorgio Testanera and Giovanna Pepe Chapter 5 Imaging in Neurological and Vascular Brain Diseases (SPECT and SPECT/CT) 54 Filipa Lucena, Eva Sousa and Tânia F. Vaz Chapter 6 Imaging in Neurological and Vascular Brain Diseases (PET/CT) 72 Ian Law, Valentina Garibotto and Marco Pagani Chapter 7 PET/CT in Radiotherapy Planning of Brain Tumours 92 Roberto Delgado-Bolton, Adriana K. Calapaquí-Terán and Javier Arbizu Chapter 8 PET/MRI for Brain Imaging 100 Peter Werner, Torsten Boehm, Solveig Tiepolt, Henryk Barthel, Karl T. Hoffmann and Osama Sabri Chapter 9 Brain Death 110 Marko Grmek Chapter 10 Health Care in Patients with Neurological Disorders 116 Claudiu Peștean Imprint 126 n accordance with the Austrian Eco-Label for printed matters. -

Nuclear Pharmacy Quick Sample
12614-01_CH01-rev3.qxd 10/25/11 10:56 AM Page 1 CHAPTER 1 Radioisotopes Distribution for Not 1 12614-01_CH01-rev3.qxd 10/25/1110:56AMPage2 2 N TABLE 1-1 Radiopharmaceuticals Used in Nuclear Medicine UCLEAR Chemical Form and Typical Dosage P Distribution a b HARMACY Radionuclide Dosage Form Use (Adult ) Route Carbon C 11 Carbon monoxide Cardiac: Blood volume measurement 60–100 mCi Inhalation Carbon C 11 Flumazenil injection Brain: Benzodiazepine receptor imaging 20–30 mCi IV Q UICK Carbon C 11 Methionine injection Neoplastic disease evaluation in brain 10–20 mCi IV R Carbon C 11 forRaclopride injection Brain: Dopamine D2 receptor imaging 10–15 mCi IV EFERENCE Carbon C 11 Sodium acetate injection Cardiac: Marker of oxidative metabolism 12–40 mCi IV Carbon C 14 Urea Diagnosis of Helicobacter pylori infection 1 µCi PO Chromium Cr 51 Sodium chromate injection Labeling red blood cells (RBCs) for mea- 10–80 µCi IV suring RBC volume, survival, and splenic sequestration Cobalt Co 57 Cyanocobalamin capsules Diagnosis of pernicious anemia and 0.5 µCi PO Not defects of intestinal absorption Fluorine F 18 Fludeoxyglucose injection Glucose utilization in brain, cardiac, and 10–15 mCi IV neoplastic disease Fluorine F 18 Fluorodopa injection Dopamine neuronal decarboxylase activity 4–6 mCi IV in brain Fluorine F 18 Sodium fluoride injection Bone imaging 10 mCi IV Gallium Ga 67 Gallium citrate injection Hodgkin’s disease, lymphoma 8–10 mCi IV Acute inflammatory lesions 5 mCi IV Indium In 111 Capromab pendetide Metastatic imaging in patients with biopsy- -

Pharmaceuticals Appendix
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ADAPALENE 106685-40-9 ABANOQUIL 90402-40-7 ADAPROLOL 101479-70-3 ABECARNIL 111841-85-1 ADEMETIONINE 17176-17-9 ABLUKAST 96566-25-5 ADENOSINE PHOSPHATE 61-19-8 ABUNIDAZOLE 91017-58-2 ADIBENDAN 100510-33-6 ACADESINE 2627-69-2 ADICILLIN 525-94-0 ACAMPROSATE 77337-76-9 ADIMOLOL 78459-19-5 ACAPRAZINE 55485-20-6 ADINAZOLAM 37115-32-5 ACARBOSE 56180-94-0 ADIPHENINE 64-95-9 ACEBROCHOL 514-50-1 ADIPIODONE 606-17-7 ACEBURIC ACID 26976-72-7 ADITEREN 56066-19-4 ACEBUTOLOL 37517-30-9 ADITOPRIME 56066-63-8 ACECAINIDE 32795-44-1 ADOSOPINE 88124-26-9 ACECARBROMAL 77-66-7 ADOZELESIN 110314-48-2 ACECLIDINE 827-61-2 ADRAFINIL 63547-13-7 ACECLOFENAC 89796-99-6 ADRENALONE 99-45-6 ACEDAPSONE 77-46-3 AFALANINE 2901-75-9 ACEDIASULFONE SODIUM 127-60-6 AFLOQUALONE 56287-74-2 ACEDOBEN 556-08-1 AFUROLOL 65776-67-2 ACEFLURANOL 80595-73-9 AGANODINE 86696-87-9 ACEFURTIAMINE 10072-48-7 AKLOMIDE 3011-89-0 ACEFYLLINE CLOFIBROL 70788-27-1 -

Adrenal Gland Scintigraphy
Adrenal Gland Scintigraphy Anca M. Avram, MD,* Lorraine M. Fig, MBChB, MPH,*,† and Milton D. Gross, MD*,† There is no question that high-resolution imaging techniques have revolutionized the approach to diagnostic imaging. Computed tomography (CT) and magnetic resonance imaging provide exquisite images of the adrenal glands and offer the best initial imaging approach in the evaluation of patients with suspected adrenal disease. However, an assessment of anatomy is only a portion of the diagnostic effort, which begins with a biochemical evaluation to establish the presence of adrenal gland dysfunction. With a confirmed biochemical diagnosis in hand, a logical and stepwise diagnostic approach can be tailored to a particular patient. Where scintigraphy fits in the evaluation of diseases of the adrenal cortex and medulla in the context of high-resolution imaging and which radiopharmaceuticals should be deployed has changed substantially during the last 2 decades. Adrenal functional imaging has evolved from classic planar scintigraphy to single-photon emission computed tomography (SPECT) and positron emission tomography (PET) using tracers that, by targeting specific metabolic or synthetic processes within the gland, have depicted adrenal pathophysiology. New PET/CT and SPECT/CT technologies integrate anatomic and functional information and redefine the radiotracer principle in the larger context of high resolution anatomic imaging. Semin Nucl Med 36:212-227 © 2006 Elsevier Inc. All rights reserved. drenal gland scintigraphy uses radiopharmaceuticals -

The Use of Stems in the Selection of International Nonproprietary Names (INN) for Pharmaceutical Substances
WHO/PSM/QSM/2006.3 The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances 2006 Programme on International Nonproprietary Names (INN) Quality Assurance and Safety: Medicines Medicines Policy and Standards The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.