Genevista Genetics of Premature Ovarian Failure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prioritization of Variants Detected by Next Generation Sequencing According to the Mutation Tolerance and Mutational Architecture of the Corresponding Genes
International Journal of Molecular Sciences Review Prioritization of Variants Detected by Next Generation Sequencing According to the Mutation Tolerance and Mutational Architecture of the Corresponding Genes Iria Roca, Ana Fernández-Marmiesse, Sofía Gouveia, Marta Segovia and María L. Couce * Unit of Diagnosis and Treatment of Congenital Metabolic Diseases, Department of Pediatrics, Hospital Clínico Universitario de Santiago de Compostela, 15706 Santiago de Compostela, Spain; [email protected] (I.R.); [email protected] (A.F.-M.); sofi[email protected] (S.G.); [email protected] (M.S.) * Correspondence: [email protected]; Tel.: +34-981-950-102 Received: 3 April 2018; Accepted: 23 May 2018; Published: 27 May 2018 Abstract: The biggest challenge geneticists face when applying next-generation sequencing technology to the diagnosis of rare diseases is determining which rare variants, from the dozens or hundreds detected, are potentially implicated in the patient’s phenotype. Thus, variant prioritization is an essential step in the process of rare disease diagnosis. In addition to conducting the usual in-silico analyses to predict variant pathogenicity (based on nucleotide/amino-acid conservation and the differences between the physicochemical features of the amino-acid change), three important concepts should be borne in mind. The first is the “mutation tolerance” of the genes in which variants are located. This describes the susceptibility of a given gene to any functional mutation and depends on the strength of purifying selection acting against it. The second is the “mutational architecture” of each gene. This describes the type and location of mutations previously identified in the gene, and their association with different phenotypes or degrees of severity. -

Lamin A/C Cardiomyopathy: Implications for Treatment
Current Cardiology Reports (2019) 21:160 https://doi.org/10.1007/s11886-019-1224-7 MYOCARDIAL DISEASE (A ABBATE AND G SINAGRA, SECTION EDITORS) Lamin A/C Cardiomyopathy: Implications for Treatment Suet Nee Chen1 & Orfeo Sbaizero1,2 & Matthew R. G. Taylor1 & Luisa Mestroni1 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review The purpose of this review is to provide an update on lamin A/C (LMNA)-related cardiomyopathy and discuss the current recommendations and progress in the management of this disease. LMNA-related cardiomyopathy, an inherited autosomal dominant disease, is one of the most common causes of dilated cardiomyopathy and is characterized by steady progression toward heart failure and high risks of arrhythmias and sudden cardiac death. Recent Findings We discuss recent advances in the understanding of the molecular mechanisms of the disease including altered cell biomechanics, which may represent novel therapeutic targets to advance the current management approach, which relies on standard heart failure recommendations. Future therapeutic approaches include repurposed molecularly directed drugs, siRNA- based gene silencing, and genome editing. Summary LMNA-related cardiomyopathy is the focus of active in vitro and in vivo research, which is expected to generate novel biomarkers and identify new therapeutic targets. LMNA-related cardiomyopathy trials are currently underway. Keywords Lamin A/C gene . Laminopathy . Heart failure . Arrhythmias . Mechanotransduction . P53 . CRISPR–Cas9 therapy Introduction functions, including maintaining nuclear structural integrity, regulating gene expression, mechanosensing, and Mutations in the lamin A/C gene (LMNA)causelaminopathies, mechanotransduction through the lamina-associated proteins a heterogeneous group of inherited disorders including muscu- [6–11]. -

WES Gene Package Multiple Congenital Anomalie.Xlsx
Whole Exome Sequencing Gene package Multiple congenital anomalie, version 5, 1‐2‐2018 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 607922 101 100 100 99 [Blood group, P1Pk system, p phenotype], 111400 NOR polyagglutination syndrome, 111400 AAAS Achalasia‐addisonianism‐alacrimia syndrome, 231550 605378 73 100 100 100 AAGAB Keratoderma, palmoplantar, -

The Genetic Mechanism That Links Hutchinson-Gilford Progeria Syndrome to Physiological Aging
Department of Biosciences and Nutrition The genetic mechanism that links Hutchinson-Gilford progeria syndrome to physiological aging AKADEMISK AVHANDLING som för avläggande av medicine doktorsexamen vid Karolinska Institutet offentligen försvaras i Hörsalen, plan 4, Novum, Huddinge. Fredagen den 14 februari, 2014, kl 09.15 av Sofía Rodríguez Vásquez B.Sc. Licentiate in Biological Sciences Huvudhandledare: Fakultetsopponent: Docent Maria Eriksson Professor Karima Djabali Karolinska Institutet Technical University Munich Institutionen för Biovetenskaper och Department of Dermatology and Näringslära Institute for Medical Engineering Bihandledare: Betygsnämnd: Professor Karin Dahlman-Wright Docent Rickard Sandberg Karolinska Institutet Karolinska Institutet Institutionen för Biovetenskaper och Institutionen för Cell- och Molekylär Näringslära Biologi Professor Caroline Graff Professor Brun Ulfhake Karolinska Institutet Karolinska Institutet Institutionen för Neurobiologi, Institutionen för Neurovetenskap Vårdvetenskap och Samhälle Professor Jan Dumanski Uppsala Universitet Institutionen för Immunologi, Genetik och Patologi. Enheten för Medicinsk Genetik Stockholm 2014 DEPARTMENT OF BIOSCIENCES AND NUTRITION Karolinska Institutet, Stockholm, Sweden THE GENETIC MECHANISM THAT LINKS HUTCHINSON-GILFORD PROGERIA SYNDROME TO PHYSIOLOGICAL AGING Sofía Rodríguez Vásquez Stockholm 2014 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. © Sofia Rodríguez Vásquez, 2014 ISBN 978-91-7549-372-5 Printed by Printed by 2014 Gårdsvägen 4, 169 70 Solna Dedicated to my beloved parents and life heroes: Benito Rodríguez Rodríguez & Doris Vásquez Silva ABSTRACT Aging is a complex process that is not completely understood. The study of segmental progeroid syndromes such as Hutchinson-Gilford progeria syndrome (HGPS) has allowed us to connect the common genetic mechanisms that occur in normal physiological aging, with the cellular alterations presented by this severe premature aging syndrome. -

Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel
Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel Overview Arthrogryposis or arthrogryposis multiplex congenita (AMC) is a group of nonprogressive conditions characterized by multiple joint contractures found throughout the body at birth. It usually appears as a feature of other neuromuscular conditions or part of systemic diseases. Primary cases may present prenatally with decreased fetal movements associated with joint contractures as well as brain abnormalities, decreased muscle bulk and polyhydramnios whereas secondary causes may present with isolated contractures. Congenital Myasthenic Syndromes (CMS) are a clinically and genetically heterogeneous group of disorders characterized by impaired neuromuscular transmission. Clinically they usually present with abnormal fatigability upon exertion, transient weakness of extra-ocular, facial, bulbar, truncal or limb muscles. Severity ranges from mild, phasic weakness, to disabling permanent weakness with respiratory difficulties and ultimately death. The mode of inheritance of these diseases typically follows and autosomal recessive pattern, although dominant forms can be seen. The Igenomix Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel can be as a tool for an accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved, and their high or intermediate penetrance. -

Case Report of Malouf Syndrome Not Associated with LMNA Gene Mutation
MOJ Clinical & Medical Case Reports Case Report Open Access Case report of malouf syndrome not associated with LMNA gene mutation Abstract Volume 4 Issue 6 - 2016 Malouf syndrome, currently known as dilated cardiomyopathy associated with Tatiyana G Vaikhanskaya,1 Larysa N hypergonadotropic hypogonadism (DCM-НН), is a rare congenital disorder with Sivitskaya,2 Nina G Danilenko,2 Tatsiyana V clinical signs including DCM phenotype, ovary dysgenesis in females or primary 1 2 testicular failure in males, mental retardation, facial dysmorphism, skin lesions, bone Kurushka, Oleg G Davydenko abnormalities and occasionally marfanoid habitus. The disorder can be caused by 1Health Information Technology Department, Republican mutation in the LMNA gene, encoding lamins A and C. In the present manuscript, Scientific and Practical Centre of Cardiology, Belarus we report the sporadic case of a young female with dilated cardiomyopathy, 2Cytoplasmic Inheritance Department, Institute of Genetics hypergonadotropic hypogonadism and primary amenorrhea, cognitive deficiency, and Cytology of the National Academy of Sciences of Belarus, body mass deficit, facial dysmorphism and subclinical hypothyroidism. Radiation Belarus exposure, mumps, diabetes mellitus, autoimmune diseases, and Turner’s syndrome have been ruled out. Specific features of mandibuloacral dysplasia, like bone dysplasia, Correspondence: Tatiyana G Vaikhanskaya, Health Information are absent. The first-degree relatives are healthy. The clinical data suggested a Technology Department, Republican Scientific and Practical laminopathy. Targeted next-generation sequencing was used to search for mutations in Centre of Cardiology, 220036, R Lyuksembourg str 110, Minsk, genes, associated with cardiomyopathy, including LMNA. However, genetic analysis Belarus, Tel +375291307140, Email [email protected] did not confirm the assumption: mutation was not found. -

Sema4 Cardiac Information Sheet
CARDIAC NEXT-GENERATION SEQUENCING PANELS Mail: One Gustave L. Levy Place, Box 1497 1 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com 0 3 8 Mail: One Gustave L. Levy Place, Box 1497 2 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com Mail: One Gustave L. Levy Place, Box 1497 3 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com Mail: One Gustave L. Levy Place, Box 1497 4 CLIA #: 33D2097541 Specimens: 1428 Madison Ave, Atran Bldg, Rm 2-25 T: 800-298-6470 New York, NY 10029 F: 212-241-0139 www.sema4.com TABLE OF CONTENTS GENETIC TESTING FOR INHERITED CARDIOVASCULAR CONDITIONS 6 GENETICS AND INDICATIONS 6 TESTING METHODS, SENSITIVITY, AND LIMITATIONS 7 TURNAROUND TIME 9 SPECIMEN AND SHIPPING REQUIREMENTS 9 CUSTOMER SERVICES AND GENETIC COUNSELING 10 THE COMPREHENSIVE CARDIOMYOPATHY PANEL 11 DILATED CARDIOMYOPATHY (DCM) SUBPANEL 23 ARRHYTHMOGENIC RIGHT VENTRICULAR CARDIOMYOPATHY (ARVC) SUBPANEL 28 HYPERTROPHIC CARDIOMYOPATHY (HCM) SUBPANEL 30 LEFT VENTRICULAR NON-COMPACTION CARDIOMYOPATHY (LVNC) SUBPANEL 33 THE COMPREHENSIVE ARRHYTHMIAS PANEL 35 BRUGADA SYNDROME (BRS) SUBPANEL 40 CATECHOLAMINERGIC POLYMORPHIC VENTRICULAR TACHYCARDIA (CPVT) SUBPANEL 42 LONG / SHORT QT SYNDROME (LQTS / SQTS) SUBPANEL 44 AORTOPATHIES PANEL 46 CONGENITAL HEART DISEASE (CHD) PANEL 49 FAMILIAL HYPERCHOLESTEROLEMIA (FH) PANEL 52 PULMONARY HYPERTENSION (PAH) PANEL 54 METABOLIC CARDIOMYOPATHY PANEL 55 NOONAN SPECTRUM DISORDERS PANEL 57 HEREDITARY HEMORRHAGIC TELANGIECTASIA PANEL 59 REFERENCES 60 DISCLAIMER 69 Mail: One Gustave L. -

Hutchinson-Gilford Progeria Syndrome—Current Status and Prospects for Gene Therapy Treatment
cells Review Hutchinson-Gilford Progeria Syndrome—Current Status and Prospects for Gene Therapy Treatment Katarzyna Piekarowicz † , Magdalena Machowska † , Volha Dzianisava and Ryszard Rzepecki * Laboratory of Nuclear Proteins, Faculty of Biotechnology, University of Wroclaw, Fryderyka Joliot-Curie 14a, 50-383 Wroclaw, Poland; [email protected] (K.P.); [email protected] (M.M.); [email protected] (V.D.) * Correspondence: [email protected]; Tel.: +48-71-3756308 † Joint first author. Received: 1 December 2018; Accepted: 19 January 2019; Published: 25 January 2019 Abstract: Hutchinson-Gilford progeria syndrome (HGPS) is one of the most severe disorders among laminopathies—a heterogeneous group of genetic diseases with a molecular background based on mutations in the LMNA gene and genes coding for interacting proteins. HGPS is characterized by the presence of aging-associated symptoms, including lack of subcutaneous fat, alopecia, swollen veins, growth retardation, age spots, joint contractures, osteoporosis, cardiovascular pathology, and death due to heart attacks and strokes in childhood. LMNA codes for two major, alternatively spliced transcripts, give rise to lamin A and lamin C proteins. Mutations in the LMNA gene alone, depending on the nature and location, may result in the expression of abnormal protein or loss of protein expression and cause at least 11 disease phenotypes, differing in severity and affected tissue. LMNA gene-related HGPS is caused by a single mutation in the LMNA gene in exon 11. The mutation c.1824C > T results in activation of the cryptic donor splice site, which leads to the synthesis of progerin protein lacking 50 amino acids. -

Blueprint Genetics Comprehensive Muscular Dystrophy / Myopathy Panel
Comprehensive Muscular Dystrophy / Myopathy Panel Test code: NE0701 Is a 125 gene panel that includes assessment of non-coding variants. In addition, it also includes the maternally inherited mitochondrial genome. Is ideal for patients with distal myopathy or a clinical suspicion of muscular dystrophy. Includes the smaller Nemaline Myopathy Panel, LGMD and Congenital Muscular Dystrophy Panel, Emery-Dreifuss Muscular Dystrophy Panel and Collagen Type VI-Related Disorders Panel. About Comprehensive Muscular Dystrophy / Myopathy Muscular dystrophies and myopathies are a complex group of neuromuscular or musculoskeletal disorders that typically result in progressive muscle weakness. The age of onset, affected muscle groups and additional symptoms depend on the type of the disease. Limb girdle muscular dystrophy (LGMD) is a group of disorders with atrophy and weakness of proximal limb girdle muscles, typically sparing the heart and bulbar muscles. However, cardiac and respiratory impairment may be observed in certain forms of LGMD. In congenital muscular dystrophy (CMD), the onset of muscle weakness typically presents in the newborn period or early infancy. Clinical severity, age of onset, and disease progression are highly variable among the different forms of LGMD/CMD. Phenotypes overlap both within CMD subtypes and among the congenital muscular dystrophies, congenital myopathies, and LGMDs. Emery-Dreifuss muscular dystrophy (EDMD) is a condition that affects mainly skeletal muscle and heart. Usually it presents in early childhood with contractures, which restrict the movement of certain joints – most often elbows, ankles, and neck. Most patients also experience slowly progressive muscle weakness and wasting, beginning with the upper arm and lower leg muscles and progressing to shoulders and hips. -

Dilated Cardiomyopathy and Ovarian Dysgenesis in a Patient with Malouf Syndrome: a Case Report
MOLECULAR MEDICINE REPORTS 8: 1311-1314, 2013 Dilated cardiomyopathy and ovarian dysgenesis in a patient with Malouf syndrome: A case report KSENIJA GERSAK1, MARUSA STRGULC1, VOJKA GORJUP2, ZVEZDANA DOLENC-STRAZAR3, VESNA JURCIC3, DANIEL J. PENNY4 and YUXIN FAN4 1Department of Obstetrics and Gynecology; 2Division of Intensive Internal Medicine, Department of Internal Medicine, University Medical Center Ljubljana; 3Institute of Pathology, Medical Faculty, University of Ljubljana, Ljubljana SI-1000, Slovenia; 4John Welsh Cardiovascular Diagnostic Laboratory, Section of Cardiology, Department of Pediatrics, Baylor College of Medicine, Houston, TX 77030, USA Received March 2, 2013; Accepted July 15, 2013 DOI: 10.3892/mmr.2013.1669 Abstract. Malouf syndrome is a rare congenital disorder DCM-HH may be caused by heterozygous mutations involving the heart, genitalia, skin and skeletal characteris- in the lamin A/C (LMNA) gene. Chen et al (6) identified tics. In the present study, we report on the sporadic case of three heterozygous missense mutations A57P, R133L and a young female with dilated cardiomyopathy, hypergonado- L140R in the LMNA gene in four patients reported to exhibit tropic hypogonadism, a small chin, bilateral blepharoptosis, atypical Werner syndrome (adult progeria) (7). The mutations marfanoid elongated fingers and hypothyroidism. Malouf altered relatively conserved residues in LMNA. syndrome may be caused by heterozygous mutations in the The heterozygous missense mutation L59R, in the LMNA lamin A/C (LMNA) gene. Genetic analyses and autopsy gene, was identified by McPherson et al (8), who noted the were performed. In spite of the patient's features, sequence phenotypic similarities between their case, with cardiomyop- analysis of the coding region of the LMNA gene including athy and hypergonadotropic hypogonadism, and female cases exon‑intron boundaries identified only one benign polymor- previously studied by Nguyen et al (9) and Chen et al (6), phism: homozygous silent variant 1698C>T (H566). -

Clinical Approach to Genetic Cardiomyopathy in Children Marcy L
(Circulation. 1996;94:2021-2038.) © 1996 American Heart Association, Inc. Articles Clinical Approach to Genetic Cardiomyopathy in Children Marcy L. Schwartz, MD; Gerald F. Cox, MD, PhD; Angela E. Lin, MD; Mark S. Korson, MD; Antonio Perez-Atayde, MD; Ronald V. Lacro, MD; Steven E. Lipshultz, MD the Department of Cardiology (M.L.S., R.V.L., S.E.L.), Division of Genetics, Inborn Errors of Metabolism Service, Department of Medicine (G.F.C., M.S.K.), and Department of Pathology (A.P.-A.), Children's Hospital, Boston, Mass; and Department of Pediatrics (M.L.S., G.F.C., M.S.K., R.V.L., S.E.L.) and Department of Pathology (A.P.-A.), Harvard Medical School, Boston, Mass. Correspondence to Steven E. Lipshultz, MD, Department of Cardiology, Children's Hospital, 300 Longwood Ave, Boston, MA 02115. E-mail [email protected]. Abstract Background Cardiomyopathy (CM) remains one of the leading cardiac causes of death in children, although in the majority of cases, the cause is unknown. To have an impact on morbidity and mortality, attention must shift to etiology-specific treatments. The diagnostic evaluation of children with CM of genetic origin is complicated by the large number of rare genetic causes, the broad range of clinical presentations, and the array of specialized diagnostic tests and biochemical assays. Methods and Results We present a multidisciplinary diagnostic approach to pediatric CM of genetic etiology. We specify criteria for abnormal left ventricular systolic performance and structure that suggest CM based on established normal echocardiographic measurements and list other indications to consider an evaluation for CM. -
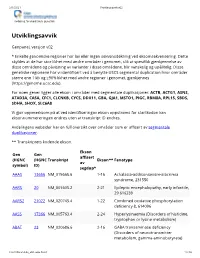
Utviklingsavvik V02
2/1/2021 Utviklingsavvik v02 Avdeling for medisinsk genetikk Utviklingsavvik Genpanel, versjon v02 * Enkelte genomiske regioner har lav eller ingen sekvensdekning ved eksomsekvensering. Dette skyldes at de har stor likhet med andre områder i genomet, slik at spesifikk gjenkjennelse av disse områdene og påvisning av varianter i disse områdene, blir vanskelig og upålitelig. Disse genetiske regionene har vi identifisert ved å benytte USCS segmental duplication hvor områder større enn 1 kb og ≥90% likhet med andre regioner i genomet, gjenkjennes (https://genome.ucsc.edu). For noen gener ligger alle ekson i områder med segmentale duplikasjoner: ACTB, ACTG1, ASNS, ATAD3A, CA5A, CFC1, CLCNKB, CYCS, DDX11, GBA, GJA1, MSTO1, PIGC, RBM8A, RPL15, SBDS, SDHA, SHOX, SLC6A8 Vi gjør oppmerksom på at ved identifiseringav ekson oppstrøms for startkodon kan eksonnummereringen endres uten at transkript ID endres. Avdelingens websider har en full oversikt over områder som er affisert av segmentale duplikasjoner. ** Transkriptets kodende ekson. Ekson Gen Gen affisert (HGNC (HGNC Transkript Ekson** Fenotype av symbol) ID) segdup* AAAS 13666 NM_015665.6 1-16 Achalasia-addisonianism-alacrimia syndrome, 231550 AARS 20 NM_001605.2 2-21 Epileptic encephalopathy, early infantile, 29 616339 AARS2 21022 NM_020745.4 1-22 Combined oxidative phosphorylation deficiency 8, 614096 AASS 17366 NM_005763.4 2-24 Hyperlysinaemia (Disorders of histidine, tryptophan or lysine metabolism) ABAT 23 NM_020686.6 2-16 GABA transaminase deficiency (Disorders of neurotransmitter metabolism, gamma-aminobutyrate)