Append Ndectomy TERI JUNGE, CST/CFA CASE STUDY
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SURGICAL INSTRUMENTS Veterinarians Are the Doctors Specializing in the Health of Animals
SURGICAL INSTRUMENTS Veterinarians are the doctors specializing in the health of animals. They do the necessary surgical operations and care for the well-being of the animal creatures. The very basic thing they need in a certain operation and care are the veterinary instruments. This will serve as the main allay of every veterinarian in providing care. (1) What are surgical instruments? Surgical instruments are essentially gadgets planned in an uncommon manner to perform particular capacities amid a surgical operation to improve viability and accomplishment of the surgery. (1) 4 Basic types of surgical instruments Surgical instruments are specially designed tools that assist health care professionals car- ry out specific actions during an operation. Most instruments crafted from the early 19th century on are made from durable stainless steel. Some are designed for general use, and others for spe- cific procedures. There are many surgical instruments available for almost any specialization in medicine. There are precision instruments used in microsurgery, ophthalmology and otology. Most surgical instruments can be classified into these 4 basic types: Cutting and Dissecting – these instruments usually have sharp edges or tips to cut through skin, tissue and suture material. Surgeons need to cut and dissect tissue to explore irregular growths and to remove dangerous or damaged tissue. These instruments have single or double razor- sharp edges or blades. Nurses need to be very careful to avoid injuries, and regularly inspect these instruments before using, for re-sharpening or replacement. 11 Iris Scissors 2016 – 1 – LV01-KA202 – 022652 This project is funded by the European Union Clamping and Occluding – are used in many surgical procedures for compressing blood vessels or hollow organs, to prevent their contents from leaking. -

The Introductory Guide/Basic Course #1 Chapter I About Sklar for 123 Years, Sklar Has Set the Standard for Surgical Instrumentation
Surgical Instruments: The Introductory Guide/Basic Course #1 Chapter I About Sklar For 123 years, Sklar has set the standard for surgical instrumentation. In 1892, German born instrument maker John Sklar, founded the company to fill a need for American made surgical instruments and the rest is history. Sklar rose to prominence during World Wars I and II and was awarded the principal contract as the surgical instrument provider for the United States military. This contract established Sklar as the industry leader and placed it on the forefront of the surgical marketplace, where it went on to receive Certificates of Merit and Achievement from the U.S. Navy and six Army Navy “E” Production Awards. During the 1930s, Sklar’s research department helped to develop a stainless steel alloy especially suited to the manufacture of surgical instruments. The company’s investment in research was justified long-term; most surgical instruments are still made of long-lasting, rust resistant, stainless steel. Today, Sklar is headquartered in West Chester, Pennsylvania where it remains the authority on the manufacture of high quality surgical instruments to medical professionals in 75 countries worldwide. Throughout its history, Sklar has collaborated with leading surgeons and medical facilities to develop thousands of unique surgical instrument patterns. In recent years, Sklar has expanded its product line to include more than 19,000 precision crafted, stainless steel instruments: the largest offering of surgical instruments in the world. Specialty practices include: OB/GYN, Orthopedic, ENT, Cardiovascular, Endoscopic, Dermatology, Podiatry, Veterinary, Dental, etc. The prevention and reduction of healthcare associated infection (HAI) is a top priority in medical facilities today. -

The Basic Surgery Kit
GLOBAL EXCLUSIVE > SURGERY > PEER REVIEWED The Basic Surgery Kit Jan Janovec, MVDr, MRCVS VRCC Veterinary Referrals Laurent Findji, DMV, MS, MRCVS, DECVS Fitzpatrick Referrals Considering the virtually limitless range of surgical instruments, it can be difficult to assemble a cost-effective basic surgery kit. Some instruments may misleadingly appear multipurpose, but their misuse may damage them, leading to unnecessary replacement costs or, worse, intraoperative accidents putting the patient’s safety at risk. Many instru- ments are available in different qualities and materials (eg, tungsten carbide instruments— more expensive but much more resistant to wear and corrosion than stainless steel) and Minimal Basic Surgery Kit varied sizes to match the purpose of their use as well as the size of the surgeon’s hand. n 1 instrument case Cutting Instruments n 1 scalpel handle Scalpel n 1 pair Mayo scissors The scalpel is an indispensible item in a surgical kit designed to make sharp incisions. Scalpel incision is the least traumatic way of dissection, but provides no hemostasis. n 1 pair Metzenbaum scissors Scalpel handles come in various sizes, each accommodating a range of disposable n 1 pair suture scissors blades (Figure 1). Entirely disposable scalpels are also available. n 1 pair Mayo-Hegar needle holder Scissors n 1 pair Brown-Adson tissue forceps Scissors are used for cutting, albeit with some crushing effect, and for blunt dissection. n 1 pair DeBakey tissue forceps Fine scissors, such as Metzenbaum scissors (Figure 2), should be reserved for cutting n 4 pairs mosquito hemostatic forceps and dissecting delicate tissues. Sturdier scissors, such as Mayo or suture scissors, are designed for use on denser tissues (eg, fascia) or inanimate objects (eg, sutures, drapes). -

Handling of Instruments
Limbs & Things TM learning online Handling of Instruments Overview If you are new to suturing, you will need to learn to recognize each of the instruments you are going to use, understand their function and practise the basic techniques of using them. 1 Scalpel A scalpel is a razor-edged blade on a handle. There are two types of surgical scalpel: reusable and disposable. Reusable scalpels consist of a blade that is replaced after every use, attached to a stainless steel handle that can be sterilised and re-used multiple times. In a hospital setting, this type is more likely to be used in order to reduce waste and to allow doctors to work with a variety of blades and handle sizes. Disposable surgical scalpels are usually single-piece with a plastic handle. This is the type provided in our Hands-on Kit for practice. Although you will use the same scalpel multiple times for practice, in a clinical setting you would dispose of the entire scalpel after a single use. 1.1 Principles A scalpel is essential for incising the skin and for sharp dissection. Held flat, it can also be useful for carefully undermining the skin edge to relieve tension. A razor edged blade engages over a flange on the scalpel handle. Several sizes of scalpel handle are available and size 3 is appropriate for most purposes. Each handle can be fitted with disposable blades of different shapes. The scalpel can be held in one of two ways: - For making large incisions e.g. laparotomy, and subcutaneous fat dissection, hold the scalpel like a table knife, with your index finger guiding the blade. -

(12) United States Patent (10) Patent No.: US 6,652,450 B2 Neisz Et Al
USOO665245OB2 (12) United States Patent (10) Patent No.: US 6,652,450 B2 Neisz et al. (45) Date of Patent: Nov. 25, 2003 (54) IMPLANTABLE ARTICLE AND METHOD FOREIGN PATENT DOCUMENTS FOR TREATING URINARY INCONTINENCE USING MEANS FOR REPOSITONING THE RE 5, c. 33. IMPLANTABLE ARTICLE EP O470308 A1 2/1992 EP O 650 703 A1 6/1994 (75) Inventors: Johann J. Neisz, Coon Rapids, MN (US); John W. Westrum, Jr., Prior (List continued on next page.) Lake, MN (US); Christopher H. Porter, Woodinville, WA (US) OTHER PUBLICATIONS Beck, Peter R. et al., Treatment of Urinary Stress Inconti (73) ASSignee: η Mystems Inc., nence With Anterior Colporrhaphy, Obstetrics and Gynecol InnelOn Ka, ogy, vol 59 (No. 3), pp. 269-274 (Mar. 1982). (*) Notice: Subject to any disclaimer, the term of this Es ES, MD, A Modified Play t atent is extended or adjusted under 35 patient Bladder Neck Suspension System, Journal of Urol C. 154(b) by 0 days ogy, vol. 152, pp. 23.16-2320 (Dec. 1994). a -- y yS. Benderev, Theodore V., MD, Anchor Fixation and Other Modifications of Endoscopic Bladder Neck Suspension, (21) Appl. No.: 09/917,562 Urology, vol 40, No. 5, pp. 409–418 (Nov. 1992). (22) Filed: Jul. 27, 2001 Das, Sakti et al., Laparoscopic Colpo-Suspension, The O O Journal of Urology, vol. 154, pp. 1119-1121 (Sep. 1995). (65) Prior Publication Data Gilja, Ivan et al., A Modified Raz Bladder Neck Suspension US 2002/0107430 A1 Aug. 8, 2002 Operation (Transvaginal Burch), The Journal of Urology, vol. 153, pp. 1455–1457 (May 1995). -
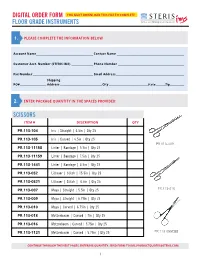
Floor Grade Instruments
DIGITAL ORDER FORM YOU MUST DOWNLOAD THIS FILE TO COMPLETE FLOOR GRADE INSTRUMENTS 1. PLEASE COMPLETE THE INFORMATION BELOW Account Name__________________________________________________ Contact Name ___________________________________________________________ Customer Acct. Number (STERIS IMS) ___________________ Phone Number __________________________________________________________ Fax Number _____________________________________________________ Email Address ____________________________________________________________ Shipping PO# _______________________ Address _____________________________________City __________________________________State ________ Zip_____________ 2. ENTER PACKAGE QUANTITY IN THE SPACES PROVIDED: SCISSORS ITEM # DESCRIPTION QTY PR.113-104 Iris | Straight | 4.5in | Qty 25 PR.113-105 Iris | Curved | 4.5in | Qty 25 PR.113-009 PR.113-11158 Lister | Bandage | 5.5in | Qty 25 PR.113-11159 Lister | Bandage | 7.5in | Qty 25 PR.113-1441 Lister | Bandage | 4.5in | Qty 25 PR.113-052 Littauer | Stitch | 15.5in | Qty 25 PR.113-0521 Littauer | Stitch | 4.5in | Qty 25 PR.113-007 Mayo | Straight | 5.5in | Qty 25 PR.113-010 PR.113-009 Mayo | Straight | 6.75in | Qty 25 PR.113-010 Mayo | Curved | 6.75in | Qty 25 PR.113-018 Metzenbaum | Curved | 7in | Qty 25 PR.113-016 Metzenbaum | Curved | 5.75in | Qty 25 PR.113-1121 Metzenbaum | Curved | 5.75in | Qty 25 PR.113-055CBB CONTINUE THROUGH THE NEXT PAGES, ENTERING QUANTITY. SEND FORM TO [email protected]. 1 SCISSORS ITEM # DESCRIPTION QTY PR.113-0063 Voper | Blunt | Straight -
Fine Surgical Instruments for Research™ Hsin-Yi Road, Sec
INTERNATIONAL Scissors, Bone Instruments Fine Science Tools Inc. & Scalpels 202-277 Mountain Highway pages 3–61 North Vancouver, British Columbia Canada V7J 3T6 Telephone 800-665-5355 / 604-980-2481 Fax 800-665-4544 / 604-987-3299 E-Mail [email protected] Web finescience.ca Fine Science Tools (USA) Inc. 373-G Vintage Park Drive F Forceps & Hemostats Foster City, California 94404-1139 I pages 63–97 Telephone 800-521-2109 / 650-349-1636 N Fax 800-523-2109 / 650-349-3729 E E-Mail [email protected] Web finescience.com S C I E Fine Science Tools GmbH N Vangerowstraße 14 C 69115 Heidelberg Germany E Telephone +49 (0) 62 21 - 90 50 50 Fax +49 (0) 62 21 - 90 50 590 T Probes, Needle Holders, O E-Mail [email protected] Thread, Retractors & Clamps Web finescience.de O pages 99–133 L S InterFocus Ltd. Pentagon Business Park Cambridge Road Linton, Cambridge CB21 4NN C United Kingdom A Telephone +44 (0)1223 894833 T Fax +44 (0)1223 894235 A Surgical & Laboratory E-Mail [email protected] L Accessories Web surgicaltools.co.uk O pages 135–161 G 2 Muromachi Kikai Co., Ltd. 0 4-2-12, Nihonbashi-Muromachi 1 Chuo-ku 4 Tokyo 103-0022 Japan Telephone (03) 3241-2444 Fax (03) 3241-2940 E-Mail [email protected] Student Quality Instruments Web muromachi.com pages 163–167 Proserv Instruments Co., Ltd. 7F-2, No. 413 Fine Surgical Instruments for Research™ Hsin-Yi Road, Sec. 4 Taipei, Taiwan R.O.C. Telephone (02) 27230455 Fax (02) 27230799 2014 E-Mail [email protected] Web proserv.com.tw TABLE OF CONTENTS | CATALOG 2014 Scissors 3 – 37 Spring 3 – 14 WE PROUDLY STOCK Fine 15 – 30 Surgical 31 – 37 Bone Instruments 38 – 51 DUMONT® Rongeurs 38 – 41 A selection of over 50 of the most popular Cutters 42 – 49 Other Bone Instruments 50 Dumont forceps are offered in this catalog. -

Federal Chargemaster Price Transparency Edgewood (2).Xlsx
EDGEWOOD SURGICAL HOSPITAL CHARGES Federal reporting rules require hospitals to maintain a catalog of thousands of procedure codes, code descriptions and list prices in a complex accounting tool, known as the hospital chargemaster. The prices listed on the chargemaster do not reflect what patients will ultimately pay as insurance companies negotiate discounts on the list prices. In addition, co-pays, co-insurance and deductibles can also bring additional discounts before a final charge is determined. To get an accurate estimate of what your out of pocket expenses will be, contact us at (724) 646-0400, Monday through Friday, from 8 a.m. – 4:30 p.m. Chg Code Description Chg Amt 1 NF-HUMULIN R INJ SOLN 100U/1ML $61.61 99077 EXTENDED RECOVERY ROOM PER MINUTE $15.00 99078 OBSERVATION 1-4 HOURS $550.00 99079 OBSERVATION >5 HOURS **EACH** $15.00 99085 OR TIME PER MINUTE COMPLEX (>3 STAFF) $197.00 99086 OR TIME PER MINUTE MAJOR (3 STAFF) $136.00 99087 OR TIME PER MINUTE MINOR (1-2 STAFF) $93.00 99088 SURGICAL NEUROMONITORING $1,350.00 99089 SURGICAL EYE LASER $1,743.00 99090 PAIN MANAGEMENT PER MINUTE $187.00 99091 OR TIME PER MINUTE ADDITIONAL STAFF $1.00 99092 FORCE TRIAD RENTAL $350.00 99093 YAG LASER CHARGE $1,182.00 99094 PAIN MANAGEMENT PER MINUTE RF $326.00 99100 CONS SEDATION (SAME DOC) <5YR 30-MIN $302.00 99101 CONS SEDATION (SAME DOC) <5YR 30-MIN $302.00 99102 CONS SEDATION (SAME DOC) ADD'S 15-MIN $151.00 99103 CONS SEDATION (DIFF DOC) <5YR 30-MIN $302.00 99104 CONS SEDATION (DIFF DOC) >5 YR 30-MIN $302.00 99105 CONS SEDATION (DIFF -

Product Catalog
precision crafted quality PRODUCT CATALOG www.medicaldevicepurchase.com 1-916-663-4165 2 precision crafted quality A letter from our CEO: Medical Device Purchase is a company started by my father and me almost 10 years ago. We knew the road ahead for MDP would be challenging and that we would inevitably face giant corporations that had been established in the industry for decades. Many said we would not even last two years. However, our approach was different from our competitors. We wanted to create a friendlier environment for healthcare professionals searching for industry-leading surgical products. How? By providing more—and higher quality—options. Our mission was to provide a welcoming environment where customers could enjoy a uniquely approachable buying experience. We wanted to build a brand that focused on creating efficiency and reliability so that our clients could spend more time on the things that really matter. Dr. Ray, our co-founder, passed away earlier this year, but the legacy of Medical Device Purchase lives on as we continue to grow and expand as a cutting edge company blazing new trails in the world of surgical products. Sincerely, Orin Ray www.medicaldevicepurchase.com 3 About MDP WHO WE ARE AND WHAT WE DO Medical Device Purchase is a leading supplier of premium quality surgical products, committed to satisfying the ever-growing demands of the healthcare community. We provide a new level of reliability, efficiency, and value by using applications, performance products, and technology unlike any any other supplier in the the industry. OUR MISSION As the cost of healthcare continues to rise, MDP remain committed to reducing your overhead. -

Measurement, Analysis, and Display of Haptic Signals During Surgical Cutting
Stephanie Greenish Measurement, Analysis, and Vincent Hayward [email protected] Display of Haptic Signals During Center for Intelligent Machines Surgical Cutting McGill University 3480 University Street Montre´al, Qc, Canada H3A 2A7 Vanessa Chial Allison Okamura Abstract Department of Mechanical Engineering The forces experienced while surgically cutting anatomical tissues from a sheep and The Johns Hopkins University two rats were investigated for three scissor types. Data were collected in situ using Baltimore, MD instrumented Mayo, Metzenbaum, and Iris scissors immediately after death to mini- mize postmortem effects. The force-position relationship, the frequency compo- Thomas Steffen nents present in the signal, the significance of the cutting rate, and other invariant Orthopaedic Research Laboratory properties were investigated after segmentation of the data into distinct task phases. Royal Victoria Hospital Measurements were found to be independent of the cutting speed for Mayo and Montre´al, Que´bec, Canada Metzenbaum scissors, but the results for Iris scissors were inconclusive. Sensitivity to cutting tissues longitudinally or transversely depended on both the tissue and on the scissor type. Data from cutting three tissues (rat skin, liver, and tendon) with Metzenbaum scissors as well as blank runs were processed and displayed as haptic recordings through a custom-designed haptic interface. Experiments demonstrated that human subjects could identify tissues with similar accuracy when performing a real or simulated cutting task. The use of haptic recordings to generate the simula- tions was simple and efficient, but it lacked flexibility because only the information obtained during data acquisition could be displayed. Future experiments should ac- count for the user grip, tissue thickness, tissue moisture content, hand orientation, and innate scissor dynamics. -

Supercut & Tungsten Carbide Instruments
SUPERCUT & TUNGSTEN carBIDE INSTRUMENTS 589 Davies Drive York, PA 17402 toll-free phone 866-854-8300 toll-free fax 866-854-8400 phone 717-840-9335 fax 717-840-9347 email [email protected] www.miltex.com INTRODUCTION The Miltex name is synonymous with premium surgical instrumentation. Manufactured of the highest quality stainless steel forgings by skilled German craftsmen to exacting specifications. The surgical “feel” of our instruments, the superb cutting ability, the smoothly beveled box locks and jaw edges which protect suture material from snags or cutting are just a few features that differentiate and make Miltex products outperform and stand-out from the competition. These premium SuperCut and Tungsten Carbide instruments include a comprehensive offering of scissors, needle holders, forceps, rasps and other specialty patterns. Our instrument selections recognize and meet the variety of clinical needs for all specialties including General Surgery, Plastic Surgery, Dermatology, Ophthalmology, Dentistry, Veterinary and many more. Illustrations and content signify general description only and may be subject to minor changes TABLE OF CONTENTS TABLE OF CONTENTS Scissors .................................................................. 4-19 Forceps ..................................................................20-23 Needle Holders .......................................................24-32 Specialty Patterns .....................................................33 Rasps .....................................................................34-36 www.miltex.com INSTRUMENT GRADES MILTEX® SUPERCUT SCISSORS SuperCut Scissors have a specially designed razor-sharp Razor-Sharp upper blade edge that cuts effortlessly through tissue. The Edge lower blade has micro-fine serrations to hold tissue and prevent slippage. For easy identification, Miltex SuperCut Scissors have two black ring handles. Micro-Fine Serrations SuperCut scissors are designed to cut tissue only. Dropping or mis- handling will cause the razor-sharp edge to nick or become irregular. -

General & Thoracic Simulation Surgery
GENERAL & THORACIC SIMULATION SURGERY Teaching for Developing Countries Manual Thomas M. Daniel, MD, FACS Professor Emeritus of Surgery, School of Medicine, University of Virginia Version 3.1 May 2016 Table of Contents Preface ......................................................................................................................................................................... 3 GENERAL & THORACIC SIMULATION SURGERY EXERCISES Exercise 1: Gastrojejunostomy ........................................................................................................................ 5 Figure 1 – PlAcement of StAy Sutures .................................................................................... 6 Figure 2 – Gastric Incision .......................................................................................................... 6 Figure 3 – JejunAl Incision .......................................................................................................... 7 Figure 4 – InitiAl Posterior SeromusculAr Suture ............................................................ 7 Figure 5 – Jejunum ApproximAted to StomAch with InitiAl ProximAl and DistAl Sutures ............................................................................................................. 8 Figure 6 – InitiAl Connell Suture PAssing Inside Out Through the DistAl JejunAl Wall .................................................................................................... 8 Figure 7 – Outside In Gastric Suture .....................................................................................