Labeling: • Hypersensitivity Reactions Including Infusion-Associated Events [See Warnings and Precautions (5.1)]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antimicrobial Stewardship Guidance
Antimicrobial Stewardship Guidance Federal Bureau of Prisons Clinical Practice Guidelines March 2013 Clinical guidelines are made available to the public for informational purposes only. The Federal Bureau of Prisons (BOP) does not warrant these guidelines for any other purpose, and assumes no responsibility for any injury or damage resulting from the reliance thereof. Proper medical practice necessitates that all cases are evaluated on an individual basis and that treatment decisions are patient-specific. Consult the BOP Clinical Practice Guidelines Web page to determine the date of the most recent update to this document: http://www.bop.gov/news/medresources.jsp Federal Bureau of Prisons Antimicrobial Stewardship Guidance Clinical Practice Guidelines March 2013 Table of Contents 1. Purpose ............................................................................................................................................. 3 2. Introduction ...................................................................................................................................... 3 3. Antimicrobial Stewardship in the BOP............................................................................................ 4 4. General Guidance for Diagnosis and Identifying Infection ............................................................. 5 Diagnosis of Specific Infections ........................................................................................................ 6 Upper Respiratory Infections (not otherwise specified) .............................................................................. -

Refreshing the Biologic Pipeline 2020
news feature Credit: Science Lab / Alamy Stock Photo Refreshing the biologic pipeline 2020 In the absence of face-to-face meetings, FDA and industry implemented regulatory workarounds to maintain drug and biologics approvals. These could be here to stay. John Hodgson OVID-19 might have been expected since 1996) — a small miracle in itself “COVID-19 confronted us with the need to severely impair drug approvals (Fig. 1 and Table 1). to better triage sponsors’ questions,” says Cin 2020. In the event, however, To the usual crop of rare disease and Peter Marks, the director of the Center for industry and regulators delivered a small genetic-niche cancer treatments, 2020 Biologics Evaluation and Research (CBER) miracle. They found workarounds and also added a chimeric antigen receptor at the FDA. “That was perhaps the single surrogate methods of engagement. Starting (CAR)-T cell therapy with a cleaner biggest takeaway from the pandemic related in January 2020, when the outbreak veered manufacturing process and the first to product applications.” Marks says that it westward, the number of face-to face approved blockbuster indication for a became very apparent with some COVID- meetings declined rapidly; by March, small-interfering RNA (siRNA) — the 19-related files that resolving a single they were replaced by Webex and Teams. European Medicines Agency’s (EMA) issue can help a sponsor enormously and (Secure Zoom meeting are to be added registration of the RNA interference accelerate the development cycle. Before this year.) And remarkably, by 31 December, (RNAi) therapy Leqvio (inclisiran) for COVID-19, it was conceivable that a small the US Food and Drug Administration cardiovascular disease. -

Atoltivimab, Maftivimab, and Odesivimab
PATIENT & CAREGIVER EDUCATION Atoltivimab, Maftivimab, and Odesivimab This information from Lexicomp® explains what you need to know about this medication, including what it’s used for, how to take it, its side effects, and when to call your healthcare provider. What is this drug used for? It is used to treat infections caused by Ebolavirus. What do I need to tell my doctor BEFORE I take this drug? If you are allergic to this drug; any part of this drug; or any other drugs, foods, or substances. Tell your doctor about the allergy and what signs you had. If you are breast-feeding. Do not breast-feed while you take this drug. This drug may interact with other drugs or health problems. Tell your doctor and pharmacist about all of your drugs (prescription or OTC, natural products, vitamins) and health problems. You must check to make sure that it is safe for you to take this drug with all of your drugs and health problems. Do not start, stop, or change the dose of any drug without checking with your doctor. Atoltivimab, Maftivimab, and Odesivimab 1/5 What are some things I need to know or do while I take this drug? Tell all of your health care providers that you take this drug. This includes your doctors, nurses, pharmacists, and dentists. Talk with your doctor before getting any vaccines. Use of some vaccines with this drug may either raise the chance of an infection or make the vaccine not work as well. Tell your doctor if you are pregnant or plan on getting pregnant. -

General a Number of Factors Could Reduce the Efficacy of This
AUSTRALIAN PRODUCT INFORMATION Administration It is strongly recommended that every time that GAMUNEX® is administered to a patient, the name Use in the elderly GAMUNEX® If dilution is required, GAMUNEX® may be diluted with 5% dextrose in water (D5/W). Do not and batch number of the product are recorded using the supplied tear off labels in order to maintain See Section 4.4 Special warnings and precautions for use: Use in renal impairment. a link between the patient and the batch of the product. (NORMAL IMMUNOGLOBULIN (HUMAN), 10%, INTRAVENOUS SOLUTION VIAL) dilute with saline. Paediatric use Anaphylaxis GAMUNEX® should be inspected visually for particulate matter and discoloration prior to adminis - No data available. GAMUNEX® should be administered only intravenously or subcutaneously. On rare occasions, tration, whenever solution and container permit. Do not use if turbid and/or if discoloration is Effects on laboratory tests 1 NAME OF THE MEDICINE observed. treatment with an immune globulin preparation may cause a precipitous fall in blood pressure and a Interference with serological testing Normal immunoglobulin (Human), 10%, for Intravenous or Subcutaneous Administration For intravenous or subcutaneous administration, GAMUNEX® should be at room temperature during clinical picture of anaphylaxis, even when the patient is not known to be sensitive to immune globulin administration. preparations. Adrenalin and other appropriate supportive care should be available for the treatment After injection of immunoglobulin the transitory rise of the various passively transferred antibodies of an acute anaphylactic reaction. in the patient’s blood may result in misleading positive results in serological testing. Passive Intravenous (IV) True anaphylactic reactions to GAMUNEX® may occur in recipients with documented prior histories transmission of antibodies to erythrocyte antigens e.g. -

October 2020
PharmNOTES Summary about new FDA-approved products, new indications, first-time generics, and WHAT IS IN THE PIPELINE. From: OCTOBER 2020 Date: 11/06/2020 ©2020 PharmPix. All rights reserved Table of Contents Page News 3 New FDA Approved Products 4-5 Inmazeb™ (atoltivimab, maftivimab, and odesivimab-ebgn) 4 Veklury™ (remdesivir) 5 New FDA Approved Formulations, Dosage Forms, Combination Products and Other Differences 6 New FDA Approved Indications 7 New First-Time Generic Drug Approval 8 Pipeline 9 References 10 2 NEWS ……………………………………………………………………………………………………………... Drug issue Date Details Avoid Use of NSAIDs in 10/15/2020 The FDA issued a warning to avoid the use of Non-steroidal Anti-inflammatory Drugs (NSAIDs) during pregnancy at 20 weeks or Pregnancy at 20 Weeks later. The use of NSAIDs around 20 weeks or later in pregnancy may cause serious kidney problems in the fetus, low levels of or Later amniotic fluids, and other complications. Previously NSAIDs labels warned to avoid use during the last three (3) months of pregnancy due to the risk of premature closure of the fetal ductus arteriosus. The FDA now requires changes in the prescribing information for both prescription and over the counter (OTC) NSAIDs. Recommendations for healthcare professionals: • Advise pregnant women to avoid the use of NSAIDs at 20 weeks of pregnancy or later. • If NSAIDs are necessary during 20 to 30 weeks of pregnancy, limit treatment to the lowest dose possible and for the shortest duration. Consider ultrasound monitoring of amniotic fluid if treatment extends over 48 hours. If low levels of amniotic fluid are identified, discontinue the NSAID. -

Polymyxin B Use Associated with Severe Hypotensive Episodes
ntimicrob Mehta et al., J Antimicro 2015, 1:1 A ia f l o A l g DOI: 10.4172/2472-1212.1000102 a e n n r Journal of t u s o J ISSN: 2472-1212 Antimicrobial Agents Case Report Open Access Polymyxin B use Associated with Severe Hypotensive Episodes Mehta M1*, Baron JM1, Nelson BC1, Muir J1 and Pereira MR2 1NewYork-Presbyterian Hospital, USA 2Columbia University Medical Center, USA Abstract Polymyxin B was developed in the 1940s but was infrequently used because of renal toxicity. Since the rise of infections due to multidrug resistant gram-negative organisms, polymyxin B has re-emerged as an important agent. However, its toxicity is still not fully elucidated. In this report, we describe two cases of multiple hypotensive events occurring after polymyxin B administration. Management strategies, such as slowing the infusion rate and administering diphenhydramine, did not mitigate the hypotension. We also describe relatively high polymyxin levels correlated with this effect in one of these cases. Keywords: Polymyxin; Toxicity; Hypotension While hypotension is usually a complication of sepsis, details in this case suggest that the episodes of hypotension are more related Case 1 to polymyxin B administration than an uncontrolled infection. The A 35-year-old-woman was admitted to our hospital for management episodes of hypotension started to occur only after polymyxin B and of newly diagnosed acute promyelocytic leukemia. Twelve days after other antibiotics were initiated. There is good evidence, with negative initiation of chemotherapy, she developed a fever to 38.0°C. Cultures follow-up cultures, resolution of fever, and improving imaging, that of her urine and blood grew a carbapenem-resistant Escherichia coli the infection was controlled by the time that the hypotensive episodes susceptible to polymyxin B (minimum inhibitory concentration started. -

Remifentanil Hydrochloride)
NDA 20-630/S-005 Page 3 Ultiva® for Injection (remifentanil hydrochloride) For IV Use Only DESCRIPTION ULTIVA (remifentanil hydrochloride) for Injection is a µ-opioid agonist chemically designated as a 3- [4-methoxycarbonyl-4-[(1-oxopropyl)phenylamino]-1-piperidine]propanoic acid methyl ester, hydrochloride salt, C20H28N2O5·HCl, with a molecular weight of 412.91. It has the following chemical structure: ULTIVA is a sterile, nonpyrogenic, preservative-free, white to off-white lyophilized powder for intravenous (IV) administration after reconstitution and dilution. Each vial contains 1, 2, or 5 mg of remifentanil base; 15 mg glycine; and hydrochloric acid to buffer the solutions to a nominal pH of 3 after reconstitution. When reconstituted as directed, solutions of ULTIVA are clear and colorless and contain remifentanil hydrochloride (HCl) equivalent to 1 mg/mL of remifentanil base. The pH of reconstituted solutions of ULTIVA ranges from 2.5 to 3.5. Remifentanil HCl has a pKa of 7.07. Remifentanil HCl has an n-octanol:water partition coefficient of 17.9 at pH 7.3. CLINICAL PHARMACOLOGY ULTIVA is a µ-opioid agonist with rapid onset and peak effect, and short duration of action. The µ-opioid activity of ULTIVA is antagonized by opioid antagonists such as naloxone. Unlike other opioids, ULTIVA is rapidly metabolized by hydrolysis of the propanoic acid-methyl ester linkage by nonspecific blood and tissue esterases. ULTIVA is not a substrate for plasma cholinesterase (pseudocholinesterase) and, therefore, patients with atypical cholinesterase are expected to have a normal duration of action. Pharmacodynamics: The analgesic effects of ULTIVA are rapid in onset and offset. -

A Short Overview of Ebola Virus Disease
Short Communication Journal of Volume 6:4, 2021 DOI: 10.37421/jidm.2021.6.173 Infectious Diseases and Medicine A Short Overview of Ebola Virus Disease Akshay Thiwari* Department of Virology, University of Hyderabad, Hyderabad, Telangana, India Ebola [1] is an uncommon but lethal virus that causes fever, body Treatment for Ebola aches, diarrhea, and, in some cases, internal and external bleeding. The Ebola has no known cure, though researchers are working on one. For immune system and organs are harmed as the virus spreads through the the treatment of Ebola [2], two drug therapies have been authorized. Inmazeb body. As a result, the number of blood-clotting cells decreases. As a is a compound that consists of three monoclonal antibodies (atoltivimab, consequence, there is a lot of uncontrollable bleeding. Ebola hemorrhagic maftivimab, and odesivimab-ebgn). Ebanga (ansuvimab-zykl) is a monoclonal fever was the previous name for the outbreak, but it is now known as Ebola antibody that is given as an injection. It aids in stopping the virus from reaching virus. It kills up to 90% of those who become infected. the cell receptor. Doctors treat Ebola symptoms [3] with the following How does one contract Ebola? medication. Ebola isn't as infectious as viruses like the common cold, influenza, or Electrolytes and fluids, Oxygen (O2), Medication for high blood pressure, measles. Contact with the skin or bodily fluids of an infected animal, such as Transfusions of blood, and other diseases'. a monkey, chimp, or fruit bat, transmits the disease to humans. Then it Facts on Ebola passes from one person to the next in the same manner. -

Package Insert
response and target IgG at 15 mL/hr/site 20 mL/hr/site HIGHLIGHTS OF PRESCRIBING trough level (2.2). INFORMATION . Ensure that patients with pre-existing renal insufficiency are not volume depleted; discontinue GAMMAGARD LIQUID if renal function These highlights do not include all the information needed to use deteriorates. (2.3, 5.2) GAMMAGARD LIQUID safely and effectively. See full prescribing . For patients at risk of renal dysfunction or thrombotic events, administer information for GAMMAGARD LIQUID. GAMMAGARD LIQUID at the minimum infusion rate practicable. (2.3, 5.2, 5.4) GAMMAGARD LIQUID, Immune Globulin Infusion (Human), 10% --------------DOSAGE FORMS AND STRENGTHS--------- Solution, for intravenous and subcutaneous administration . Aqueous solution containing 10% IgG (100 milligram/mL) (3) ---------------------CONTRAINDICATIONS ------------------- Initial U.S. Approval: 2005 . Anaphylactic or severe systemic hypersensitivity reactions to Immune Warning: RENAL DYSFUNCTION & ACUTE RENAL FAILURE Globulin (Human) (4) See full prescribing information for complete boxed warning . IgA deficient patients with antibodies against IgA and a history of . Renal dysfunction, acute renal failure, osmotic nephropathy, and hypersensitivity (4) death may occur with immune globulin intravenous (IGIV) -----------------WARNINGS AND PRECAUTIONS---------- products in predisposed patients. Renal dysfunction and acute . IgA deficient patients with antibodies to IgA are at greater risk of developing failure occur more commonly in patients receiving IGIV severe hypersensitivity and anaphylactic reaction. (5.1) products containing sucrose. GAMMAGARD LIQUID does not . Monitor renal function, including blood urea nitrogen, serum creatinine, and contain sucrose. urine output in patients at risk of acute renal failure. (5.2) . For patients at risk of renal dysfunction or failure, administer . Hyperproteinemia, increased serum viscosity and hyponatremia may occur. -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -
Oxytocin to Accelerate Or Induce Labour
CLINICAL PRACTICE GUIDELINE OXYTOCIN CLINICAL PRACTICE GUIDELINE OXYTOCIN TO ACCELERATE OR INDUCE LABOUR Institute of Obstetricians and Gynaecologists, Royal College of Physicians of Ireland and the Clinical Strategy and Programmes Division, Health Service Executive Version: 1.0 Publication date: April 2016 Guideline No: 36 Revision date: April 2019 CLINICAL PRACTICE GUIDELINE OXYTOCIN Table of Contents 1. Revision History ....................................................................................................................... 3 2. Key recommendations .......................................................................................................... 3 3. Purpose and Scope ................................................................................................................. 4 4. Background ............................................................................................................................... 5 5. Methodology .............................................................................................................................. 9 6. Clinical guideline ................................................................................................................... 10 7. References .............................................................................................................................. 16 8. Implementation Strategy ................................................................................................... 19 9. Key Performance Indicators ............................................................................................ -
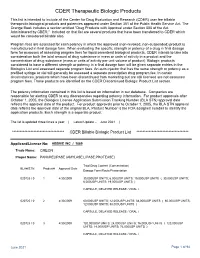
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database.