HS2020 Technical Report Template
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Citizens Wealth Platform 2017
2017 FEDERAL CAPITAL BUDGET PULLOUT Of the States in the SOUTH-EAST Geo-Political Zone C P W Citizens Wealth Platform Citizen Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) 2017 FEDERAL CAPITAL BUDGET of the States in the SOUTH EAST Geo-Political Zone Compiled by VICTOR EMEJUIWE For Citizens Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) 2017 SOUTH EAST FEDERAL CAPITAL BUDGET PULLOUT Page 2 First Published in August 2017 By Citizens Wealth Platform C/o Centre for Social Justice 17 Yaounde Street, Wuse Zone 6, Abuja Email: [email protected] Website: www.csj-ng.org Tel: 08055070909. Blog: csj-blog.org. Twitter:@censoj. Facebook: Centre for Social Justice, Nigeria 2017 SOUTH EAST FEDERAL CAPITAL BUDGET PULLOUT Page 3 Table of Contents Foreword 5 Abia State 6 Anambra State 26 Embonyi State 46 Enugu State 60 Imo State 82 2017 SOUTH EAST FEDERAL CAPITAL BUDGET PULLOUT Page 4 Foreword In the spirit of the mandate of the Citizens Wealth Platform to ensure that public resources are made to work and be of benefit to all, we present the South East Capital Budget Pullout for the financial year 2017. This has been our tradition in the last six years to provide capital budget information to all Nigerians. The pullout provides information on federal Ministries, Departments and Agencies, names of projects, amount allocated and their location. The Economic Recovery and Growth Plan (ERGP) is the Federal Government’s blueprint for the resuscitation of the economy and its revival from recession. -

Paper Number
British Journal of Applied Science & Technology 4(34): 4751-4770, 2014 ISSN: 2231-0843 SCIENCEDOMAIN international www.sciencedomain.org Delineating Aquifer Systems Using Dar Zarouk Parameters Determined from Surface Geoelectric Survey: Case Study of Okigwe District, Southeastern Nigeria Leonard I. Nwosu1*, Cyril N. Nwankwo1 and Anthony S. Ekine1 1Department of Physics, University of Port Harcourt, Nigeria. Authors’ contributions This work was carried out in collaboration between all authors. Author LIN designed the study, wrote the protocol, carried out the field survey, and wrote the first draft of the manuscript and managed literature searches. Authors CNN, ASE managed the literature searches and analyses of the study data. All authors read and approved the final manuscript. Article Information DOI: 10.9734/BJAST/2014/7798 Editor(s): (1) Vyacheslav O. Vakhnenko, Division of Geodynamics of Explosion, Subbotin Institute of Geophysics, National Academy of Sciences of Ukrainian, Ukraine. Reviewers: (1) Amos-Uhegbu, Chukwunenyoke, Department of Physics (Geophysics), Michael Okpara University of Agriculture, Umudike Abia-State, Nigeria. (2) Emad A. M. Salah Al-Heety, Applied Geology, College of Science, University of Anbar, Iraq. (3) Anonymous, Enugu State University Enugu, Nigeria. (4) Anonymous, University of Calabar, Nigeria. Complete Peer review History: http://www.sciencedomain.org/review-history.php?iid=671&id=5&aid=6184 Received 11th November 2013 th Original Research Article Accepted 10 June 2014 rd Article………… Article Published 23 September 2014 ABSTRACT This study is aimed at delineating the aquifer systems in the study area and hence determining the parts with higher aquifer yield. To achieve this, 120 Vertical Electrical Soundings (VES) were carried out in Okigwe District of Imo State of Nigeria, using the Schlumberger electrode array and a maximum electrode spread of 900 m. -

N Okigwe Zone, Southeastern Nigeria
Journal of Architecture and Construction Volume 3, Issue 3, 2020, PP 1-16 ISSN 2637-5796 Best Practice Building Integration Methods along Slopes (15% To 65% Gradient) N Okigwe Zone, Southeastern Nigeria Christopher Irehie1*, Napoleon Imaah2, and Patrick Youdeowei3 1Institute of Geosciences and Space Technology (IGST), Rivers State University, Nkpolu/Oroworukwo, Port Harcourt, Rivers State, Nigeria 2Department of Architecture, Rivers State University, Nkpolu/Oroworukwo, Port Harcourt, Rivers State, Nigeria 3Institute of Geosciences and Space Technology (IGST), Rivers State University, Nkpolu/Oroworukwo, Port Harcourt, Rivers State, Nigeria *Corresponding Author: Christopher Irehie, 1Institute of Geosciences and Space Technology (IGST), Rivers State University, Nkpolu/Oroworukwo, Port Harcourt, Rivers State, Nigeria ABSTRACT To create integral buildings along slopes require that the land form and topography of the slope be incorporated into the architectural designs and construction plans from the outset. The relevance of the study was informed by the need to bring man closer to natural environment visibly manifest in the form of slopes. The study, through data collection, analyses, and concept development determined five architectural floor methods of building integration along slopes. Different building integration methods fit into slopes of different gradients and angles which are classified by percentage characteristics as: Split level (4 – 6% slope); Build up above the slope (6 – 10% slope); Build into the slope (10 – 16% slope); Cut and fill (16 – 25% slope); and Multi-level (25% slope and above). For ease of analysis, the architectural floor methods of integration were catalogued into A, B, C and D systematic order for appropriate results presentation relative to slope factors. Keywords: Building integration, Concept, Slopes gradient, Slope angle, Slopes profile, Architectural floor method. -
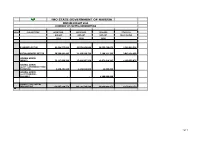
Imo State Government of Nigeria Revised Budget 2020 Summary of Capital Expenditure
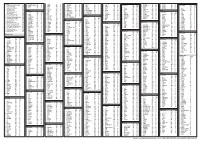
IMO STATE GOVERNMENT OF NIGERIA REVISED BUDGET 2020 SUMMARY OF CAPITAL EXPENDITURE HEAD SUB-SECTORS APPROVED APPROVED REVISED COVID-19 BUDGET BUDGET BUDGET RESPONSIVE 2019 2020 2020 ECONOMIC SECTOR 82,439,555,839 63,576,043,808 20,555,468,871 2,186,094,528 SOCIAL SERVICES SECTOR 50,399,991,403 21,139,598,734 7,190,211,793 3,043,134,650 GENERAL ADMIN: (MDA'S) 72,117,999,396 17,421,907,270 12,971,619,207 1,150,599,075 GENERAL ADMIN: (GOVT COUNTERPART FUND PAYMENTS) 9,690,401,940 4,146,034,868 48,800,000 - GENERAL ADMIN: (GOVT TRANSFER - ISOPADEC) - - 4,200,000,000 - GRAND TOTAL CAPITAL EXPENDITURE 214,647,948,578 106,283,584,680 44,966,099,871 6,379,828,253 1of 1 IMO STATE GOVERNMENT OF NIGERIA IMO STATE GOVERNMENT OF NIGERIA REVISED BUDGET 2020 MINISTERIAL SUMMARY OF CAPITAL EXPENDITURE ECONOMIC SECTOR APPROVED 2019 APPROVED 2020 REVISED 2020 COVID-19 RESPONSIVE O414 MINISTRY OF AGRICULTURE AND FOOD SECURITY 1,499,486,000 2,939,000,000 1,150,450,000 - 0 AGRIC & FOOD SECURITY 1,499,486,000 0414-2 MINISTRY OF LIVESTOCK DEVELOPMENT 1,147,000,000 367,000,000 367,000,000 - 0 LIVESTOCK 1,147,000,000 697000000 1147000000 0414-1 MINISTRY OF ENVIRONMENT AND NATURAL RESOURCES 13,951,093,273 1,746,000,000 620,000,000 - 0 MINISTRY OF ENVIRONMENT 13951093273 450000000 O415 MINISTRY OF COMMERCE AND INDUSTRY 7,070,700,000 2,650,625,077 1,063,000,000 - -5,541,800,000 MINISTRY OF COMMERCE, INDUSTRY AND ENTREPRENEURSHIP1528900000 0419-2 MINISTRY OF WATER RESOURCES 2,880,754,957 2,657,000,000 636,869,000 - 1,261,745,492 MINISTRY OF PUBLIC UTILITIES 4,142,500,449 -

Environmental-And-Social-Impact-Assessment-For-The-Rehabilitation-And-Construction-Of
Public Disclosure Authorized FEDERAL REPUPLIC OF NIGERIA IMO STATE RURAL ACCESS AND MOBILITY PROJECT (RAMP-2) ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT (ESIA) Public Disclosure Authorized FOR Public Disclosure Authorized THE REHABILITATION/ CONSTRUCTION OF 380.1KM OF RURAL ROADS IN IMO STATE August 2019 Public Disclosure Authorized Final ESIA for the Rehabilitation of 88 Rural Roads in Imo State under RAMP-2 TABLE OF CONTENTS TABLE OF CONTENTS ..................................................................................................................... ii LIST OF TABLES .............................................................................................................................. vii LIST OF FIGURES ........................................................................................................................... viii LIST OF PLATES ............................................................................................................................. viii LIST OF ACRONYMS AND ABBREVIATIONS ........................................................................... ix EXECUTIVE SUMMARY .................................................................................................................. x CHAPTER ONE: INTRODUCTION ................................................................................................. 1 1.1 Background................................................................................................................................ 1 1.2 Project Development Objective -

LGA Aboh Mbaise Ahiazu Mbaise Ehime Mbano Ezinihitte Mbaise Ideato North Ideato South Ihitte Uboma Ikeduru Isiala Mbano Isu Mbai
LGA Aboh Mbaise Ahiazu Mbaise Ehime Mbano Ezinihitte Mbaise Ideato North Ideato South Ihitte Uboma Ikeduru Isiala Mbano Isu Mbaitoli Ngor Okpala Njaba Nkwerre Nwangele Obowo Oguta Ohaji/Egbema Okigwe Onuimo Orlu Orsu Oru East Oru West Owerri Municipal Owerri North Owerri West PVC PICKUP ADDRESS Inside The Local Govt. Secretariat Behind The Local Govt. Stadium Along Umuezela Isiala Mbano Road, Near Aba Branch Inside The Lga Secretariat Inside The Lga Secretariat Behind The Lga Office (SHARES A Common Fence With The Lga Office Along Isinweke Express Road Opposite The Lga Office Along Umuelemai/Umuezeala Road Along The Lga Office Road, Umundugba Along Awo-Mbieri Road, Nwaorieubi Inside The Lga Office Inside The Lga Office Along Nkwerre Orlu Road, Near The Lga Office Situated Within The Old Site Of The Lga Office Along Umuahia-Obowo Road, Opp. Obowo Police Station At Nkwo-Oguta Inside The Lga Secretariat Office Inside The Lga Complex Inside The Lga Office Along Ezerioha Road Along Police Station Road Awo-Idemili Insde The Lga Office Along Onitsha-Owerri Road, Mgbidi (AFTER Magistrate Court-Sharing Same Fence Opposite The State Post Office, Along Douglas Road, Within The Lga Secretariat After The Lga H/Q (ORIE Uratta) Within The Lga Office Along Onitsha-Owerri Road, Mgbidi (AFTER Magistrate Court-Sharing Same Fence Opposite The State Post Office, Along Douglas Road, Within The Lga Secretariat. -

Flooding in Imo State Nigeria: the Socio-Economic Implication for Sustainable Development
Humanities and Social Sciences Letters 2014 Vol. 2, No. 3, pp. 129-140 ISSN(e): 2312-4318 ISSN(p): 2312-5659 © 2014 Conscientia Beam. All Rights Reserved FLOODING IN IMO STATE NIGERIA: THE SOCIO-ECONOMIC IMPLICATION FOR SUSTAINABLE DEVELOPMENT Duru Pat. N1 --- Chibo Christian N2 1,2Department of Geography and Environmental Management, Imo State University, Owerri ABSTRACT The menace of flooding ravaging different areas of Imo state Nigeria has been a recurrent phenomenon in recent years. This research investigated the socio-economic implications of flooding for sustainable development of the state. The paper aimed at investigating, identifying and documenting the socioeconomic implications of flooding to sustainable development of Imo state. The study tried to identify various locations affected by flooding and also examined the positive and negative effects of flood to the area. 500 copies of questionnaires were distributed using systematic sampling in six local government areas of the state used for pilot survey. About 96.8 percent of the questionnaires was retrieved and used for the study. Collected data were presented using frequency tables, charts and percentages. The study identified various locations affected by flooding, years of severe flooding and also identified various effects of flooding in the state. Finally the paper concluded by making recommendations which includes discouraging development of areas prone to flooding among others. Keywords: Menace, Flooding, Ravaging, Sustanainable development, Socio-economic, Floodplain, Environment. 1. INTRODUCTION Flood is a body of water which rises to overflow land which is not normally submerged. Flood results from a number of causes of which the most important are climatological in nature (Okorie, 2010). -

Groundwater Prospect for Siting Productive Water
ORIGINAL RESEARCH PAPER Physics Volume : 6 | Issue : 11 | November 2016 | ISSN - 2249-555X | IF : 3.919 | IC Value : 74.50 GROUNDWATER PROSPECT FOR SITING PRODUCTIVE WATER BOREHOLE USING TRANSMISSIVITY VALUES DETERMINED FROM PUMPING TEST AND SURFACE GEOELECTRIC SOUNDING DATA IN PARTS OF THE SEDIMENTARY AREA OF SOUTHEASTERN NIGERIA. KEYWORDS transmissivity, aquiferous zones, resistivity, pumping test data, hydraulic conductivity. Leonard I Nwosu Doris N. Ndubueze Department of Physics, University of Port Federal University of Agriculture Umudike, Harcourt, Nigeria Nigeria. ABSTRAC T Transmissivity values were determined from pumping test and surface geoelectric sounding data in Okigwe geopolitical zone of Imo state, Nigeria. Eleven out of the fteen boreholes drilled in the area, which have drawdown values were used to determine the parameters. The Schlumberger electrode array with a maximum electrode spacing of 900m were used to carry out 120 vertical electrical soundings (VES) across the study area. Relating the geoelectric resistivity data to the borehole hydrogeological information for the area led to delineation of probable aquiferous zones. The aquifer thickness increases towards the southern part to a maximum value of 104m obtained at Amonze in Obowo Local Government Area. Using an average transmissivity of 1030.085m2/day determined from the pumping test data, a mean conductance value of 19.222m/day was obtained for the area. The transmissivity values vary from 992m2/day to 1038m2/day while the hydraulic conductivity values range from 9.885 to 115.965m/day. Based on the result of the study, and the diagnostic hydraulic and electrical conductivity product (k) values, zones of sites for productive boreholes were delineated. -

2020 Issn: 2456-8643
International Journal of Agriculture, Environment and Bioresearch Vol. 5, No. 05; 2020 ISSN: 2456-8643 COMPARATIVE ASSESSMENT OF SELECTED ERODIBILITY INDICES FOR EROSION PREDICTION OF SOILS OF IMO STATE, SOUTHEAST, NIGERIA 1Madubuike, C. N., 1,2Nwachukwu, P. I., 3Emerson, K. U. and 2Asuzu, C. C. 1Department of Agricultural and Bio-resources Engineering, Federal University of Technology Owerri, Nigeria 2Imo State Polytechnic Umuagwo-Ohaji, Owerri, Imo State, Nigeria 3Civil Engineering and Geosciences, Newcastle University, United Kingdom https://doi.org/10.35410/IJAEB.2020.5563 ABSTRACT A performance evaluation of selected erodibility indices for erosion prediction of soils of Imo State, Nigeria, was performed. Soil samples were collected from 12 locations across three regions of Imo State (Owerri, Okigwe and Orlu), using completely randomized design. Samples were analysed for erodibility indices: modified clay ratio (MCR), clay ratio (CR), dispersion ratio (DR), and erosion ratio (ER), alongside selected physicochemical properties. Results indicated that the soils are predominantly sand. Soils of Owerri region are loamy sand texture, while Okigwe and Orlu regions are Sandy loam and Sand textured respectively. Bulk density of soils ranged from 1.50Mg/m3 1.81Mg/m3, while soil organic matter (SOM) averages 2.27% for Owerri and Orlu, and 0.92% for Okigwe respectively. MCR varied across the various locations in the order of Orlu (65.23 80.01) > Okigwe (43.11 55.30) > Owerri (15.20 35.65) regions. Least DR (0.58) and ER (0.44) were recorded in Owerri region, while highest values of 0.99 and 0.91 were recorded in Orlu region. A simulated rainfall intensity of 165mm/hr resulted in 1.2 ton/ha and 6.6 ton/ha annual soil loss for Owerri and Orlu respectively. -
States and Lcdas Codes.Cdr
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Haematological Profile in the Oil Producing Localities of Imo State, South-East, Nigeria
Current Journal of Applied Science and Technology 38(6): 1-27, 2019; Article no.CJAST.45000 ISSN: 2457-1024 (Past name: British Journal of Applied Science & Technology, Past ISSN: 2231-0843, NLM ID: 101664541) Haematological Profile in the Oil Producing Localities of Imo State, South-East, Nigeria Nnamdi N. Jibiri1 and Benedict C. Eke2* 1Department of Physics, Radiation and Health Physics Research Unit, University of Ibadan, Nigeria. 2Department of Physics, Radiation and Health Physics Research Group, Federal University of Technology, Owerri, Nigeria. Authors’ contributions This work was carried out in collaboration between both authors. Author NNJ supervised the study, laboratory procedures and statistical analysis. Author BCE designed the study, participated in the laboratory procedures and wrote the first draft of the manuscript. Both authors read and approved the final manuscript. Article Information DOI: 10.9734/CJAST/2019/v38i630438 Editor(s): (1) Dr. Chang-Yu Sun, Assistant Professor, China University of Petroleum, China. (2) Dr. Belisario Dominguez-Mancera, Laboratory of Cell Biology and Radioimmunoassay, School of Veterinary Medicine and Animal Science, University Veracruz, Mexico. (3) Dr. Teresa De Pilli, Assistant Professor, Department of Science of Agriculture of Food of Environment (SAFE), University of Foggia, Via Napoli, Italy. Reviewers: (1) Chukwuemeka C. Chukwuma, University of Port Harcourt, Nigeria. (2) Ariffin Samsuri, Universiti Teknologi Malaysia, Malaysia. (3) Neema Tiwari, ERA's Lucknow Medical University, India. Complete Peer review History: http://www.sdiarticle4.com/review-history/45000 Received 06 March 2019 Original Research Article Accepted 13 May 2019 Published 27 December 2019 ABSTRACT Aim: To determine if oil exploration and production in Ohaji/Egbema and Oguta LGAs have resulted in carcinogenic effects for a specific lifetime from exposures since our secondary data have shown a high percentage of cancer cases from the two LGAs. -

Geoelectric Survey for Mapping Groudnwater Flow Pattern in Okigwe District, Southeastern Nigeria
Geoelectric Survey for Mapping Groudnwater Flow Pattern in Okigwe District, Southeastern Nigeria. Leonard I. Nwosu*, Anthony S. Ekine, Cyril N. Nwankwo Department of Physics, University of Port Harcourt, Nigeria . E-mail Address: [email protected] , [email protected] , [email protected] ABSTRACT Aims: This study was carried out to determine the groundwater flow pattern in order to identify the converging centres with high yield expectations. Study design : The study area, Okigwe District in Imo State Nigeria, lies between latitude 5o30′N to 5 o57 ′N and longitude 7 o04 ′E to 7o26 ′E and covers an area of approximately 1,824 km 2. Methodology: One hundred and twenty (120) vertical electrical sounding (VES) results, using the Schlumberger configuration were acquired in order to map the ground water flow pattern within the study area. The maximum current electrode spacing for the survey was 900 m. Results: Twelve of the VES stations were sited near existing boreholes to enhance interpretation. The resistivity of the aquiferous zones varied across the study area ranging from 33.1 Ωm obtained at Umuedi (VES 7) in the northern part to 32600 Ωm at Otoko (VES 93) in the southern part of the area. Using an average transmissivity of 1032.0848 m 2/day determined from pumping test data of the boreholes in the area a mean conductance value of 91.222 m/day was obtained for the area. Analysis of VES data shows that the groundwater flows from the Northern part of the district towards the Southeastern part, South central and South Western parts. It also flows from the South-South area to Southeastern and South central parts of the study area forming two main collecting (converging) centres C1 and C2 having approximately West-East trend.