Pdf/2015/Births.Pdf Similarly, Delay in Penetration of Screening Guidelines to 11
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heatwave Guide for Cities
HEATWAVE GUIDE FOR CITIES HEATWAVE GUIDE FOR CITIES 2 HEATWAVE GUIDE FOR CITIES Heatwaves are deadly and their impacts are on the rise globally due to climate change. But this is not inevitable; it is up to us to prevent this public-health crisis from impacting our neighbours, family members and friends. Every year, heatwaves claim the lives of infants, older people, and people with chronic health conditions. The urban poor frequently bear the brunt of this silent emergency. In addition to threatening the lives and health of vulnerable popula- tions, heatwaves have cascading impacts in other areas of society, such as reduced economic output, strained health systems and rolling power outages. The Lancet estimates that in 2017, 153 billion hours of work were lost due to extreme heat. What is unacceptable about this silent emergency is that simple, low-cost actions such as ordinary citizens checking on vulnerable neighbours can save lives during episodes of extreme heat. As many as 5 billion people live in areas of the world where heatwaves can be forecast before they happen, which means we have time to take early action to save lives. To address the existing need and reduce future risks posed by climate change, we need collective global action to scale up early warning systems for heat. People living in urban areas are amongst the hardest hit when a heatwave occurs because these are hotter than the surrounding countryside. Along with climate change, urbanization is one of the most transformative trends of this century and the last. Over half the world now lives in urban areas and this is projected to increase to two-thirds by 2050. -
2015 World First Aid Day Global Activity Report
2015 WORLD FIRST AID DAY GLOBAL ACTIVITY REPORT Introduction IFRC has been the world’s leading first aid trainer and provider for more than 100 years. In 2014, more than 15 million people were trained worldwide by National Societies. By aiming to equip many more millions of people with lifesaving skills worldwide, we can ensure, notably through the World First Aid Day, that first aid gains the attention and support it deserves as part of a broader resilience approach. World First Aid Day (WFAD) is a time to promote first aid as a lifesaving skill around the globe and ensure that a growing number of people and communities, anywhere, are prepared and equipped to save lives when a disaster or an emergency occurs. In 2015 WFAD was celebrated on Saturday 12 September, with the theme “first aid and ageing population”. The aim was to build a positive image of ageing and recognizing older people as an important resource. We believe that older people can be transformed from being cared for into people providing quality integrated care. We are advocating for empowering older people with life-saving skills. Older people trained in first aid means they can take swift and effective action to reduce serious injuries, spot early warning signs for non- communicable diseases such as strokes. Neither cape nor superpowers are needed to be a hero: “Be a hero. Save lives. First aid is for everyone, everywhere.” As in previous years IFRC provided some support through visual and communication tools to help National Societies promote WFAD. A communication toolkit was available on Fed Net: https://fednet.ifrc.org/wfad2015 and included: key messages first aid training for older people resource packs web banners infographics social media tips and guidelines My Story – an active first aid tag on the site (http://ifrc.tumblr.com/tagged/first-aid) to collect volunteer and beneficiary stories around first aid. -

Iso/Ts 13399-5:2014
PD ISO/TS 13399-5:2014 BSI Standards Publication Cutting tool data representation and exchange Part 5: Reference dictionary for assembly items PD ISO/TS 13399-5:2014 PUBLISHED DOCUMENT National foreword This Published Document is the UK implementation of ISO/TS 13399-5:2014. The UK participation in its preparation was entrusted to Technical Committee MTE/18, Tools tips and inserts for cutting applications. A list of organizations represented on this committee can be obtained on request to its secretary. This publication does not purport to include all the necessary provisions of a contract. Users are responsible for its correct application. © The British Standards Institution 2014. Published by BSI Standards Limited 2014 ISBN 978 0 580 82713 6 ICS 25.100.01; 35.240.50 Compliance with a British Standard cannot confer immunity from legal obligations. This Published Document was published under the authority of the Standards Policy and Strategy Committee on 31 March 2014. Amendments/corrigenda issued since publication Date Text affected PD ISO/TS 13399-5:2014 TECHNICAL ISO/TS SPECIFICATION 13399-5 Second edition 2014-02-15 Cutting tool data representation and exchange — Part 5: Reference dictionary for assembly items Représentation et échange des données relatives aux outils coupants — Partie 5: Dictionnaire de référence de termes pour les éléments d’assemblage Reference number ISO/TS 13399-5:2014(E) © ISO 2014 PD ISO/TS 13399-5:2014 ISO/TS 13399-5:2014(E) COPYRIGHT PROTECTED DOCUMENT © ISO 2014 All rights reserved. Unless otherwise specified, no part of this publication may be reproduced or utilized otherwise in any form orthe by requester. -

Digital Twin-Driven Smart Manufacturing: Connotation, Reference Model, Applications and Research Issues
Digital twin-driven smart manufacturing: Connotation, reference model, applications and research issues Yuqian Lu a, Chao Liu b, Kevin I-Kai Wang c, Huiyue Huang a, Xun Xu a,* a Department of Mechanical Engineering, The University of Auckland, New Zealand b School of Engineering, Cardiff University, United Kingdom c Department of Electrical, Computer and Software Engineering, The University of Auckland, New Zealand * Corresponding author: Tel.: +64 9 923 4527; E-mail address: [email protected] ABSTRACT This paper reviews the recent development of Digital Twin technologies in manufacturing systems and processes, to analyze the connotation, application scenarios, and research issues of Digital Twin-driven smart manufacturing in the context of Industry 4.0. To understand Digital Twin and its future potential in manufacturing, we summarized the definition and state-of-the- art development outcomes of Digital Twin. Existing technologies for developing a Digital Twin for smart manufacturing are reviewed under a Digital Twin reference model to systematize the development methodology for Digital Twin. Representative applications are reviewed with a focus on the alignment with the proposed reference model. Outstanding research issues of developing Digital Twins for smart manufacturing are identified at the end of the paper. Keywords : Smart Manufacturing; Digital Twin; Industry 4.0; Cyber-physical System; Big Data; Standard; Industrial Communication Y. Lu, C, Liu, K, Wang, H, Huang, X. Xu, Digital twin-driven smart manufacturing: Connotation, reference model, applications and research issues, Robot. Comput. Integr. Manuf. 1 Introduction Digital Twin has gained significant impetus as a breakthrough technological development that has the potential to transform the landscape of manufacturing today and tomorrow [1]. -
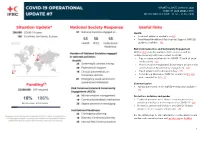
EP-2020-000012-CHN OPERATION TIMEFRAME: 31 Jan - 31 Dec 2020
REPORTING DATE: 20 March 2020 GLIDE: EP-2020-000012-CHN OPERATION TIMEFRAME: 31 Jan - 31 Dec 2020 Health • Technical guidance available on GO • New Mental Health and Psychosocial Support (MHPSS) guidance available - EN Risk Communication and Community Engagement Online table includes available RCCE resources and be updated regularly with new content and links. o Tips on using social media for COVID-19 (with all social media assets) - EN o How to include marginalized & vulnerable people in risk communication & community engagement - EN o Rapid assessment tools: rapid survey - EN o Focus Group Discussion (FGD) for volunteers (EN, FR) and communities (EN, FR) Communication • Media statements on the COVID-19 response available - EN Protection, inclusion and gender • Technical guidance note: How to consider protection, gender and inclusion in the response to COVID-19 - EN • Protection, gender and inclusion and COVID-19 basic guidance (key messages and groups) - EN For the detailed up-to-date information on the situation and guidance documents please visit go.ifrc.org or FedNet. 1 OPERATIONAL UPDATE The Emergency Plans of Actions for COVID-19 operation are available here. Red Cross and Red Crescent activities globally Health (including MHPSS) The IFRC, in close collaboration with global and local health partners, is continuing to provide risk assessment and guidance to support National Societies to implement high-quality, effective and appropriate epidemic response, social support and epidemic impact mitigation activities. In the last week, along with various National Societies and external partners, IFRC attended a webinar which focused on sharing experiences between countries and organizations working in prehospital and intensive care service provision. -

Organisation 28. Jun 350.Org Able Child Africa Abraham Law & Consulting Abzesolar S.A
Organisation 28. Jun 350.org Able Child Africa Abraham Law & Consulting AbzeSolar S.A. Academic Council on the United Nations System (ACUNS) Academy of Philanthropy ACAPS Agency Coordinating Body for Afghan Relief and Development (ACBAR) Accenture Access2innovation ACT Alliance Act for Peace Agence d'Aide à la Coopération Technique et au Développement (ACTED) Action 24 Action Africa Help International (AAH-I) Action Against Hunger - ACF International ActionAid International Active Learning Network for Accountability and Performance (ALNAP) Agence de Développement Economique et Social (ADES) African Development Solutions - Southern Non Governmental Organisations Network (ADESO - SNGO Network) A Demand For Action (AFDA) Adventist Relief and Development Agency (ADRA) Afghan Institute of Learning Afghan Landmine Survivors' Organization Afghan Red Crescent Afghanaid Afghanistan Independent Human Rights Commission Africa Humanitarian Action Africa Scout Foundation Africa Solidarity Network (ASONET) African Centre for Disaster Studies, North West University African Centre of Meteorological Application for Development (ACMAD) African Clean Energy African Development Trust (ADT) African Disability Forum African Foundation for Development African Risk Capacity Agency African Technology Foundation African Union Afrique Secours et Assistance (ASA) Agence d'Assistance aux Rapatriés et Réfugiés au Congo (AARREC) Agility Agir Ensemble pour le Tchad Asian Coordinating Center for Humanitarian Assistance (AHA Center) Ahmadu Bello University, Zaria, Kaduna -

Hand in Hand a Collection of Disaster Risk Reduction Success Stories Hand in Hand a Collection of Disaster Risk Reduction Success Stories RC/RC Movement in Indonesia
Hand in Hand A Collection of Disaster Risk Reduction Success Stories Hand in Hand A Collection of Disaster Risk Reduction Success Stories RC/RC Movement in Indonesia The international Committee of the Red Cross (ICRC) - is an impartial, neutral and independent organization whose exclusively All rights reserved. Except for quotation in a review of the work, no part of this publication may be reproduced, stored in a retrieval system, or humanitarian mission is to protect the lives and dignity of victims of war and internal violence and to provide them with assistance. transmitted, in any form or by any means, electronic, photocopying, recording or otherwise without the prior permission of the Indonesian Red Cross It directs and coordinates the international relief activities conducted by the Movement in situations of conflict. It also endeavors to and International Federation of Red Cross and Red Crescent Societies Indonesia Delegation. This publication is copyright, but maybe reproduced without fee for teaching purpose but not for resale prevent suffering by promoting and strengthening humanitarian law and universal humanitarian principles. Established in 1863, the ICRC is at the origin of the International Red Cross and Red Crescent Movement We would like to thank all those who assisted during the publication for this issue The International Federation of Red Cross and Red Crescent Societies (IFRC) is the world’s largest humanitarian organization, Production Managers: providing assistance without discrimination as to nationality, race, religious beliefs, class or political opinions. The International Anggun Permana Sidiq, Arifin Muh. Hadi, Bevita Dwi Meidityawati, Indra Yogasara Federation’s mission is to improve the lives of vulnerable people by mobilizing the power of humanity. -

Industrial Automation
ISO Focus The Magazine of the International Organization for Standardization Volume 4, No. 12, December 2007, ISSN 1729-8709 Industrial automation • Volvo’s use of ISO standards • A new generation of watches Contents 1 Comment Alain Digeon, Chair of ISO/TC 184, Industrial automation systems and integration, starting January 2008 2 World Scene Highlights of events from around the world 3 ISO Scene Highlights of news and developments from ISO members 4 Guest View ISO Focus is published 11 times Katarina Lindström, Senior Vice-President, a year (single issue : July-August). It is available in English. Head of Manufacturing in Volvo Powertrain and Chairman of the Manufacturing, Key Technology Committee Annual subscription 158 Swiss Francs Individual copies 16 Swiss Francs 8 Main Focus Publisher • Product data – ISO Central Secretariat Managing (International Organization for information through Standardization) the lifecycle 1, ch. de la Voie-Creuse CH-1211 Genève 20 • Practical business Switzerland solutions for ontology Telephone + 41 22 749 01 11 data exchange Fax + 41 22 733 34 30 • Modelling the E-mail [email protected] manufacturing enterprise Web www.iso.org • Improving productivity Manager : Roger Frost with interoperability Editor : Elizabeth Gasiorowski-Denis • Towards integrated Assistant Editor : Maria Lazarte manufacturing solutions Artwork : Pascal Krieger and • A new model for machine data transfer Pierre Granier • The revolution in engineering drawings – Product definition ISO Update : Dominique Chevaux data sets Subscription enquiries : Sonia Rosas Friot • A new era for cutting tools ISO Central Secretariat • Robots – In industry and beyond Telephone + 41 22 749 03 36 Fax + 41 22 749 09 47 37 Developments and Initiatives E-mail [email protected] • A new generation of watches to meet consumer expectations © ISO, 2007. -

Six Months Report Ecuador: Earthquake
Six months report Ecuador: Earthquake Emergency appeal n° MDREC012 GLIDE n° EQ-2016-000035-ECU Six months report Timeframe covered by this update: 22 April to 16 October 2016 Emergency Appeal operation start date: 22 April 2016 Timeframe: 16 months (ends on 21 August 2017) Appeal budget: Appeal Total estimated Red Cross and Red Crescent 15,085,628 Swiss Francs coverage: response to date: CHF 7,524,462 Swiss francs 56% Disaster Relief Emergency Fund (DREF) allocated: 405,778 Swiss francs N° of people being assisted: 85,324 people (21,331 families) Host National Society presence: The Ecuadorian Red Cross (ERC) has a national headquarters in Quito, 24 provincial boards, 110 local branches 200 staff members and for this operation has mobilized 765 volunteers. Red Cross Red Crescent Movement partners actively involved in the operation: American Red Cross, British Red Cross, Canadian Red Cross Society, Colombian Red Cross Society, Red Crescent Society of the Islamic Republic of Iran, Mexican Red Cross Society, Norwegian Red Cross Society, Philippines Red Cross, Salvadorian Red Cross Society Spanish Red Cross, the International Committee of the Red Cross (ICRC) and the International Federation of Red Cross and Red Crescent Societies (IFRC). Red Cross Red Crescent Movement partners supporting this operation: American Red Cross, British Red Cross, Canadian Red Cross Society, Finnish Red Cross, German Red Cross, Honduran Red Cross, Hong Kong Red Cross, Japanese Red Cross Society, Republic of Korea National Red Cross, Macau Red Cross, Netherlands Red Cross (with government of the Netherlands funds), Norwegian Red Cross, Peruvian Red Cross, Swedish Red Cross (with Swedish government funds) and Swiss Red Cross. -

Haemochromatosis and Blood Donation
Haemochromatosis and blood donation -Philippe Vandekerckhove Rode Kruis Introduction: haemochromatosis hereditary disorder of the iron metabolism affecting predominantly people of Northern European origin − survival advantage in regions with iron-poor diets − mutations spread by migratory activities of Vikings requiring frequent phlebotomies to normalise serum iron levels Merryweather-Clarke A. 2000 Introduction: haemochromatosis Currently no consensus on using the blood from carriers with a documented mutation and/or patients as blood donor for red cell transfusion Issues are: − Can the donation be considered voluntary ? − Is this blood safe for transfusion? Questions addressed Question 1: What is the current policy in different countries with a primarily Caucasian population? Question 2: Is blood of uncomplicated haemochromatosis patients safe and effective for blood transfusion? QUESTION 1 What is the current policy in different countries with a primarily Caucasian population? Methodology & Results Cross-sectional survey − Using a web-based questionnaire (SurveyMonkey® software) − 8 questions on current policy concerning haemochromatosis patients and blood donation − Respondents: • representatives of of the European Blood Alliance (EBA) and/or Alliance of Blood Operators (ABO) • 44 representatives of blood services in 41 countries Response rate − 80 % − 35 respondents representing blood services in 33 countries (next slide) Methodology: participants Last name and first name of Country Affiliation Last name and first name of -

Typhoon Haiyan: One Month Later Donor Report Typhn Oo Haiyan: One Month Later | Donor Report
Friday November 8, 2013, Typhoon On Haiyan – locally known as Yolanda – created widespread destruction across the Philippines, affecting 11.2 million people, leaving lives and homes destroyed. Despite the many typhoons to hit the Philippines in the past, Haiyan has created more dev- astation than any other. In its wake, it has left 4.1 million people displaced and after one month, urgent, life-saving emergency services continue to be required in the form of food, clean water, health and emergency shelter. TYPHOON HAIYAN: ONE MONTH LATER Donor Report TYPHN OO HAIYAN: onE MONTH LATER | DONOR REPORT Red Cross Response By The Numbers Over $24 million raised by the Canadian Red Cross 615,305 people have received over 123,000 Red Cross food packages 55,300 people reached with health and hygiene promotion 32,000 Family reunification cases responded to 29,202 hot meals distributed 17,889 people reached with psychosocial support 6,233 Red Cross volunteers mobilized 11,777 people reached with medical support 12 International Emergency Response Units deployed 2 Basic Healthcare Units operational, one of which is the Canadian Red Cross field hospital The Canadian Red Cross field hospital has performed44 surgeries and has delivered over 150 babies since opening,including 21 life-saving caesarean sections. TYPHoon HAIYAN: ONE MontH LATER | DONOR REPORT The International The Canadian Red Red Cross & Cross Response Red Crescent Shortly after the devastating typhoon made landfall in the Philippines, the Canadian Red Cross deployed its Response emergency field hospital along with 28 highly trained personnel. This hospital can be set up quickly and Immediately following the disaster, Red Cross cover the health needs of a population of more than volunteers in the Philippines and across affected 100,000 people. -

Rfl Strategy Implementation Group / Groupe De Mise En Oeuvre Rlf / Grupo De Aplicación Rcf
RFL STRATEGY IMPLEMENTATION GROUP / GROUPE DE MISE EN OEUVRE RLF / GRUPO DE APLICACIÓN RCF The RFL Strategy Implementation Group is comprised of members from the National Societies of Australia, Canada, China, RD Congo, Colombia, Côte d’Ivoire, Germany, Honduras, Indonesia, Iran, Iraq, Mexico, The Netherlands, Saudi Arabia, Senegal, Sweden, Uganda, Ukraine, the United States and the United Kingdom, as well as the International Federation and the ICRC. It provides guidance and support in the implementation process of the RFL Strategy for the Movement (2008-2018). Le Groupe de mise en œuvre de la Stratégie RLF est composé de membres de la Fédération internationale, du CICR et des Sociétés nationales des pays suivants : Allemagne, Arabie Saoudite, Australie, Canada, Chine, Colombie, République démocratique du Congo, Côte d’Ivoire, États- Unis, Honduras, Indonésie, Iran, Irak, Mexique, Ouganda, Pays-Bas, Royaume-Uni, Sénégal, Suède et Ukraine. Il est chargé de guider et de soutenir le processus de mise en œuvre de la Stratégie de RLF pour le Mouvement (2008-2018). El Grupo de Aplicación de la Estrategia relativa al RCF, integrado por representantes de las Sociedades Nacionales de Alemania, Arabia Saudita, Australia, Canadá, China, RD Congo, Colombia, Costa de Marfil, los Estados Unidos, Honduras, Indonesia, Irak, Irán, México, Países Bajos, el Reino Unido, Senegal, Suecia, Uganda y Ucrania, así como de la Federación Internacional y del CICR, presta orientación y apoyo en el proceso de aplicación de la Estrategia del Movimiento relativa al