Multi-Drug Resistance of MRSA Isolated Strains from Healthcare, Community and the Distribution of Fusidic Acid MIC and Zone Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mechanisms and Strategies to Overcome Multiple Drug Resistance in Cancer
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector FEBS Letters 580 (2006) 2903–2909 Minireview Mechanisms and strategies to overcome multiple drug resistance in cancer Tomris Ozben* Akdeniz University, Faculty of Medicine, Department of Biochemistry, 07070 Antalya, Turkey Received 30 January 2006; accepted 9 February 2006 Available online 17 February 2006 Edited by Horst Feldmann The cytotoxic drugs that are most frequently associated with Abstract One of the major problems in chemotherapy is multi- drug resistance (MDR) against anticancer drugs. ATP-binding MDR are hydrophobic, amphipathic natural products, such as cassette (ABC) transporters are a family of proteins that medi- the taxanes (paclitaxel and docetaxel), vinca alkaloids (vinorel- ate MDR via ATP-dependent drug efflux pumps. Many MDR bine, vincristine, and vinblastine), anthracyclines (doxorubicin, inhibitors have been identified, but none of them have been pro- daunorubicin, and epirubicin), epipodophyllotoxins (etoposide ven clinically useful without side effects. Efforts continue to dis- and teniposide), antimetabolites (methorexate, fluorouracil, cover not toxic MDR inhibitors which lack pharmacokinetic cytosar, 5-azacytosine, 6-mercaptopurine, and gemcitabine) interactions with anticancer drugs. Novel approaches have also topotecan, dactinomycin, and mitomycin C [4,6–8]. been designed to inhibit or circumvent MDR. In this review, Overexpression of ATP-binding cassette (ABC) transporters the structure and function of ABC transporters and development has been shown to be responsible for MDR [5]. Therefore eluci- of MDR inhibitors are described briefly including various ap- dation of the structure and function for each ABC transporter is proaches to suppress MDR mechanisms. -

Expression of Cytokeratin Confers Multiple Drug Resistance (Multidrug Resance/Cytoskeleton) PATRICIA A
Proc. Nati. Acad. Sci. USA Vol. 91, pp. 5311-5314, June 1994 Pharmacology Expression of cytokeratin confers multiple drug resistance (multidrug resance/cytoskeleton) PATRICIA A. BAUMAN*, WILLIAM S. DALTON*t, JOHN M. ANDERSONt, AND ANNE E. CRESSO§ Departments of *Pharmacology and Toxicology, tMedicine, and *Radiation Oncology, The University of Arizona, The Arizona Cancer Center, Tucson, AZ 85724 Communicated by Gertrude B. Elion, February 23, 1994 (received for review October 21, 1993) ABSTRACT The cytokeratin network is an extensive fda- We utilized a mouse fibroblast cell line and a transfected mentous structure in the cytoplasm whose biological function(s) variant expressing cytokeratins 8 and 18 (9) to test whether is unknown. Based upon previous data showing the modifica- cytokeratin expression could alter the cell survival response tion ofcytokeratin by mitoxantrone, we investigated the ability to six different chemotherapeutic drugs. of cytokeratin networks to influence the survival response of cells to chemotherapeutic agents. We have compared the MATERIALS AND METHODS survival of mouse L fibroblasts lacking cytokeratins with that of L cells transfected with cytokeratins 8 and 18 in the presence Tumor Cell Lines, Growth Curves, and Cell Cycle Distri- of chemotherapeutic drugs. The expression of cytokeratins 8 butions. Parental L cells and transfected LK8+18 cells were and 18 conferred a multiple drug resistance phenotype on cells obtained from Robert Oshima (La Jolla Cancer Research exposed to mitoxantrone, doxorubicin, methotrexate, melpha- Foundation, La Jolla, CA) and maintained as described (9). Ian, Colcemid, and vincristine. The degree of drug resistance Mock transfectants (LPBMOC) were created by simultane- was 5-454 times that of parental cells, depending upon the ous calcium phosphate transfection of pGEM-3 (Promega) agent used. -

Resistance to Paromomycinis Conferred by Rpsl Mutations
VOL.53 NO. 12, DEC.2000 THE JOURNAL OF ANTIBIOTICS pp.1424 - 1427 COMMUNICATIONS TO THE EDITOR Resistance to Paromomycinis Conferred by paromomycin at a frequency of 10 7 or 10 8, respectively. rpsL Mutations, Accompaniedby an Out of 77 randomly selected paromomycin resistant Enhanced Antibiotic Production in mutants, 4 strains, designated as KO-347-350, were found to produce actinorhodin in 7 to 10-fold greater amounts Streptomyces coelicolor A3 (2) than the parent strain (Table 1). In our previous studies10'11>14) we established that an antibiotic- Sir: overproducing characteristic frequently appears together Aminoglycoside antibiotics interfere with bacterial with the mutation within the rpsL gene. To address this protein synthesis by binding to the 3OS ribosomal relationship weexamined for the presence of mutations in subunit1>2). Their binding is known to stabilize the tRNA- rpsL. Strikingly, all antibiotic-overproducing mutants mRNAinteraction in the A-site by decreasing the tRNA (Class I) examined had rpsL mutations, resulting in the dissociation rates3). Eventually, aminoglycoside antibiotics alteration of amino acid residue 91 from proline to serine cause a decrease in translational accuracy and inhibit (Table 1). In contrast, another group of paromomycin translocation of the ribosome. Such detrimental effects of resistant mutant, (Class II; KO-351-356) which do not aminoglycoside antibiotics can be circumvented by overproduce antibiotic, was found to have no mutation mutations altering 16S rRNA4~6) or certain ribosomal within the rpsL gene. It should be pointed out that Class I proteins6^; these mutations have been found in either the mutants displayed a higher level of resistance to nucleotide 530 or 915 regions of 16S rRNAor in ribosomal paromomycin than that of Class II mutants (Table 1). -

Association of Genetic and Nongenetic Variabilities With
ASSOCIATION OF GENETIC AND NONGENETIC VARIABILITIES WITH PHENYTOIN AND CARBAMAZEPINE RESPONSE PHENOTYPES A DISSERTATION SUBMITTED TO THE FACULTY OF THE GRADUATE SCHOOL OF THE UNIVERSITY OF MINNESOTA BY PORNPIMOL KIJSANAYOTIN IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY RICHARD BRUNDAGE ADVISOR APRIL, 2012 © Pornpimol Kisanayotin 2012 Acknowledgements It has been a long time since I decided to pursue the PhD study in the US after receiving a scholarship from the Royal Thai Government. Without the following people I could not be able to follow my dream to successfully conduct this pharmacogenetic study for my PhD dissertation. First, I would like to express my deep gratitude to Prof. James C Cloyd and Prof. Ilo E Leppik for not only giving me the opportunity to carry out this research work by using data sets from the P50 program projects but also all their academic and financial support. I also would like to express my special gratitude to Prof. Richard Brundage, my advisor, for his kindness, academic advice as well as all his support and encouragement. I express my gratitude to Prof. William S Oetting, my co-advisor for his academic advice and encouraging words. I also express my gratitude to Prof. Richard King for allowing me to use his laboratory, facilities and providing technical support for genotyping work. I would like to thank Dr. Angela K Burnbaum and all the staff at the Epilepsy Reseach and Education Program, University of Minnesota for all their assistance in research. I would like to thank Dr. Elving Anderson for his kindness and academic advice. -

Farrukh Javaid Malik
I Farrukh Javaid Malik THESIS PRESENTED TO OBTAIN THE GRADE OF DOCTOR OF THE UNIVERSITY OF BORDEAUX Doctoral School, SP2: Society, Politic, Public Health Specialization Pharmacoepidemiology and Pharmacovigilance By Farrukh Javaid Malik “Analysis of the medicines panorama in Pakistan – The case of antimicrobials: market offer width and consumption.” Under the direction of Prof. Dr. Albert FIGUERAS Defense Date: 28th November 2019 Members of Jury M. Francesco SALVO, Maître de conférences des universités – praticien hospitalier, President Université de Bordeaux M. Albert FIGUERAS, Professeur des universités – praticien hospitalier, Director Université Autonome de Barcelone Mme Antonia AGUSTI, Professeure, Vall dʹHebron University Hospital Referee Mme Montserrat BOSCH, Praticienne hospitalière, Vall dʹHebron University Hospital Referee II Abstract A country’s medicines market is an indicator of its healthcare system, the epidemiological profile, and the prevalent practices therein. It is not only the first logical step to study the characteristics of medicines authorized for marketing, but also a requisite to set up a pharmacovigilance system, thus promoting rational drug utilization. The three medicines market studies presented in the present document were conducted in Pakistan with the aim of describing the characteristics of the pharmaceutical products available in the country as well as their consumption at a national level, with a special focus on antimicrobials. The most important cause of antimicrobial resistance is the inappropriate consumption of antimicrobials. The results of the researches conducted in Pakistan showed some market deficiencies which could be addressed as part of the national antimicrobial stewardship programmes. III Résumé Le marché du médicament d’un pays est un indicateur de son système de santé, de son profil épidémiologique et des pratiques [de prescription] qui y règnent. -

Multiple Drug Resistance: a Fast-Growing Threat
Review Article ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2019.21.003572 Multiple Drug Resistance: A Fast-Growing Threat Eremwanarue Aibuedefe Osagie1,2* and Shittu Hakeem Olalekan1 1Department of Plant Biology and Biotechnology, University of Benin, Nigeria 2Lahor Research Laboratories and Diagnostics Centre, Nigeria *Corresponding author: Eremwanarue Aibuedefe Osagie, Department of Plant Biology and Biotechnology, University of Benin, Nigeria ARTICLE INFO Abstract Received: September 03, 2019 The spread of antibiotic resistant bacteria is a growing problem and a public health Published: September 10, 2019 issue. Over the years, various genetic mechanisms concerned with antibiotic resistance have been identified to be natural and acquired resistance. The natural resistance Citation: Eremwanarue Aibuedefe Osag- ie, Shittu Hakeem Olalekan. Multiple Geneticinvolved Elements mutation [MGEs] via target such modification,as plasmid, transposon reduced permeability, and integrons efflux genetic system elements and Drug Resistance: A Fast-Growing Threat. on the other hand, acquired resistance via horizontal gene tranfer include Moblie Biomed J Sci & Tech Res 21(2)-2019. Integrons are widely distributed, especially in Gram-negative bacteria; they are carried BJSTR. MS.ID.003572. bythat Mobile can acquire, Genetic exchange, Elements and such express as plasmids, genes embeddedand transposons, within whichGene Cassettespromote [GC].their spread within bacterial communities and have been studied mainly in the clinical setting Keywords: Antibiotics; Multiple Drug for their involvement in antibiotic resistance, their role in the environment is now an Resistant Bacteria; Mobile Genetic increasing focus of attention. The aim of this review is to educate the populise about Element; Integrons Plasmid the mechanisms of multiple drug resistance bacteria isolates and the danger ahead if appropriate regulations are not put in place especially in developing country like Nigeria. -
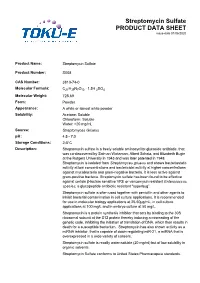
Streptomycin Sulfate PRODUCT DATA SHEET Issue Date 01/06/2020
Streptomycin Sulfate PRODUCT DATA SHEET issue date 01/06/2020 Product Name: Streptomycin Sulfate Product Number: S008 CAS Number: 3810-74-0 Molecular Formula: C21H39N7O12 · 1.5H 2SO4 Molecular Weight: 728.69 Form: Powder Appearance: A white or almost white powder Solubility: Acetone: Soluble Chloroform: Soluble Water: >20 mg/mL Source: Streptomyces Griseus pH: 4.5 - 7.0 Storage Conditions: 28°C Description: Streptomycin sulfate is a freely soluble aminocyclitol glycoside antibiotic, that was co-discovered by Salman Waksman, Albert Schatz, and Elizabeth Bugie at the Rutgers University in 1943 and was later patented in 1948. Streptomycin is isolated from Streptomyces griseus and shows bacteriostatic activity at low concentrations and bactericidal activity at higher concentrations against mycobacteria and gram-negative bacteria. It is less active against gram-positive bacteria. Streptomycin sulfate has been found to be effective against certain βlactam sensitive VRE or vancomycin resistant Enterococcus species; a glycopeptide antibiotic resistant "superbug”. Streptomycin sulfate is often used together with penicillin and other agents to inhibit bacterial contamination in cell culture applications. It is recommended for use in molecular biology applications at 2550μg/mL, in cell culture applications at 100 mg/L and in embryo culture at 50 mg/L. Streptomycin is a protein synthesis inhibitor that acts by binding to the 30S ribosomal subunit at the S12 protein thereby inducing a misreading of the genetic code, inhibiting the initiation of translation of DNA, which then results in death for a susceptible bacterium. Streptomycin has also shown activity as a miRNA inhibitor, that is capable of down-regulating miR-21, a miRNA that is overexpressed in a wide variety of cancers. -

Neomycin—Production and Antibiotic Properties
NEOMYCIN—PRODUCTION AND ANTIBIOTIC PROPERTIES Selman A. Waksman, … , Hubert A. Lechevalier, Dale A. Harris J Clin Invest. 1949;28(5):934-939. https://doi.org/10.1172/JCI102182. Research Article Find the latest version: https://jci.me/102182/pdf NEOMYCIN-PRODUCTION AND ANTIBIOTIC PROPERTIES 1, 2 3 By SELMAN A. WAKSMAN, HUBERT A. LECHEVALIER, AND DALE A. HARRIS (From the Department of Microbiology, New Jersey Agricultural Experiment Station, Rutgers University, New Brunswick, N. J.) ANTIBIOTIC SURVEYS All these cultures proved to be highly active against mycobacteria. of During the last 10 years, a large number anti- Only few of the cultures, however, that gave biotics which are active against Gram-negative good activity by the agar-streak method yielded and Gram-positive bacteria, mycobacteria, rickett- filtrates which possessed corresponding potency. siae, and certain of the larger viruses were iso- This may be due to a variety of factors, such as lated (1) from various species and strains of the the formation by a single organism of more than genus Streptomyces. This served to focus atten- one antibiotic or the production of different anti- tion on the actinomycetes as potential producers of biotics under different conditions of culture. One antimicrobial agents that might possess promising of these cultures proved to be highly promising chemotherapeutic properties. The fact that nearly and was selected for more detailed investigations. 20 to 50%o of these organisms possess antimicrobial This culture was entered into the Collection as No. activities served to heighten this interest. Numer- 3535. The nature of its antimicrobial spectrum, ous surveys have been conducted. -

Fisher Bioreagents Antibiotics and Antimycotics Catalog
Fisher BioReagents® Antibiotics and Antimycotics In many life science laboratories, the in vitro culturing of bacterial, Optimized for cell culture plant, and animal cells is a routine task. High quality antibiotics and antimycotics from Fisher BioReagents can be used to ensure success- ful growth of cells by eliminating unwanted bacterial strains and fungi while maintaining the health and vitality of the desired cells. Advantages • High quality - antibiotics and antimycotics meet rigorous quality control tests, including verifi cation of potency, purity, and solubility using microbiological and chromatographic methods. • Built for selection - excellent choice of antibiotics for selection of antibiotic resistance genes in both bacterial and mammalian cells. • High purity and stability - ultrapure antibiotics ensure successful growth of target cells and reproducible results. • Maximum convenience - antibiotics and antimycotics come in both sterile powder and liquid forms. Applications • Plant cell culture • Mammalian cell culture • Tissue culture • Genetic marker selection Table 1. Antibiotic modes of action Molecular Catalog No. Product Description Mode of Action Susceptible Organisms Form Size Packaging Weight Inhibitor of protein disulfide isomerase. Interferes with BP2950-1 Bacitracin 1422.7 Gram+ Dry 1g Amber glass bottle building blocks of peptidoglycan bacterial cell wall. Inhibitor of bacterial cell wall synthesis. Eliminates BP2951-1 Cefotaxime Sodium Salt 477.5 Gram- Dry 1g Amber glass bottle Agrobacterium species after inoculation. BP2952- Prokaryotes and higher Crimp top on glass Hygromycin B 527.5 Inhibits protein synthesis. Liquid 1mu 1MU eukaryotes bottle Alters membrane permeability and allows potassium ion BP2949-5 Nystatin 926.1 Yeasts and molds Dry 5g Amber glass bottle leakage. BP2953-1 Paromomycin Sulfate 615.6 Inhibits protein synthesis. -

SEPSIS AMINOGLYCOSIDES Examples: Streptomycin, Gentamicin
SEPSIS AMINOGLYCOSIDES Examples: streptomycin, gentamicin, tobramycin Mechanism of action A bactericidal group of drugs which inhibit bacterial protein synthesis by irreversibly binding bacterial ribosomes. They require entry to Gram negative bacterial cells through outer cell membrane (via porins) and inner cytoplasmic membrane (an oxygen-dependent system) in order to exert their effect. They have difficulty penetrating Gram positive cell walls. They are therefore effective against Gram negative aerobic bacteria but not against anaerobic gram negative bacteria whose cell wall/membranes the antibiotic cannot penetrate. They have limited application against Gram positive bacteria. Synergistic with penicillins - cell wall synthesis inhibitors increase the permeability of the cell wall to aminoglycosides. They do not cross the blood brain barrier and have low concentrations in many tissues. They reach high concentrations in the inner ears and kidneys. Adverse Effects Ototoxicity - accumulates in the endolymph and perilymph of the inner ear causing deafness, tinnitus and vertigo. Increased risk with co-use of loop diuretics and cisplatin. Nephrotoxicity - retention of aminoglycosides by proximal tubular cells disrupts calcium- mediated transport processes resulting in nephrotoxicity. This ranges from mild, reversible renal impairment to severe, irreversible acute tubular necrosis. Dose, frequency and duration of therapy determine the extent of nephrotoxicity. Other adverse effects - allergy, neuromuscular blockade. They cross the placenta and may cause congenital deafness. Gentamicin Prescribing Where possible prescribe gentamicin using the Gentamicin calculator. If critically ill and gentamicin is needed prescribe 5mg/kg actual body weight (max 400mg). If critically ill and known CKD stage V give 2.5mg/kg (max 180mg). Always prescribe gentamicin on the Gentamicin prescription chart. -
Third ESVAC Report
Sales of veterinary antimicrobial agents in 25 EU/EEA countries in 2011 Third ESVAC report An agency of the European Union The mission of the European Medicines Agency is to foster scientific excellence in the evaluation and supervision of medicines, for the benefit of public and animal health. Legal role Guiding principles The European Medicines Agency is the European Union • We are strongly committed to public and animal (EU) body responsible for coordinating the existing health. scientific resources put at its disposal by Member States • We make independent recommendations based on for the evaluation, supervision and pharmacovigilance scientific evidence, using state-of-the-art knowledge of medicinal products. and expertise in our field. • We support research and innovation to stimulate the The Agency provides the Member States and the development of better medicines. institutions of the EU the best-possible scientific advice on any question relating to the evaluation of the quality, • We value the contribution of our partners and stake- safety and efficacy of medicinal products for human or holders to our work. veterinary use referred to it in accordance with the • We assure continual improvement of our processes provisions of EU legislation relating to medicinal prod- and procedures, in accordance with recognised quality ucts. standards. • We adhere to high standards of professional and Principal activities personal integrity. Working with the Member States and the European • We communicate in an open, transparent manner Commission as partners in a European medicines with all of our partners, stakeholders and colleagues. network, the European Medicines Agency: • We promote the well-being, motivation and ongoing professional development of every member of the • provides independent, science-based recommenda- Agency. -
Inventory of Projects
INVENTORY OF PROJECTS PROGRESS REPORT: IMPLEMENTATION OF A PUBLIC HEALTH ACTION PLAN TO COMBAT ANTIMICROBIAL RESISTANCE PROGRESS THROUGH 2007 FOCUS AREA I: SURVEILLANCE ACTION ITEM #1: DETERMINE WHICH ORGANISMS AND SUSCEPTIBILITY TO SPECIFIC ANTIMICROBIAL DRUGS SHOULD BE UNDER SURVEILLANCE AND CREATE A MECHANISM FOR PERIODIC UPDATING OF THIS LIST. PROJECT TITLE: PUBLIC HEALTH SURVEILLANCE • Agency: CDC, USDA, FDA, DoD, VA • Description: Organisms currently under public health surveillance for antimicrobial resistance include: Campylobacter, E. coli O157:H7, Gram negative and Gram positive organisms causing health care associated infections, group A Streptococcus, group B Streptococcus, Haemophilus influenzae, Helicobacter pylori, HIV, Influenza, Malaria, Mycobacterium tuberculosis, Neisseria gonorrhoeae, Neisseria meningitidis, Salmonella, Shigella, Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus pyogenes, Trichomonas vaginalis, and Vancomycin Resistant Enterococcus. Organisms are added to this list when resistance emerges as a public health problem, as tools are developed for detecting resistance, and when there is capacity at the appropriate level. On August 30, 2006, FDA cleared a new test for the detection of vancomycin resistant Enterococci (VRE) by detecting vanA and vanB genes using an automated real-time PCR Instrument. It is indicated for use for patients at risk for VRE colonization. • Results: Ongoing. See Executive Summary and Surveillance Data (to be released following public comment period, summer 2007). PROJECT: CDC ANTIMICROBIAL RESISTANCE SURVEILLANCE ACTIVITIES MEETING • Agency: CDC • Description: The CDC Office of Antimicrobial Resistance, in response to the recently held Antimicrobial Resistance Task Force consultants meeting, convened an internal AR surveillance meeting to explore ways for programs to strengthen and enhance their current surveillance efforts. By sharing successes and failures and exploring potential collaborations, we may be able to increase the impact and utility of our overall surveillance programs.