A System for Monitoring Breathing Activity Using an Ultrasonic Radar Detection with Low Power Consumption
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -
Emergency Nursing Program Foreword
RESOURCE MANUAL NSW HEALTH 2011 Transition to Practice Emergency Nursing Program Foreword The role of emergency nurses requires a broad level of skill and ability to meet the care needs of patients and their families. The Transition to Emergency Nursing Program is designed to support registered nurses new to the practice of emergency nursing. The Emergency Department is a fast-moving environment within which nurses can find themselves faced with a variety of challenges across a day. This program will assist them as they develop their knowledge and skills to meet these often changing care needs within the emergency setting. The program also supports a more consistent approach to transition to emergency nursing and it is anticipated will become the standard for initial entry to practice as an emergency nurse across NSW. This Resource Manual is the core document for the program and is complemented by both the Participant Workbook and the Facilitator’s Manual. Within the Emergency Department participants will be supported by staff to meet the relevant learning objectives during the 3-6 months over which this program extends. The development of the Transition to Emergency Nursing Program has been a lengthy process which reflects the commitment of emergency nurses to their area of practice and I acknowledge and thank them for their enthusiasm and work in enabling the Program to be developed. I am sure that it will have a positive impact for those nurses new to emergency nursing and to the care of patients. 1 Adjunct Professor Debra Thoms Chief Nursing and Midwifery Officer NSW Health NSW Department of Health 73 Miller Street NORTH SYDNEY NSW 2060 Tel. -

Lesson 1 ELECTROMYOGRAPHY 1 Motor Unit Recruitment
Physiology Lessons for use with the Biopac Science Lab MP40 Lesson 12 Respiration 1 Apnea PC running Windows® XP or Mac® OS X 10.3-10.4 Lesson Revision 3.15.2006 BIOPAC Systems, Inc. 42 Aero Camino, Goleta, CA 93117 (805) 685-0066, Fax (805) 685-0067 [email protected] www.biopac.com © BIOPAC Systems, Inc. 2006 Page 2 Biopac Science Lab Lesson 12 The Respiratory Cycle I. SCIENTIFIC PRINCIPLES All body cells require oxygen for metabolism and produce carbon dioxide as a metabolic waste product. The respiratory system supplies oxygen to the blood for delivery to cells, and removes carbon dioxide added to the blood by the cells. Cyclically breathing in and out while simultaneously circulating blood between the lungs and other body tissues facilitates the exchange of oxygen and carbon dioxide between the body and the external environment. This process serves cells by maintaining rates of oxygen delivery and carbon dioxide removal adequate to meet the cells’ metabolic needs. The breathing cycle, or respiratory cycle, consists of inspiration during which new air containing oxygen is inhaled, followed by expiration during which old air containing carbon dioxide is exhaled. Average adult people at rest breathe at a frequency of 12 to 15 breaths per minute (BPM), and with each cycle, move an equal volume of air, called tidal volume (TV), into and back out of the lungs. The actual value of tidal volume varies in direct proportion to the depth of inspiration. During normal, quiet, unlabored breathing (eupnea) at rest, adult tidal volume is about 450 ml to 500 ml. -

Design of Respiration Rate Meter Using Flexible Sensor
JEEMI, Vol. 2, No. 1, January 2020, pp: 13-18 DOI: 10.35882/jeeemi.v2i1.3 ISSN:2656-8632 Design of Respiration Rate Meter Using Flexible Sensor Sarah Aghnia Miyagi#,1, Muhammad Ridha Mak’ruf1, Endang Dian Setyoningsih1, Tarak Das2 1Department of Electromedical Engineering Poltekkes Kemenkes, Surabaya Jl. Pucang Jajar Timur No. 10, Surabaya, 60245, Indonesia 2Department of Biomedical Engineering Netaji Subhash, Engineering College Kolkata, India #[email protected], [email protected], [email protected], [email protected] Abstract— Respiration rate is an important physiological parameter that helps to provide important information about the patient's health status, especially from the human respiratory system. So it is necessary to measure the human respiratory rate by calculating the number of respiratory frequencies within 1 minute. The respiratory rate meter is a tool used to calculate the respiratory rate by counting the number of breaths for 1 minute. The author makes a tool to detect human respiratory rate by using a sensor that detects the ascend and descend of the chest cavity based on a microcontroller so that the operator can measure the breathing rate more practically and accurately. Component tool contains analog signal conditioning circuit and microcontroller circuit accompanied by display in the form of LCD TFT. The results of measurement data on 10 respondents obtained an average error value, namely the position of the right chest cavity 6.6%, middle chest cavity 7.92%, and left chest cavity 6.85%. This value is still below the error tolerance limit of 10%. It can be concluded that to obtain the best measurement results, the sensor is placed in the position of the right chest cavity. -
Chapter 22 *Lecture Powerpoint
Chapter 22 *Lecture PowerPoint The Respiratory System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Breathing represents life! – First breath of a newborn baby – Last gasp of a dying person • All body processes directly or indirectly require ATP – ATP synthesis requires oxygen and produces carbon dioxide – Drives the need to breathe to take in oxygen, and eliminate carbon dioxide 22-2 Anatomy of the Respiratory System • Expected Learning Outcomes – State the functions of the respiratory system – Name and describe the organs of this system – Trace the flow of air from the nose to the pulmonary alveoli – Relate the function of any portion of the respiratory tract to its gross and microscopic anatomy 22-3 Anatomy of the Respiratory System • The respiratory system consists of a system of tubes that delivers air to the lung – Oxygen diffuses into the blood, and carbon dioxide diffuses out • Respiratory and cardiovascular systems work together to deliver oxygen to the tissues and remove carbon dioxide – Considered jointly as cardiopulmonary system – Disorders of lungs directly effect the heart and vice versa • Respiratory system and the urinary system collaborate to regulate the body’s acid–base balance 22-4 Anatomy of the Respiratory System • Respiration has three meanings – Ventilation of the lungs (breathing) – The exchange of gases between the air and blood, and between blood and the tissue fluid – The use of oxygen in cellular metabolism 22-5 Anatomy of the Respiratory System • Functions – Provides O2 and CO2 exchange between blood and air – Serves for speech and other vocalizations – Provides the sense of smell – Affects pH of body fluids by eliminating CO2 22-6 Anatomy of the Respiratory System Cont. -

Vitals & Assessment Bingo
Vitals & Assessment Bingo myfreebingocards.com Safety First! Before you print all your bingo cards, please print a test page to check they come out the right size and color. Your bingo cards start on Page 3 of this PDF. If your bingo cards have words then please check the spelling carefully. If you need to make any changes go to mfbc.us/e/dtfgtk Play Once you've checked they are printing correctly, print off your bingo cards and start playing! On the next page you will find the "Bingo Caller's Card" - this is used to call the bingo and keep track of which words have been called. Your bingo cards start on Page 3. Virtual Bingo Please do not try to split this PDF into individual bingo cards to send out to players. We have tools on our site to send out links to individual bingo cards. For help go to myfreebingocards.com/virtual-bingo. Help If you're having trouble printing your bingo cards or using the bingo card generator then please go to https://myfreebingocards.com/faq where you will find solutions to most common problems. Share Pin these bingo cards on Pinterest, share on Facebook, or post this link: mfbc.us/s/dtfgtk Edit and Create To add more words or make changes to this set of bingo cards go to mfbc.us/e/dtfgtk Go to myfreebingocards.com/bingo-card-generator to create a new set of bingo cards. Legal The terms of use for these printable bingo cards can be found at myfreebingocards.com/terms. -

Respiratory Failure
Respiratory Failure Phuong Vo, MD,* Virginia S. Kharasch, MD† *Division of Pediatric Pulmonary and Allergy, Boston Medical Center, Boston, MA †Division of Respiratory Diseases, Boston Children’s Hospital, Boston, MA Practice Gap The primary cause of cardiopulmonary arrest in children is unrecognized respiratory failure. Clinicians must recognize respiratory failure in its early stage of presentation and know the appropriate clinical interventions. Objectives After completing this article, readers should be able to: 1. Recognize the clinical parameters of respiratory failure. 2. Describe the respiratory developmental differences between children and adults. 3. List the clinical causes of respiratory failure. 4. Review the pathophysiologic mechanisms of respiratory failure. 5. Evaluate and diagnose respiratory failure. 6. Discuss the various clinical interventions for respiratory failure. WHAT IS RESPIRATORY FAILURE? Respiratory failure is a condition in which the respiratory system fails in oxy- genation or carbon dioxide elimination or both. There are 2 types of impaired gas exchange: (1) hypoxemic respiratory failure, which is a result of lung failure, and (2) hypercapnic respiratory failure, which is a result of respiratory pump failure (Figure 1). (1)(2) In hypoxemic respiratory failure, ventilation-perfusion (V_ =Q)_ mismatch results in the decrease of PaO2) to below 60 mm Hg with normal or low PaCO2. _ = _ (1) In hypercapnic respiratory failure, V Q mismatch results in the increase of AUTHOR DISCLOSURE Drs Vo and Kharasch fi PaCO2 to above 50 mm Hg. Either hypoxemic or hypercapnic respiratory failure have disclosed no nancial relationships can be acute or chronic. Acute respiratory failure develops in minutes to hours, relevant to this article. -

Respiratory System
Respiratory System Course Rationale Anatomy & To pursue a career in health care, proficiency in anatomy and physiology is Physiology vital. Unit XIII Objectives Respiratory Upon completion of this lesson, the student will be able to: System • Describe biological and chemical processes that maintain homeostasis • Analyze forces and the effects of movement, torque, tension, and Essential elasticity on the human body Question • Define and decipher terms pertaining to the respiratory system How long can • Distinguish between the major organs of the respiratory system the body be • Analyze diseases and disorders of the respiratory system without • Label a diagram of the respiratory system oxygen? Engage TEKS Perform the following in front of the class using a paper towel and a hand 130.206 (c) mirror: 1 (A)(B) • Use the paper towel to clean and dry the mirror. 2(A)(D) • Hold the mirror near, but not touching, your mouth. 3 (A)(B)(E) • Exhale onto the mirror two or three times. 5 (B)(C)(D) • Examine the surface of the mirror. 6 (B) What happens to the mirror? 8 (A)(B)(C) Why does the mirror become fogged? 9 (A)(B) 10 (A)(B)(C) Or Prior Student Of all the substances the body must have to survive, oxygen is by far the most Learning critical. Think about the following: Cardiovascular system – • Without food - live a few weeks Pulmonary • Without water - live a few days Circulation • Without oxygen - live 4 – 6 minutes Estimated time 4 - 6 hours Key Points 1. Introduction – Respiratory System A. General Functions *Teacher note: 1. Brings oxygenated air to the alveoli invite a 2. -

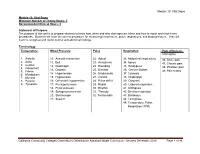
Chest Exam Codes Code Description 1 1800 Tachypnea 2 1801 H
Jan-07 Fernald Medical Monitoring Program Sort Code Physician Exam - Chest Exam Codes Code Description 1 1800 tachypnea 2 1801 hyperpnea 3 1802 hyperventilation 4 1803 bradypnea 5 1804 Cheyne-Stokes breathing 6 1805 ataxic breathing 7 1806 sighing respiration 8 1807 pursed lip breathing 9 1875 Prolong expiration 10 1808 Dyspneic or dyspnea-short of breath 11 1886 PT on 02 12 1809 chronic cough 13 14 1892 Upper Airway Tightness 15 1889 Respiratory Distress 16 1888 Orthopnea (difficulty breathing while lying down) 17 1885 Chest burning 18 1884 Clavicle deformity/Prominence 19 1882 Rib pain 20 1881 Chest tightness 21 1869 Abnormal Lung exam 22 23 1810 barrel chest 24 1811 funnel chest 25 1855 pectus excavatum 26 1835 Pigeon chest/pectus casrinatum 27 1839 chest wall discomfort/tenderness 28 1812 intercostal retraction 29 1813 tender pectoral muslces 30 1814 tender costal cartilages 31 1848 missing rib 32 1837 slightly protruding xyphoid tip, rib cage 33 1859 Prominent bone, sternum 34 35 1815 (Fatty-like)mass on chest 36 1816 kyphosis 37 1831 scoliosis 38 1872 poor posture 39 1817 increased AP diameter 40 1874 decreased AP diameter 41 pacemaker generator in place/ 1818 defibrillator 42 1819 Hickman catheter in precordium port-a-cath 43 44 1820 Faint/few breath sounds 45 1838 Using accessory muscles to breathe 46 1844 decreased breath sounds 47 1838 small lung volume 48 1821 (fine) rales 49 1822 crackling rales 50 1823 rhonchi 51 1824 wheeze 52 1825 obstructive breathing 53 1826 pleural rub 54 1827 basilar crackles 55 1828 bilateral crackles -
Module 10: Vital Signs
Module 10: Vital Signs Module 10: Vital Signs Minimum Number of Theory Hours: 3 Recommended Clinical Hours: 6 Statement of Purpose: The purpose of this unit is to prepare students to know how, when and why vital signs are taken and how to report and chart these procedures. Students will learn the correct procedure for measuring temperature, pulse, respirations, and blood pressure. They will learn to recognize and report normal and abnormal findings. Terminology: Temperature: Blood Pressure Pulse Respiration Pain (effects on Vital signs) 1. Afebrile 10. Aneroid manometer 22. Apical 33. Abdominal respirations 46. Acute pain 2. Axilla 11. Bell 23. Arrhythmia 34. Apnea 47. Chronic pain 3. Celsius 12. Diaphragm 24. Bounding 35. Bradypnea 4. Fahrenheit 48. Phantom pain 13. Diastolic 25. Brachial 36. Cheyne-Stokes 5. Febrile 49. Pain scales 6. Metabolism 14. Hypertension 26. Bradycardia 37. Cyanosis 7. Mucosa 15. Hypotension 27. Carotid 38. Diaphragm 8. Pyrexia 16. Orthostatic hypotension 28. Pulse deficit 39. Dyspnea 9. Tympanic 17. Pre-hypertension 29. Radial 40. Labored respiration 18. Pulse pressure 30. Rhythm 41. Orthopnea 19. Sphygmomanometer 31. Thready 42. Shallow respiration 20. Stethoscope 32. Tachycardia 43. Stertorous 21. Systolic 44. Tachypnea 45. Temperature, Pulse, Respiration (TPR) Patient, patient/resident, and client are synonymous terms Californiareferring to Community the person Colleges Chancellor’s Office Nurse Assistant Model Curriculum - Revised December 2018 Page 1 of 46 receiving care Module 10: Vital Signs Patient, resident, and client are synonymous terms referring to the person receiving care Performance Standards (Objectives): Upon completion of three (3) hours of class plus homework assignments and six (6) hours of clinical experience, the student will be able to: 1. -

Chest Auscultation: Presence/Absence and Equality of Normal/Abnormal and Adventitious Breath Sounds and Heart Sounds A
Northwest Community EMS System Continuing Education: January 2012 RESPIRATORY ASSESSMENT Independent Study Materials Connie J. Mattera, M.S., R.N., EMT-P COGNITIVE OBJECTIVES Upon completion of the class, independent study materials and post-test question bank, each participant will independently do the following with a degree of accuracy that meets or exceeds the standards established for their scope of practice: 1. Integrate complex knowledge of pulmonary anatomy, physiology, & pathophysiology to sequence the steps of an organized physical exam using four maneuvers of assessment (inspection, palpation, percussion, and auscultation) and appropriate technique for patients of all ages. (National EMS Education Standards) 2. Integrate assessment findings in pts who present w/ respiratory distress to form an accurate field impression. This includes developing a list of differential diagnoses using higher order thinking and critical reasoning. (National EMS Education Standards) 3. Describe the signs and symptoms of compromised ventilations/inadequate gas exchange. 4. Recognize the three immediate life-threatening thoracic injuries that must be detected and resuscitated during the “B” portion of the primary assessment. 5. Explain the difference between pulse oximetry and capnography monitoring and the type of information that can be obtained from each of them. 6. Compare and contrast those patients who need supplemental oxygen and those that would be harmed by hyperoxia, giving an explanation of the risks associated with each. 7. Select the correct oxygen delivery device and liter flow to support ventilations and oxygenation in a patient with ventilatory distress, impaired gas exchange or ineffective breathing patterns including those patients who benefit from CPAP. 8. Explain the components to obtain when assessing a patient history using SAMPLE and OPQRST. -

The Main Symptoms of Pulmonary Diseases
The main symptoms of pulmonary diseases Peter Farkas MD Pulmonary physiology • IRV (~3.3 L) • TV (~ 0.5 L) • ERV (~ 1.0 L) • RV (~ 1.2 L) • Total lung capacity: IRV+TV+ERV+RV • Vital capacity: IRV+TV+ERV • Inspiratory capacity: IRV+TV • Functional residual capacity: ERV+RV • Respiratory minute volume 6 L/min • Alveolar ventillation 4.2 L/min • Maximal voluntary ventillation 125-170 L/min • FEV 1”: proportion of VC during 1 sec. of forced exspiration Pulmonary physiology • 16-20x/min • Diffusion capacity: CO2/O2 = 20:1 • Triggers – pCO2 (NB! in case of severe hypercapnia, hypoxia will drive breathing) – pH – PO2 Main signs and symptoms • History taking • Dyspnea • Coughing • Expectoration of sputum • Chest pain History taking • Smoking (active/passive; PY) • Chronic pulmonary diseases (asthma bronchiale, COPD, emphysaema) • Infectious hazard • Profession • Known broncho-pulmonary neoplasms • Trauma • Immuncompromised hosts (congenital/acquired immundeficiency) • Congenital broncho-pulmonary diseases (bronchiectasia, CF) Dyspnea • Disbalance between actual respitarory necessity and support (inreased metabolism, decreased cardio-respiratory function) • Perception: asinchrony between neural stimulation and muscle contraction/pulmonary expansion (delay) • Subjective feeling – „short of breath” (Borg, visual analogue scale 1- 10) • Objective signs – Frequency, depth, rhytm of breathing are changing (best detectable during speaking) – Accessory muscles are used – Patient is in a special position • Can be normal (during extreme physical excercise)