Triptolide Induces Cell Killing in Multidrug- Resistant Tumor Cells
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Council Declines to Release Report on Allegations School Officials Remember Teen Killed in Wreck
| PAGE LABEL EVEN | FALLOUT CONTINUES T Vol. 116HE No. 331 JOURNALTuesday, November 24, 2020 $100 Tigers’ Swinney T J slams FSU after COMPLEX HISTORY: Thanksgiving lessons jettison Pilgrim hats, welcome truth. B1 Saturday game TRANSITION GREEN LIGHT: Government recognizes Biden as president-elect. D1 postponed. C1 OCONEE COUNTY Council declines to release report on allegations hike in ISO ratings, but Rogers said the county’s county administrator decision to not release ‘This report is Investigation into misconduct claims at Amanda Brock said she the report “gives the didn’t think there should public the idea there is a a public record fire department cost county more than $6K be any concern. Late last coverup.” month, Brock said the “This report is a public and was paid for county’s new ISO data record and was paid for BY RILEY MORNINGSTAR quest for any paperwork investigation in April, as had been completed, was with public funds,” Rog- with public funds. THE JOURNAL relating to the investiga- well as uneasiness inside under review and could ers added. “A public re- tion into the Oconee take up to six months to cord cannot be withheld A public record WALHALLA — Oconee allegations Coun- finalize. in its entirety. They can County Council opted to of sexual ty Fire After executive session redact protected details.” OUR VIEW cannot be withheld leave the results of an in- harass- Commis- at last week’s meeting, TO READ A RELATED vestigation of misconduct ment and sion over county attorney David COUNCIL SPEAKS EDITORIAL, TURN in its entirety. at the Westminster Fire miscon- not being Root asked county coun- Even with the opportu- TO PAGE A4. -

LAW and LEGISLATIVE DIGITAL LIBRARY at the Maine State Law and Legislative Reference Library
MAINE STATE LEGISLATURE The following document is provided by the LAW AND LEGISLATIVE DIGITAL LIBRARY at the Maine State Law and Legislative Reference Library http://legislature.maine.gov/lawlib Reproduced from scanned originals with text recognition applied (searchable text may contain some errors and/or omissions) ONE HUNDRED AND FIRST LEGISLATURE Legislative Document No. 823 H. P. 585 House of Representatives, January 30, 1963 Referred to Committee on Inland Fisheries and Game. Sent up for concur rence and ordered printed. HARVEY R. PEASE, Clerk Presented by Mr. Cookson of Glenburn. STATE OF MAINE IN THE YEAR OF OUR LORD NINETEEN HUNDRED SIXTY-THREE AN ACT Providing for a Bounty on Bears. Be it enacted by the People of the State of Maine, as follows: R. S., c. 37, § 122, additional. Chapter 37 of the Revised Statutes, as revised, is amended by adding a new section 122, to read as follows: 'Sec. 122. Bounty on bears. A bounty of $15 shall be paid for each and every bear killed in organized townships and plantations and unorganized town ships adjoining organized townships and plantations to the person killing the same, by the treasurer of the organized township or plantation in which said bear was killed or the treasurer of any organized township or plantation adjoining the unorganized territory in which said bear was killed. These bounties shall be paid by such treasurers. No bounty shall be paid unless claimant within 72 hours after he has killed such animal exhibits to the town treasurer the entire skin thereof or the entire animal for the killing of which such bounty is claimed, and signs a certificate under oath, which said treasurer may administer, stating that he killed such animal and the time and place within the State. -

Information for the Family and Friends of Homicide Victims
Information for the family and friends of homicide victims “Survivor Tree Oklahoma City Bombing Memorial” Permission to reprint by Jeter Photography Department of Justice Iowa Attorney General’s Office Crime Victim Assistance Division Survivor Tree The photograph on the cover of this guide is of the “Survivor Tree” at the Oklahoma City Bombing Memorial in downtown Oklahoma City, Oklahoma. This American Elm tree survived the bombing of the Alfred P. Murrah Federal Building in Oklahoma City on April 19, 1995. It is now a prominent part of the Oklahoma City National Memorial. The Survivor Tree was nearly chopped down in order to recover evidence from the bombing. It was also severely damaged from the blast and, even though the tree was not chopped down, it was believed it would not survive. Nearly a year after the bombing, the tree was beginning to bloom again. The Survivor Tree is now thriving and is a prominent part of the Memorial. The following is the inscription found in the deck wall around the Survivor Tree: The spirit of this city and this nation will not be defeated; our deeply rooted faith sustains us. The cover photo of the Survivor Tree was chosen as a symbol and tribute to all the survivors of homicide. It represents the strength you demonstrate each day and serves as a reminder of the seed of hope that exists for life after great tragedy and loss. 2 Dear Friends: If you are reviewing this booklet because a loved one has been killed in a homicide, please know that we extend to you our sympathy and support. -
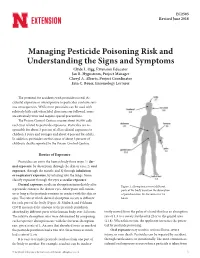
Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L
EC2505 Revised June 2018 Managing Pesticide Poisoning Risk and Understanding the Signs and Symptoms Clyde L. Ogg, Extension Educator Jan R. Hygnstrom, Project Manager Cheryl A. Alberts, Project Coordinator Erin C. Bauer, Entomology Lecturer The potential for accidents with pesticides is real. Ac- cidental exposure or overexposure to pesticides can have seri- ous consequences. While most pesticides can be used with relatively little risk when label directions are followed, some are extremely toxic and require special precautions. The Poison Control Centers receive about 90,000 calls each year related to pesticide exposures. Pesticides are re- sponsible for about 3 percent of all accidental exposures to children 5 years and younger and about 4 percent for adults. In addition, pesticides are the cause of about 3 percent of children’s deaths reported to the Poison Control Centers. Routes of Exposure Pesticides can enter the human body three ways: 1) der- mal exposure, by absorption through the skin or eyes; 2) oral exposure, through the mouth; and 3) through inhalation or respiratory exposure, by inhaling into the lungs. Some classify exposure through the eyes as ocular exposure. Dermal exposure results in absorption immediately after Figure 1. Absorption rates of different a pesticide contacts the skin or eyes. Absorption will contin- parts of the body based on the absorption ue as long as the pesticide remains in contact with the skin or of parathion into the forearm over 24 eyes. The rate at which dermal absorption occurs is different hours. for each part of the body (Figure 1). Maiback and Feldman (1974) measured the amount of the pesticide parathion absorbed by different parts of the human body over 24 hours. -

Boxoffice Barometer (March 26, 1962)
“KING OF KINGS” (70mm Super Technirama Technicolor) Jeffrey Hunter, Siobhan McKenna, Hurt Hatfield, Ron Randell, Viveca Lindfors, Rita Gam, Carmen Sevilla, Brigid Bazlen, Harry Guardino, Rip Torn, Frank Thring, Guy Rolfe, with Maurice Marsac, Gregoire Aslan and Robert Ryan as John the Baptist, with thousands of extras. Presenting an epic story of the life and times of Jesus Christ. A Samuel Bronston Production. “THE FOUR HORSEMEN OF THE APOCALYPSE” ( CinemaScope-Color) Glenn Ford, Ingrid Thulin, Charles Boyer, Lee J. Cobb, Paul Henreid, Paul Lukas, Yvette Mimieux, Karl Boehm. Film ver- sion of the famed Vicente Blasco-Ibanez novel. A Julian Blaustein Production. V f “SWEET BIRD OF YOUTH” ( CinemaScope-Metrocolor) Paul Newman, Geraldine Page, Shirley Knight, Ed Begley, Rip Torn, Mildred “THE HORIZONTAL LIEUTENANT” Dunnock, Madeleine ( CinemaScope- Metrocolor) Sherwood. Film version of Jim Hutton, Paula Prentiss, Jack Carter, Jim the Tennessee Williams Backus, Charles McGraw, Myoshi Umeki. Comedy Broadway stage success. of a U.S. military “clean up” operation on a An Avon Production. Pacific island. A Euterpe Production. ' THROUGH IN 62 ! “MUTINY ON THE BOUNTY” ( Ultra Panavision- Metrocolor) Marlon Brando, Trevor Howard, Richard Harris, Hugh Griffith, Richard Hayden and Tarita. Spectacular sea adventure drama, based on trilogy of novels by Charles Nordoff and James Norman Hall. Filmed in the South Seas and on a replica of the great three masted sailing ship, HMS Bounty. An Areola Pictures Production. “A VERY PRIVATE AFFAIR” {Color) Brigitte Bardot and Marcello Mastroianni. Story of a French girl who achieves fame as a screen star. A Progefi- Cipra Production. “ALL FALL DOWN” Lva Marie Saint, Warren Beatty, Karl dalden, Lansbury, ! Angela Brandon deWilde. -

Ex-Militants Who Admit Killing Cops Seek Parole
c Official Publication Of The c SAN FRANCISCO POLICE OFFICERS ASSOCIATION This Publication was Produced and Printed in California, USA ✯ Buy American ✯ Support Local Business VOLUME 46, NUMBER 3 SAN FRANCISCO, MARCH 2014 www.sfpoa.org These are allegations. Few of Take the POA Online Survey the“ facts — or their questionable First Week of March sources — have been fully From March 3rd through March 7th, the POA will be conducting an online disclosed. I am convinced of the Members Survey. It will be an opportunity for you to express your opinions integrity and dedication of each and provide the POA with valuable feedback. of these officers, and they are all You will receive an e-mail from the POA directing you to the ‘Members innocent until proven guilty. The Only’ section of the website, SFPOA.org. There, you will be asked to complete full resources of the San Francisco a brief survey of up to 10 questions. Participants will remain anonymous, but we will ask for your current assignment and years of service (both with Police Officers Association will the SFPD and other law enforcement). be used to defend these officers We have many members who have provided the POA with a current e- and restore their careers and mail address. Please send an e-mail to Cyndee Bates (POA Office Manager) reputations. or me so that we can ensure you receive notice of this important survey: [email protected] or [email protected]. — Martin” Halloran, President At the completion of the survey we will share the results. — Mike Nevin, Secretary SFPOA Press Release Ingleside Station Attackers February 27, 2014 SFPOA President Disappointed Ex-Militants Who Admit with Indictments San Francisco Police Officers Association President, Martin Halloran today Killing Cops Seek Parole expressed disappointment at the indictment of the current San Francisco Forwarded to the Journal a militant black power group serving Police Officers by a Federal Grand Jury. -

WHO Guidelines on Drawing Blood Best Practices in Phlebotomy (Eng)
WHO guidelines on drawing blood: best practices in phlebotomy WHO Library Cataloguing-in-Publication Data WHO guidelines on drawing blood: best practices in phlebotomy. 1.Bloodletting – standards. 2.Phlebotomy – standards. 3.Needlestick injuries – prevention and control. 4.Guidelines. I.World Health Organization. ISBN 978 92 4 159922 1 (NLM classification: WB 381) © World Health Organization 2010 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. -

107 Civilians Killed, Including 34 Children, in the First 72 Hours Following Security Council Resolution 2401
107 Civilians Killed, including 34 Children, in the First 72 Hours Following Security Council Resolution 2401 Most Notable Violations of Security Council Resolution 2401 in Three Days Wednesday, February 28, 2018 1 snhr [email protected] www.sn4hr.org The Syrian Network for Human Rights (SNHR), founded in June 2011, is a non-governmental, independent group that is considered a primary source for the OHCHR on all death toll-related analyses in Syria. Contents I. Introduction and Report Methodology II. Executive Summary III. Details IV. Conclusions and Recommendations I. Introduction and Methodology Security Council resolution 2041 comes at a time when the Security Council’s impact in the Syrian catastrophe had reached extreme degrees of passivity and impotence. Even though the Security Council has adopted 18 resolutions on Syria so far, these resolutions are mere words, including the ones that include warning phrases and threaten to take pu- nitive measures in the event of non-compliance, such as resolution 2139 on the cease of barrel bomb use, as well as resolutions 2118, 2209, and 2235 that addressed the repeated use of chemical weapons and have been violated hundreds of times by the Syrian regime, as the Security Council is still standing idly by under Russia’s thumb. No real progress has been seen in the case of resolution 2401 that was adopted in the form of weak, non-binding phrases, without addressing any penal specifics or consequences in the event of non-compliance. A resolution like this was a greenlight to the Syrian regime and its allies to continue the killing and bombardment, as nothing has happened, where the heavy and indiscriminate bombardment was resumed merely a few hours after the res- olution was adopted. -

Law Enforcement Response to Domestic Violence and Sexual Assault
Law Enforcement Response to Domestic Violence and Sexual Assault This project was supported by Grant No. 2008-WF-AX- 0007 awarded by the Office on Violence Against Women, U.S. Department of Justice. The opinions, findings, conclusions, and recommendations expressed in this publication are those of the author and do not necessarily reflect the views of the Department of Justice, Office of Violence Against Women. Revised November 2014 1 2 Table of Contents Domestic Violence Section Domestic Violence Introduction 5 Chapter 1 Arrest & Establishing Probable Cause 7 Chapter 2 Writing Reports and Collecting Evidence 13 Chapter 3 Enforcement of Protection Orders 16 Chapter 4 Officer Liability 26 Chapter 5 Officers’ Attitudes Influence Their Actions 28 Chapter 6 Abuser Profiles 29 Chapter 7 Victim Responses/Dynamics of Battering 34 Chapter 8 Victim Rights 43 Chapter 9 SD Codified Laws Regarding Domestic Violence 50 Chapter 10 Domestic Violence Investigation Checklist 81 3 Sexual Assault Section Sexual Assault Introduction The Truth about Sexual Assault 102 Chapter 11 Sexual Assault Response Team 104 Chapter 12 Building Your Case 109 Chapter 13 Report Writing 120 Chapter 14 Victim Initial Response and Post-Assault Response 124 Chapter 15 Victim Rights and Support Services 128 Chapter 16 Delayed Reporting 135 Chapter 17 Drug Facilitated Sexual Assault 137 Chapter 18 SD Codified Laws Regarding Sexual Assault 142 Chapter 19 Sexual Assault Glossary of Terms 148 Chapter 20 Sexual Assault Investigation Checklist 151 Appendix: Shelters and Service Programs 154 4 Domestic Violence Introduction “Domestic violence (DV) is not a law enforcement problem.” That’s what one veteran officer once said during a training session.