Cell‑Free DNA As a Liquid Biopsy for Early Detection of Gastric Cancer (Review)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Efficacy of Texture and Color Enhancement Imaging In
www.nature.com/scientificreports OPEN Efcacy of Texture and Color Enhancement Imaging in visualizing gastric mucosal atrophy and gastric neoplasms Tsubasa Ishikawa1, Tomoaki Matsumura1*, Kenichiro Okimoto1, Ariki Nagashima1, Wataru Shiratori1, Tatsuya Kaneko1, Hirotaka Oura1, Mamoru Tokunaga1, Naoki Akizue1, Yuki Ohta1, Keiko Saito1, Makoto Arai1,2, Jun Kato1 & Naoya Kato1 In 2020, Olympus Medical Systems Corporation introduced the Texture and Color Enhancement Imaging (TXI) as a new image-enhanced endoscopy. This study aimed to evaluate the visibility of neoplasms and mucosal atrophy in the upper gastrointestinal tract through TXI. We evaluated 72 and 60 images of 12 gastric neoplasms and 20 gastric atrophic/nonatrophic mucosa, respectively. The visibility of gastric mucosal atrophy and gastric neoplasm was assessed by six endoscopists using a previously reported visibility scale (1 = poor to 4 = excellent). Color diferences between gastric mucosal atrophy and nonatrophic mucosa and between gastric neoplasm and adjacent areas were assessed using the International Commission on Illumination L*a*b* color space system. The visibility of mucosal atrophy and gastric neoplasm was signifcantly improved in TXI mode 1 compared with that in white-light imaging (WLI) (visibility score: 3.8 ± 0.5 vs. 2.8 ± 0.9, p < 0.01 for mucosal atrophy; visibility score: 2.8 ± 1.0 vs. 2.0 ± 0.9, p < 0.01 for gastric neoplasm). Regarding gastric atrophic and nonatrophic mucosae, TXI mode 1 had a signifcantly greater color diference than WLI (color diferences: 14.2 ± 8.0 vs. 8.7 ± 4.2, respectively, p < 0.01). TXI may be a useful observation modality in the endoscopic screening of the upper gastrointestinal tract. -

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -

Circulating Tumor DNA As Biomarkers for Cancer Detection
Genomics Proteomics Bioinformatics 15 (2017) 59–72 HOSTED BY Genomics Proteomics Bioinformatics www.elsevier.com/locate/gpb www.sciencedirect.com REVIEW Circulating Tumor DNA as Biomarkers for Cancer Detection Xiao Han 1,2,a, Junyun Wang 1,b, Yingli Sun 1,*,c 1 CAS Key Laboratory of Genomic and Precision Medicine, China Gastrointestinal Cancer Research Center, Beijing Institute of Genomics, Chinese Academy of Sciences, Beijing 100101, China 2 University of Chinese Academy of Sciences, Beijing 100049, China Received 1 July 2016; revised 13 December 2016; accepted 20 December 2016 Available online 7 April 2017 Handled by Cesar Wong KEYWORDS Abstract Detection of circulating tumor DNAs (ctDNAs) in cancer patients is an important com- Precision medicine; ponent of cancer precision medicine ctDNAs. Compared to the traditional physical and biochemical Liquid biopsy; methods, blood-based ctDNA detection offers a non-invasive and easily accessible way for cancer Circulating tumor DNA; diagnosis, prognostic determination, and guidance for treatment. While studies on this topic are Biomarker; currently underway, clinical translation of ctDNA detection in various types of cancers has been Clinical diagnosis; attracting much attention, due to the great potential of ctDNA as blood-based biomarkers for early Cell-free nucleic acids diagnosis and treatment of cancers. ctDNAs are detected and tracked primarily based on tumor- related genetic and epigenetic alterations. In this article, we reviewed the available studies on ctDNA detection and described the representative methods. We also discussed the current understanding of ctDNAs in cancer patients and their availability as potential biomarkers for clin- ical purposes. Considering the progress made and challenges involved in accurate detection of speci- fic cell-free nucleic acids, ctDNAs hold promise to serve as biomarkers for cancer patients, and further validation is needed prior to their broad clinical use. -

Synergistic Genetic Interactions Between Pkhd1 and Pkd1 Result in an ARPKD-Like Phenotype in Murine Models
BASIC RESEARCH www.jasn.org Synergistic Genetic Interactions between Pkhd1 and Pkd1 Result in an ARPKD-Like Phenotype in Murine Models Rory J. Olson,1 Katharina Hopp ,2 Harrison Wells,3 Jessica M. Smith,3 Jessica Furtado,1,4 Megan M. Constans,3 Diana L. Escobar,3 Aron M. Geurts,5 Vicente E. Torres,3 and Peter C. Harris 1,3 Due to the number of contributing authors, the affiliations are listed at the end of this article. ABSTRACT Background Autosomal recessive polycystic kidney disease (ARPKD) and autosomal dominant polycystic kidney disease (ADPKD) are genetically distinct, with ADPKD usually caused by the genes PKD1 or PKD2 (encoding polycystin-1 and polycystin-2, respectively) and ARPKD caused by PKHD1 (encoding fibrocys- tin/polyductin [FPC]). Primary cilia have been considered central to PKD pathogenesis due to protein localization and common cystic phenotypes in syndromic ciliopathies, but their relevance is questioned in the simple PKDs. ARPKD’s mild phenotype in murine models versus in humans has hampered investi- gating its pathogenesis. Methods To study the interaction between Pkhd1 and Pkd1, including dosage effects on the phenotype, we generated digenic mouse and rat models and characterized and compared digenic, monogenic, and wild-type phenotypes. Results The genetic interaction was synergistic in both species, with digenic animals exhibiting pheno- types of rapidly progressive PKD and early lethality resembling classic ARPKD. Genetic interaction be- tween Pkhd1 and Pkd1 depended on dosage in the digenic murine models, with no significant enhancement of the monogenic phenotype until a threshold of reduced expression at the second locus was breached. -
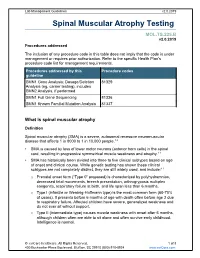
Spinal Muscular Atrophy Testing
Lab Management Guidelines v2.0.2019 Spinal Muscular Atrophy Testing MOL.TS.225.B v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline SMN1 Gene Analysis; Dosage/Deletion 81329 Analysis (eg, carrier testing), includes SMN2 Analysis, if performed SMN1 Full Gene Sequencing 81336 SMN1 Known Familial Mutation Analysis 81337 What is spinal muscular atrophy Definition Spinal muscular atrophy (SMA) is a severe, autosomal recessive neuromuscular disease that affects 1 in 8000 to 1 in 10,000 people.1,2 SMA is caused by loss of lower motor neurons (anterior horn cells) in the spinal cord, resulting in progressive symmetrical muscle weakness and atrophy.1-3 SMA has historically been divided into three to five clinical subtypes based on age of onset and clinical course. While genetic testing has shown these clinical subtypes are not completely distinct, they are still widely used, and include:1-3 o Prenatal onset form (“Type 0” proposed) is characterized by polyhydramnios, decreased fetal movements, breech presentation, arthrogryposis multiplex congenita, respiratory failure at birth, and life span less than 6 months. o Type I (infantile or Werdnig-Hoffmann type) is the most common form (60-70% of cases). It presents before 6 months of age with death often before age 2 due to respiratory failure. Affected children have severe, generalized weakness and do not ever sit without support. -

Microsatellite Instability in Colorectal Cancer Liquid Biopsy—Current Updates on Its Potential in Non-Invasive Detection, Prognosis and As a Predictive Marker
diagnostics Review Microsatellite Instability in Colorectal Cancer Liquid Biopsy—Current Updates on Its Potential in Non-Invasive Detection, Prognosis and as a Predictive Marker Francis Yew Fu Tieng 1 , Nadiah Abu 1, Learn-Han Lee 2,* and Nurul-Syakima Ab Mutalib 1,2,3,* 1 UKM Medical Molecular Biology Institute (UMBI), Universiti Kebangsaan Malaysia, Kuala Lumpur 56000, Malaysia; [email protected] (F.Y.F.T.); [email protected] (N.A.) 2 Novel Bacteria and Drug Discovery Research Group, Microbiome and Bioresource Research Strength, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Selangor 47500, Malaysia 3 Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur 50300, Malaysia * Correspondence: [email protected] (L.-H.L.); [email protected] (N.-S.A.M.); Tel.: +60-391459073 (N.-S.A.M.) Abstract: Colorectal cancer (CRC) is the third most commonly-diagnosed cancer in the world and ranked second for cancer-related mortality in humans. Microsatellite instability (MSI) is an indicator for Lynch syndrome (LS), an inherited cancer predisposition, and a prognostic marker which predicts the response to immunotherapy. A recent trend in immunotherapy has transformed cancer treatment to provide medical alternatives that have not existed before. It is believed that MSI-high (MSI-H) CRC patients would benefit from immunotherapy due to their increased immune infiltration and higher neo-antigenic loads. MSI testing such as immunohistochemistry (IHC) and PCR MSI assay Citation: Tieng, F.Y.F.; Abu, N.; Lee, has historically been a tissue-based procedure that involves the testing of adequate tissue with a high L.-H.; Ab Mutalib, N.-S. -

797 Circulating Tumor DNA and Circulating Tumor Cells for Cancer
Medical Policy Circulating Tumor DNA and Circulating Tumor Cells for Cancer Management (Liquid Biopsy) Table of Contents • Policy: Commercial • Coding Information • Information Pertaining to All Policies • Policy: Medicare • Description • References • Authorization Information • Policy History • Endnotes Policy Number: 797 BCBSA Reference Number: 2.04.141 Related Policies Biomarkers for the Diagnosis and Cancer Risk Assessment of Prostate Cancer, #336 Policy1 Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Plasma-based comprehensive somatic genomic profiling testing (CGP) using Guardant360® for patients with Stage IIIB/IV non-small cell lung cancer (NSCLC) is considered MEDICALLY NECESSARY when the following criteria have been met: Diagnosis: • When tissue-based CGP is infeasible (i.e., quantity not sufficient for tissue-based CGP or invasive biopsy is medically contraindicated), AND • When prior results for ALL of the following tests are not available: o EGFR single nucleotide variants (SNVs) and insertions and deletions (indels) o ALK and ROS1 rearrangements o PDL1 expression. Progression: • Patients progressing on or after chemotherapy or immunotherapy who have never been tested for EGFR SNVs and indels, and ALK and ROS1 rearrangements, and for whom tissue-based CGP is infeasible (i.e., quantity not sufficient for tissue-based CGP), OR • For patients progressing on EGFR tyrosine kinase inhibitors (TKIs). If no genetic alteration is detected by Guardant360®, or if circulating tumor DNA (ctDNA) is insufficient/not detected, tissue-based genotyping should be considered. Other plasma-based CGP tests are considered INVESTIGATIONAL. CGP and the use of circulating tumor DNA is considered INVESTIGATIONAL for all other indications. 1 The use of circulating tumor cells is considered INVESTIGATIONAL for all indications. -

Ciliopathies Gene Panel
Ciliopathies Gene Panel Contact details Introduction Regional Genetics Service The ciliopathies are a heterogeneous group of conditions with considerable phenotypic overlap. Levels 4-6, Barclay House These inherited diseases are caused by defects in cilia; hair-like projections present on most 37 Queen Square cells, with roles in key human developmental processes via their motility and signalling functions. Ciliopathies are often lethal and multiple organ systems are affected. Ciliopathies are London, WC1N 3BH united in being genetically heterogeneous conditions and the different subtypes can share T +44 (0) 20 7762 6888 many clinical features, predominantly cystic kidney disease, but also retinal, respiratory, F +44 (0) 20 7813 8578 skeletal, hepatic and neurological defects in addition to metabolic defects, laterality defects and polydactyly. Their clinical variability can make ciliopathies hard to recognise, reflecting the ubiquity of cilia. Gene panels currently offer the best solution to tackling analysis of genetically Samples required heterogeneous conditions such as the ciliopathies. Ciliopathies affect approximately 1:2,000 5ml venous blood in plastic EDTA births. bottles (>1ml from neonates) Ciliopathies are generally inherited in an autosomal recessive manner, with some autosomal Prenatal testing must be arranged dominant and X-linked exceptions. in advance, through a Clinical Genetics department if possible. Referrals Amniotic fluid or CV samples Patients presenting with a ciliopathy; due to the phenotypic variability this could be a diverse set should be sent to Cytogenetics for of features. For guidance contact the laboratory or Dr Hannah Mitchison dissecting and culturing, with ([email protected]) / Prof Phil Beales ([email protected]) instructions to forward the sample to the Regional Molecular Genetics Referrals will be accepted from clinical geneticists and consultants in nephrology, metabolic, laboratory for analysis respiratory and retinal diseases. -

Short Course 10 Metaplasia in The
0 3: 436-446 Rev Esp Patot 1999; Vol. 32, N © Prous Science, SA. © Sociedad Espajiola de Anatomia Patot6gica Short Course 10 © Sociedad Espafiola de Citologia Metaplasia in the gut Chairperson: NA. Wright, UK. Co-chairpersons: G. Coggi, Italy and C. Cuvelier, Belgium. Overview of gastrointestinal metaplasias only in esophagus but also in the duodenum, intestine, gallbladder and even in the pancreas. Well established is columnar metaplasia J. Stachura of esophageal squamous epithelium. Its association with increased risk of esophageal cancer is widely recognized. Recent develop- Dept. of Pathomorphology, Jagiellonian University ments have suggested, however, that only the intestinal type of Faculty of Medicine, Krakdw, Poland. metaplastic epithelium (classic Barrett’s esophagus) predisposes to cancer. Another field of studies is metaplasia in the short seg- ment at the esophago-cardiac junction, its association with Metaplasia is a reversible change in which one aduit cell type is Helicobacter pylon infection and/or reflux disease and intestinal replaced by another. It is always associated with some abnormal metaplasia in the cardiac and fundic areas. stimulation of tissue growth, tissue regeneration or excessive hor- Studies on gastric mucosa metaplasia could be divided into monal stimulation. Heterotopia, on the other hand, takes place dur- those concerned with pathogenesis and detailed structural/func- ing embryogenesis and is usually supposed not to be associated tional features and those concerned with clinical significance. with tissue damage. Pancreatic acinar cell clusters in pediatric gas- We know now that gastric mucosa may show not only complete tric mucosa form another example of aberrant cell differentiation. and incomplete intestinal metaplasia but also others such as ciliary Metaplasia is usually divided into epithelial and connective tis- and pancreatic metaplasia. -

Hyperplasia (Growth Factors
Adaptations Robbins Basic Pathology Robbins Basic Pathology Robbins Basic Pathology Coagulation Robbins Basic Pathology Robbins Basic Pathology Homeostasis • Maintenance of a steady state Adaptations • Reversible functional and structural responses to physiologic stress and some pathogenic stimuli • New altered “steady state” is achieved Adaptive responses • Hypertrophy • Altered demand (muscle . hyper = above, more activity) . trophe = nourishment, food • Altered stimulation • Hyperplasia (growth factors, . plastein = (v.) to form, to shape; hormones) (n.) growth, development • Altered nutrition • Dysplasia (including gas exchange) . dys = bad or disordered • Metaplasia . meta = change or beyond • Hypoplasia . hypo = below, less • Atrophy, Aplasia, Agenesis . a = without . nourishment, form, begining Robbins Basic Pathology Cell death, the end result of progressive cell injury, is one of the most crucial events in the evolution of disease in any tissue or organ. It results from diverse causes, including ischemia (reduced blood flow), infection, and toxins. Cell death is also a normal and essential process in embryogenesis, the development of organs, and the maintenance of homeostasis. Two principal pathways of cell death, necrosis and apoptosis. Nutrient deprivation triggers an adaptive cellular response called autophagy that may also culminate in cell death. Adaptations • Hypertrophy • Hyperplasia • Atrophy • Metaplasia HYPERTROPHY Hypertrophy refers to an increase in the size of cells, resulting in an increase in the size of the organ No new cells, just larger cells. The increased size of the cells is due to the synthesis of more structural components of the cells usually proteins. Cells capable of division may respond to stress by undergoing both hyperrtophy and hyperplasia Non-dividing cell increased tissue mass is due to hypertrophy. -

Neurological Manifestation of Sacral Tumors
Neurosurg Focus 15 (2):Article 1, 2003, Click here to return to Table of Contents Neurological manifestation of sacral tumors MICHAEL PAYER, M.D. Department of Neurosurgery, University Hopital of Geneva, Switzerland An extensive analysis of the existing literature concerning sacral tumors was conducted to characterize their clin- ical manifestations. Although certain specific manifestations can be attributed to some of the tumor types, a more general pattern of clinical presentation of an expansive sacral lesion can be elaborated. Local pain with or without pseudoradicular or radicular radiation is the most frequent initial symptom and is usually followed by the manifesta- tion of a lumbosacral sensorimotor deficit; bladder/bowel and/or sexual dysfunction appear throughout the natural course of disease. KEY WORDS • sacrum • tumor • lesion • neurological presentation All sacral and presacral tumors are rare.32,93 In one se- REVIEW OF SACRAL ANATOMY ries patients with these tumors were estimated to account for approximately one in 40,000 hospital admissions.93 Osseous Structures of the Sacrum Tumors arising from the bone of the sacrum are by far the The sacrum is a complex bone, comprising five sacral most frequent sacral tumors; chordomas are the most com- vertebrae that have fused. In its center lies the longitudi- mon and GCTs the second most common.20,46,50,61,74,81,98 nal sacral canal, which opens caudally posteriorly into the Although sacrococcygeal teratoma is the most common sacral hiatus, an incomplete posterior closure of the S-5 sacral tumor in neonates, it is very rare in adults.30,45,66 lamina. The thick anterior or pelvic face of the sacrum is The author conducted an extensive analysis of the exist- concave and contains four right- and left-sided anterior ing literature concerning tumors of the sacrum to charac- sacral foramina. -

De Novo, Systemic, Deleterious Amino Acid Substitutions Are Common in Large Cytoskeleton‑Related Protein Coding Regions
BIOMEDICAL REPORTS 6: 211-216, 2017 De novo, systemic, deleterious amino acid substitutions are common in large cytoskeleton‑related protein coding regions REBECCA J. STOLL1, GRACE R. THOMPSON1, MOHAMMAD D. SAMY1 and GEORGE BLANCK1,2 1Department of Molecular Medicine, Morsani College of Medicine, University of South Florida; 2Immunology Program, H. Lee Moffitt Cancer Center and Research Institute, Tampa, FL 33612, USA Received June 13, 2016; Accepted October 31, 2016 DOI: 10.3892/br.2016.826 Abstract. Human mutagenesis is largely random, thus large Introduction coding regions, simply on the basis of probability, represent relatively large mutagenesis targets. Thus, we considered Genetic damage is largely random and therefore tends to the possibility that large cytoskeletal-protein related coding affect the larger, functional regions of the human genome regions (CPCRs), including extra-cellular matrix (ECM) more frequently than the smaller regions (1). For example, coding regions, would have systemic nucleotide variants that a systematic study has revealed that cancer fusion genes, on are not present in common SNP databases. Presumably, such average, are statistically, significantly larger than other human variants arose recently in development or in recent, preceding genes (2,3). The large introns of potential cancer fusion genes generations. Using matched breast cancer and blood-derived presumably allow for many different productive recombina- normal datasets from the cancer genome atlas, CPCR single tion opportunities, i.e., many recombinations that would allow nucleotide variants (SNVs) not present in the All SNPs(142) for exon juxtaposition and the generation of hybrid proteins. or 1000 Genomes databases were identified. Using the Protein Smaller cancer fusion genes tend to be associated with the rare Variation Effect Analyzer internet-based tool, it was discov- types of cancer, for example EWS RNA binding protein 1 in ered that apparent, systemic mutations (not shared among Ewing's sarcoma.