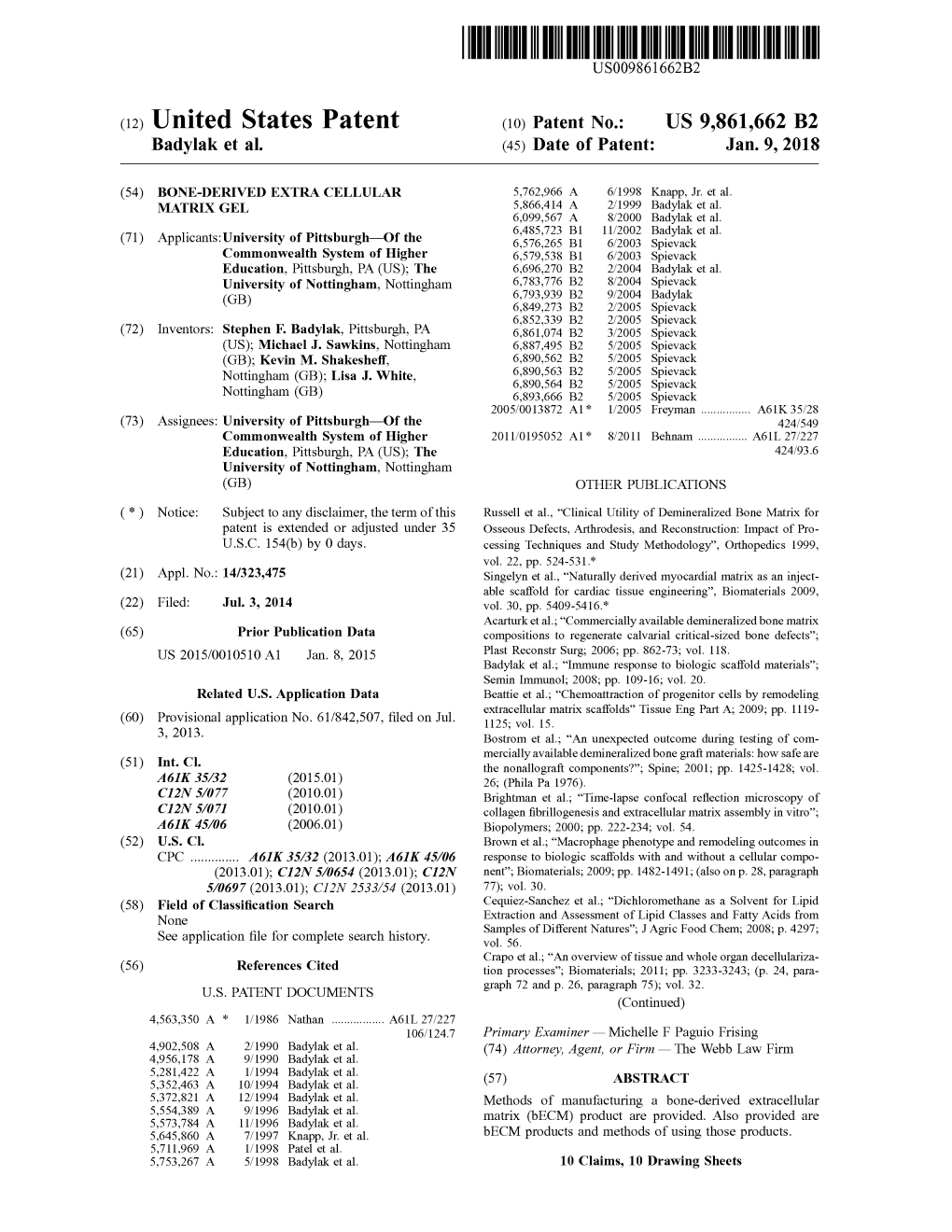
( 12 ) United States Patent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent (19) 11 Patent Number: 5,955,504 Wechter Et Al
USOO5955504A United States Patent (19) 11 Patent Number: 5,955,504 Wechter et al. (45) Date of Patent: Sep. 21, 1999 54 COLORECTAL CHEMOPROTECTIVE Marnett, “Aspirin and the Potential Role of Prostaglandins COMPOSITION AND METHOD OF in Colon Cancer, Cancer Research, 1992; 52:5575–89. PREVENTING COLORECTAL CANCER Welberg et al., “Proliferation Rate of Colonic Mucosa in Normal Subjects and Patients with Colonic Neoplasms: A 75 Inventors: William J. Wechter; John D. Refined Immunohistochemical Method.” J. Clin Pathol, McCracken, both of Redlands, Calif. 1990; 43:453-456. Thun et al., “Aspirin Use and Reduced Risk of Fatal Colon 73 Assignee: Loma Linda University Medical Cancer." N Engl J Med 1991; 325:1593-6. Center, Loma Linda, Calif. Peleg, et al., “Aspirin and Nonsteroidal Anti-inflammatory Drug Use and the Risk of Subsequent Colorectal Cancer.” 21 Appl. No.: 08/402,797 Arch Intern Med. 1994, 154:394–399. 22 Filed: Mar 13, 1995 Gridley, et al., “Incidence of Cancer among Patients With Rheumatoid Arthritis J. Natl Cancer Inst 1993 85:307-311. 51) Int. Cl. .......................... A61K 31/19; A61K 31/40; Labayle, et al., “Sulindac Causes Regression Of Rectal A61K 31/42 Polyps. In Familial Adenomatous Polyposis” Gastroenterol 52 U.S. Cl. .......................... 514/568; 514/569; 514/428; ogy 1991 101:635-639. 514/416; 514/375 Rigau, et al., “Effects Of Long-Term Sulindac Therapy On 58 Field of Search ..................................... 514/568, 570, Colonic Polyposis” Annals of Internal Medicine 1991 514/569, 428, 416, 375 11.5:952-954. Giardiello.et al., “Treatment Of Colonic and Rectal 56) References Cited Adenomas With Sulindac In Familial Adenomatous Poly U.S. -

Drug–Drug Salt Forms of Ciprofloxacin with Diflunisal and Indoprofen
CrystEngComm View Article Online COMMUNICATION View Journal | View Issue Drug–drug salt forms of ciprofloxacin with diflunisal and indoprofen† Cite this: CrystEngComm,2014,16, 7393 Partha Pratim Bag, Soumyajit Ghosh, Hamza Khan, Ramesh Devarapalli * Received 27th March 2014, and C. Malla Reddy Accepted 12th June 2014 DOI: 10.1039/c4ce00631c www.rsc.org/crystengcomm Two salt forms of a fluoroquinolone antibacterial drug, Crystal engineering approach has been effectively ciprofloxacin (CIP), with non-steroidal anti-inflammatory drugs, utilized in recent times in the synthesis of new forms particu- diflunisal (CIP/DIF) and indoprofen (CIP/INDP/H2O), were synthe- larly by exploiting supramolecular synthons. Hence the sized and characterized by PXRD, FTIR, DSC, TGA and HSM. Crystal identification of synthons that can be transferred across Creative Commons Attribution-NonCommercial 3.0 Unported Licence. structure determination allowed us to study the drug–drug different systems is important. For example, synthon trans- interactions and the piperazine-based synthon (protonated ferability in cytosine and lamivudine salts was recently dem- piperazinecarboxylate) in the two forms, which is potentially useful onstrated by Desiraju and co-workers by IR spectroscopy for the crystal engineering of new salt forms of many piperazine- studies.20a Aakeröy and co-workers successfully estab- based drugs. lished the role of synthon transferability (intermolecular amide⋯amide synthons) in the assembly and organization of Multicomponent pharmaceutical forms consisting of an bidentate acetylacetonate (acac) and acetate “paddlewheel” active pharmaceutical ingredient (API) and an inactive 20b complexes of a variety of metal(II)ions. Recently Das et al. co-former,whichisideallyagenerally recognized as safe – have reported the gelation behaviour in various diprimary This article is licensed under a 1 3 (GRAS) substance, have been well explored in recent times. -

Analgesic and Anti-Inflammatory Compositions Comprising of Using Same
Europaisches Patentamt J) European Patent Office Publication number: 0 1 65 308 Office europeen des brevets B1 EUROPEAN PATENT SPECIFICATION Date of publication of patent specification: 22.03.89 Intel.4: A 61 K 31/19, A 61 K 31/53 Application number: 85900409.5 Date of filing: 12.12.84 International application number: PCT/US84/02035 International publication number: WO 85/02540 20.06.85 Gazette 85/14 XANTHINES AND METHODS ANALGESIC AND ANTI-INFLAMMATORY COMPOSITIONS COMPRISING OF USING SAME. (30) Priority: 12.12.83 US 560576 Proprietor: Richardson-Vicks, Inc. Ten Westport Road Wilton, CT 06897 (US) (43) Date of publication of application: 27.12.85 Bulletin 85/52 Inventor: SUNSHINE, Abraham 254 East 68 Street Apt. 12D Publication of the grant of the patent: New York, NY 10021 (US) 22.03.89 Bulletin 89/12 Inventor: LASKA, Eugene, M. 34 Dante Street Larchmont, NY 10538 (US) Designated Contracting States: Inventor: SIEGEL, Carole, E. BEFR 1304 Colonial Court Mamaroneck, NY 10543 (US) References cited: WO-A-84/00487 @ Representative: Pendlebury, Anthony et al WO-A-84/00488 Page, White & Farrer 5 Plough Place New Fetter US-A-3439 094 Lane US-A-4479 956 London EC4A1HY(GB) Chemical Abstracts, vol. 96, no. 18, 3 May 1982, (58) References cited: Columbus, OH (US); Kaken Chemical Co.: 00 Clinical Pharmacol. Therapeutics, vol. 24, no. 1, "Combined analgesic and antipyretic A.K. et o 149 162u July 1978 (The C.V. Mosby Co.), Jain, formulations", p. 422, no. al.: and in « "Aspirin aspirin-caffeine postpartum pain relief, pp. 69-75 in Note: Within nine months from the publication of the mention of the grant of the European patent, any person may notice to the European Patent Office of opposition to the European patent granted. -

202439Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 202439Orig1s000 MEDICAL REVIEW(S) Clinical Review: Nhi Beasley, Preston Dunnmon and Martin Rose Application type: Standard, NDA 22-439 Xarelto (rivaroxaban) CLINICAL REVIEW Application Type NDA Type 1 -- (505(b)(1)) Application Number(s) 202439 Priority or Standard Standard Submit Date(s) 4 January 2011 Received Date(s) 5 January 2011 PDUFA Goal Date 5 November 2011 Division / Office DCRP/ODE 1 Reviewer Name(s) Nhi Beasley, Preston Dunnmon (safety); Martin Rose (efficacy) Review Completion Date 10 August 2011 Established Name Rivaroxaban Trade Name Xarelto® Therapeutic Class Anticoagulant (factor Xa inhibitor) Applicant Johnson & Johnson Pharmaceutical Research & Development, LLC Formulation(s) Oral tablets – 15 & 20 mg Dosing Regimen 15 or 20 mg once daily, based on renal function Indication(s) Prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation Intended Population(s) Adults Template Version: March 6, 2009 1 Reference ID: 2998874 Clinical Review: Nhi Beasley, Preston Dunnmon and Martin Rose Application type: Standard, NDA 22-439 Xarelto (rivaroxaban) Note to Readers In this review, a high level summary of the efficacy, safety and risk-benefit data is found in Section 1.2 Individual summaries of the efficacy and safety data are found at the beginning of Section 6 and Section 7, respectively. Internal hyperlinks to other parts of the review are in blue font. The Tables of Contents, Tables, and Figures are also hyperlinked to their targets. Table of Contents NOTE TO READERS ...................................................................................................... 2 TABLE OF CONTENTS .................................................................................................. 2 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ....................................... 10 1.1 Recommendation on Regulatory Action .......................................................... -

Indoprofen and Naproxen in the Treatment of Rheumatoid Arthritis
274 BRITISH MEDICAL JOURNAL 4 FEBRUARY 1978 Discussion haemorrhagic side effects has been based on trials in which anticoagulant dosage was determined by extrinsic clotting testsBr Med J: first published as 10.1136/bmj.1.6108.274 on 4 February 1978. Downloaded from The British comparative thromboplastin or its routine alone-that is, Quick prothrombin time test or Thrombotest. counterpart the Manchester comparative reagent is used in Our results also show the interesting and important finding that almost all hospitals in Britain. The BCT is also used throughout surgery is safe when intrinsic clotting is depressed, as judged by the world as a reference material. Hitherto the lower limits of a prolongation of PTT, provided that this is not excessive. the therapeutic range have been defined by clinical experience For moderate-risk patients, the necessary preoperative and correlation with other monitoring systems used in Britain stabilisation period for oral anticoagulants makes this type of and overseas. Our study allows an objective evaluation of the prophylaxis unnecessarily troublesome. For these patients the effectiveness of oral anticoagulant dosage monitored by the present study endorses the effectiveness of the fixed low-dose BCT to be made. The DVT incidence in untreated patients heparin regimen. If, however, a patient is already stabilised on (23%) agrees with other series. It is similar to that in the study of oral anticoagulants, it is apparently not worth changing to low- Ballard et a14 in gynaecological patients (290') and to that in the dose heparin for the operative period, as has recently been multicentre trial study8 of mixed surgical patients (24°0). -

Heparin EDTA Patent Application Publication Feb
US 20110027771 A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0027771 A1 Deng (43) Pub. Date: Feb. 3, 2011 (54) METHODS AND COMPOSITIONS FORCELL Publication Classification STABILIZATION (51) Int. Cl. (75)75) InventorInventor: tDavid Deng,eng, Mountain rView, V1ew,ar. CA C09KCI2N 5/073IS/00 (2006.01)(2010.01) C7H 2L/04 (2006.01) Correspondence Address: CI2O 1/02 (2006.01) WILSON, SONSINI, GOODRICH & ROSATI GOIN 33/48 (2006.01) 650 PAGE MILL ROAD CI2O I/68 (2006.01) PALO ALTO, CA 94304-1050 (US) CI2M I/24 (2006.01) rsr rr (52) U.S. Cl. ............ 435/2; 435/374; 252/397:536/23.1; (73) Assignee: Arts Health, Inc., San Carlos, 435/29: 436/63; 436/94; 435/6: 435/307.1 (21) Appl. No.: 12/847,876 (57) ABSTRACT Fragile cells have value for use in diagnosing many types of (22) Filed: Jul. 30, 2010 conditions. There is a need for compositions that stabilize fragile cells. The stabilization compositions of the provided Related U.S. Application Data inventionallow for the stabilization, enrichment, and analysis (60) Provisional application No. 61/230,638, filed on Jul. of fragile cells, including fetal cells, circulating tumor cells, 31, 2009. and stem cells. 14 w Heparin EDTA Patent Application Publication Feb. 3, 2011 Sheet 1 of 17 US 2011/0027771 A1 FIG. 1 Heparin EDTA Patent Application Publication Feb. 3, 2011 Sheet 2 of 17 US 2011/0027771 A1 FIG. 2 Cell Equivalent/10 ml blood P=0.282 (n=11) 1 hour 6 hours No Composition C Composition C Patent Application Publication Feb. -

Low Molecular Weight Heparin
LOW MOLECULAR WEIGHT HEPARIN (LMWH) AHFS ??? Indications: Prevention and treatment of deep vein thrombosis, pulmonary embolism, †thrombophlebitis migrans, †disseminated intravascular coagulation (DIC). Contra-indications: Active major bleeding, history of heparin-induced thrombocytopenia with unfractionated heparin, thrombocytopenia with positive anti- platelet antibody test, severe renal impairment ( certoparin, reviparin (not USA)). Pharmacology Several different varieties of low molecular weight heparin (LMWH) are now available (e.g. bemiparin , certoparin , dalteparin , enoxaparin , reviparin and tinzaparin ). Most are approved for the prevention of venous thrombo-embolism and some are also indicated for the treatment of deep vein thrombosis, pulmonary embolism, unstable coronary artery disease and for the prevention of clotting in extracorporeal circuits. All LMWH is derived from porcine heparin and some patients may need to avoid them because of hypersensitivity, or for religious or cultural reasons. The most appropriate non-porcine alternative is fondaparinux . LMWH acts by potentiating the inhibitory effect of antithrombin III on Factor Xa and thrombin. It has a relatively higher ability to potentiate Factor Xa inhibition than to prolong plasma clotting time (APTT) which cannot be used to guide dosage. Anti- factor Xa levels can be measured if necessary but routine monitoring is not required because the dose is determined by the patient’s weight. LMWH is as effective as unfractionated heparin for the treatment of deep vein thrombosis and pulmonary embolism and is now considered the initial treatment of choice. 1,2 Other advantages include a longer duration of action which allows administration q.d., and possibly a better safety profile, e.g. fewer major hemorrhages. 1-5 LMWH is the treatment of choice for chronic DIC; this commonly presents as recurrent thromboses in both superficial and deep veins which do not respond to warfarin . -

Treatment for Acute Pain: an Evidence Map Technical Brief Number 33
Technical Brief Number 33 R Treatment for Acute Pain: An Evidence Map Technical Brief Number 33 Treatment for Acute Pain: An Evidence Map Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. 290-2015-0000-81 Prepared by: Minnesota Evidence-based Practice Center Minneapolis, MN Investigators: Michelle Brasure, Ph.D., M.S.P.H., M.L.I.S. Victoria A. Nelson, M.Sc. Shellina Scheiner, PharmD, B.C.G.P. Mary L. Forte, Ph.D., D.C. Mary Butler, Ph.D., M.B.A. Sanket Nagarkar, D.D.S., M.P.H. Jayati Saha, Ph.D. Timothy J. Wilt, M.D., M.P.H. AHRQ Publication No. 19(20)-EHC022-EF October 2019 Key Messages Purpose of review The purpose of this evidence map is to provide a high-level overview of the current guidelines and systematic reviews on pharmacologic and nonpharmacologic treatments for acute pain. We map the evidence for several acute pain conditions including postoperative pain, dental pain, neck pain, back pain, renal colic, acute migraine, and sickle cell crisis. Improved understanding of the interventions studied for each of these acute pain conditions will provide insight on which topics are ready for comprehensive comparative effectiveness review. Key messages • Few systematic reviews provide a comprehensive rigorous assessment of all potential interventions, including nondrug interventions, to treat pain attributable to each acute pain condition. Acute pain conditions that may need a comprehensive systematic review or overview of systematic reviews include postoperative postdischarge pain, acute back pain, acute neck pain, renal colic, and acute migraine. -

(12) United States Patent (10) Patent No.: US 8,158,152 B2 Palepu (45) Date of Patent: Apr
US008158152B2 (12) United States Patent (10) Patent No.: US 8,158,152 B2 Palepu (45) Date of Patent: Apr. 17, 2012 (54) LYOPHILIZATION PROCESS AND 6,884,422 B1 4/2005 Liu et al. PRODUCTS OBTANED THEREBY 6,900, 184 B2 5/2005 Cohen et al. 2002fOO 10357 A1 1/2002 Stogniew etal. 2002/009 1270 A1 7, 2002 Wu et al. (75) Inventor: Nageswara R. Palepu. Mill Creek, WA 2002/0143038 A1 10/2002 Bandyopadhyay et al. (US) 2002fO155097 A1 10, 2002 Te 2003, OO68416 A1 4/2003 Burgess et al. 2003/0077321 A1 4/2003 Kiel et al. (73) Assignee: SciDose LLC, Amherst, MA (US) 2003, OO82236 A1 5/2003 Mathiowitz et al. 2003/0096378 A1 5/2003 Qiu et al. (*) Notice: Subject to any disclaimer, the term of this 2003/OO96797 A1 5/2003 Stogniew et al. patent is extended or adjusted under 35 2003.01.1331.6 A1 6/2003 Kaisheva et al. U.S.C. 154(b) by 1560 days. 2003. O191157 A1 10, 2003 Doen 2003/0202978 A1 10, 2003 Maa et al. 2003/0211042 A1 11/2003 Evans (21) Appl. No.: 11/282,507 2003/0229027 A1 12/2003 Eissens et al. 2004.0005351 A1 1/2004 Kwon (22) Filed: Nov. 18, 2005 2004/0042971 A1 3/2004 Truong-Le et al. 2004/0042972 A1 3/2004 Truong-Le et al. (65) Prior Publication Data 2004.0043042 A1 3/2004 Johnson et al. 2004/OO57927 A1 3/2004 Warne et al. US 2007/O116729 A1 May 24, 2007 2004, OO63792 A1 4/2004 Khera et al. -

Pharmaceutical Compositions Containing Non-Steroidal Anti-Inflammatory Drugs
Europaisches Patentamt J European Patent Office © Publication number: 0 259 047 Office europeen des brevets A1 s EUROPEAN PATENT APPLICATION © Application number: 87307246.6 © int. CIA A61K 45/06 A61 , K 31/60 , A61K 31/405, © Date of filing: 17.0&87 //(A61 K31/60,31 :1 85),(A61 K31/- 405,31:185) ® Priority: 18.08.86 GB 8620073 © Applicant: DELANDALE LABORATORIES LIMITED © Date of publication of application: Delandale House 37 Old Dover Road 09.03.88 Bulletin 88/10 Canterbury Kent CT1 3JF(GB) © Designated Contracting States: @ inventor: Trigger, David John AT BE CH DE ES FR GB GR IT LI LU NL SE 74 Mountbatten Way Brabourne Lees Ashford Kent TN25 6PU(GB) © Representative: Paget, Hugh Charles Edward etal MEWBURN ELUS & CO. 2/3 Cursitor Street London EC4A 1BQ(GB) © Pharmaceutical compositions containing non-steroidal anti-Inflammatory drugs. © A pharmaceutical composition for treating an inflammatory condition contains a non-steroidal anti-inflam- matory drug (NSAID) and a physiologically acceptable aromatic hydroxysulphonic acid. The two components may be for simultaneousr separate or sequential use. Administration of the two components, for example of aspirin with ethamsylate, reduces the damage which the NSAID does to the gastrointestinal tract while having no deleterious effect on the anti-inflammatory activity. s in cm Q. LU Xerox Copy Centre 0 259 047 PHARMACEUTICAL COMPOSITIONS CONTAINING NON-STEROIDAL ANTI-INFLAMMATORY DRUGS The present invention relates to pharmaceutical compositions containing aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs). The non-steroidal anti-inflammatory drugs are a group of compounds which inhibit the biosynthesis of prostaglandins. -

PAI-19-2 Master
Research article Singlet oxygen scavenging activity of non- steroidal anti-inflammatory drugs David Costa, Ana Gomes, José L.F.C. Lima, Eduarda Fernandes REQUIMTE, Departamento de Química-Física, Faculdade de Farmácia, Universidade do Porto, Porto, Portugal 1 It has long been known that singlet oxygen ( O2) is generated during inflammatory processes. 1 Once formed in substantial amounts, O2 may have an important role in mediating the destruction 1 of infectious agents during host defense. On the other hand, O2 is capable of damaging almost all biological molecules and is particularly genotoxic, which gives a special relevance to the scavenging of this ROS throughout anti-inflammatory treatments. Considering that the use of non- steroidal anti-inflammatory drugs (NSAIDs) constitutes a first approach in the treatment of persistent inflammatory processes (due to their ability to inhibit cyclooxygenase), a putative 1 scavenging activity of NSAIDs for O2 would also represent a significant component of their 1 therapeutic effect. The aim of the present study was to evaluate the scavenging activity for O2 by several chemical families of NSAIDs. The results suggested that the pyrazole derivatives (dipyrone 1 and aminopyrine) are, by far, the most potent scavengers of O2 (much more potent compared to the other tested NSAIDs), displaying IC 50 -values in the low micromolar range. There was a lack of activity for most of the arylpropionic acid derivatives tested, with only naproxen and indoprofen displaying residual activities, as for the oxazole derivative, oxaprozin. On the other hand, the pyrrole derivatives (tolmetin and ketorolac), the indolacetic acid derivatives (indomethacin, and etodolac), as well as sulindac and its metabolites (sulindac sulfide and sulindac sulfone) displayed scavenging activity in the high micromolar range. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of - Medicines belonging to the ATC group M01 (Antiinflammatory and antirheumatic products) Table of Contents Page INTRODUCTION 6 DISCLAIMER 8 GLOSSARY OF TERMS USED IN THIS DOCUMENT 9 ACTIVE SUBSTANCES Phenylbutazone (ATC: M01AA01) 11 Mofebutazone (ATC: M01AA02) 17 Oxyphenbutazone (ATC: M01AA03) 18 Clofezone (ATC: M01AA05) 19 Kebuzone (ATC: M01AA06) 20 Indometacin (ATC: M01AB01) 21 Sulindac (ATC: M01AB02) 25 Tolmetin (ATC: M01AB03) 30 Zomepirac (ATC: M01AB04) 33 Diclofenac (ATC: M01AB05) 34 Alclofenac (ATC: M01AB06) 39 Bumadizone (ATC: M01AB07) 40 Etodolac (ATC: M01AB08) 41 Lonazolac (ATC: M01AB09) 45 Fentiazac (ATC: M01AB10) 46 Acemetacin (ATC: M01AB11) 48 Difenpiramide (ATC: M01AB12) 53 Oxametacin (ATC: M01AB13) 54 Proglumetacin (ATC: M01AB14) 55 Ketorolac (ATC: M01AB15) 57 Aceclofenac (ATC: M01AB16) 63 Bufexamac (ATC: M01AB17) 67 2 Indometacin, Combinations (ATC: M01AB51) 68 Diclofenac, Combinations (ATC: M01AB55) 69 Piroxicam (ATC: M01AC01) 73 Tenoxicam (ATC: M01AC02) 77 Droxicam (ATC: M01AC04) 82 Lornoxicam (ATC: M01AC05) 83 Meloxicam (ATC: M01AC06) 87 Meloxicam, Combinations (ATC: M01AC56) 91 Ibuprofen (ATC: M01AE01) 92 Naproxen (ATC: M01AE02) 98 Ketoprofen (ATC: M01AE03) 104 Fenoprofen (ATC: M01AE04) 109 Fenbufen (ATC: M01AE05) 112 Benoxaprofen (ATC: M01AE06) 113 Suprofen (ATC: M01AE07) 114 Pirprofen (ATC: M01AE08) 115 Flurbiprofen (ATC: M01AE09) 116 Indoprofen (ATC: M01AE10) 120 Tiaprofenic Acid (ATC: