Donepezil and Related Cholinesterase Inhibitors As Mood and Behavioral Controlling Agents Tal Burt, MD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pyridostigmine in the Treatment of Postural
Pyridostigmine in the Treatment of Postural Orthostatic Tachycardia: A Single-Center Experience KHALIL KANJWAL, M.D.,* BEVERLY KARABIN, PH.D.,* MUJEEB SHEIKH, M.D.,* LAWRENCE ELMER, M.D., PH.D.,† YOUSUF KANJWAL, M.D.,* BILAL SAEED, M.D.,* and BLAIR P. GRUBB, M.D.* From the *Electrophysiology Section, Division of Cardiology, Department of Medicine, The University of Toledo, Toledo, Ohio; and †Department of Neurology, The University of Toledo College of Medicine, Health Science Campus, Toledo, Ohio Background: The long-term efficacy of pyridostigmine, a reversible acetyl cholinesterase inhibitor, in the treatment of postural orthostatic tachycardia syndrome (POTS) patients remains unclear. We report our retrospective, single-center, long-term experience regarding the efficacy and adverse effect profile of pyridostigmine in the treatment of POTS patients. Methods: This retrospective study included an extensive review of electronic charts and data collection in regards to patient demographics, orthostatic parameters, side-effect profile, subjective response to therapy, as well as laboratory studies recorded at each follow-up visit to our institution’s Syncope and Autonomic Disorders Center. The response to pyridostigmine therapy was considered successful if patient had both symptom relief in addition to an objective response in orthostatic hemodynamic parameters (heart rate [HR] and blood pressure). Three hundred patients with POTS were screened for evaluation in this study. Of these 300, 203 patients with POTS who received pyridostigmine therapy were reviewed. Of these 203 patients, 168 were able to tolerate the medication after careful dose titration. The mean follow- up duration in this group of patients was 12 ± 3 (9–15) months. Pyridostigmine improved symptoms of orthostatic intolerance in 88 of 203 (43%) of total patients or 88 of 172 (51%) who were able to tolerate the drug. -

Relief of Hypersensitivity After Nerve Injury from Systemic Donepezil
Saranya devi Relief of Hypersensitivity after Nerve Injury from ALN Systemic Donepezil Involves Spinal Cholinergic and γ-Aminobutyric Acid Mechanisms Spinal ACh and GABA Mechanisms for Donepezil Analgesia Masafumi Kimura, M.D.,* Ken-ichiro Hayashida, D.V.M., Ph.D.,† James C. Eisenach, M.D.,‡ KIMURA ET AL. Shigeru Saito M.D.,§ Hideaki Obata, M.D.‖ XX ABSTRACT What We Already Know about This Topic • Donepezil increases central nervous system acetylcholine lev- Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/118/1/173/259568/0000542-201301000-00030.pdf by guest on 28 September 2021 10.1097/ALN.0b013e318277a81c Background: Evoking spinal release of acetylcholine (ACh) els and is used for treatment of dementia produces antinociception in normal animals and reduces • Increases in spinal acetylcholine levels have been implicated in the relief of neuropathic pain hypersensitivity after nerve injury, and some studies suggest January that ACh-mediated analgesia relies on γ-aminobutyric acid (GABA)-ergic signaling in the spinal cord. In this study, the authors tested the spinal mechanisms underlying the anti- What This Article Tells Us That Is New 118 hypersensitivity effects of donepezil, a central nervous sys- • Donepezil increased spinal acetylcholine levels and γ- tem–penetrating cholinesterase inhibitor, in a rat model of aminobutyric acid levels to reduce nociceptive responses after nerve injury and represents a potential therapeutic pathway to neuropathic pain. reduce pain after nerve injury Methods: Male Sprague-Dawley rats were anesthetized, and L5 spinal nerve ligation was performed unilaterally. With- A antagonist; and CGP 35348 (30 μg), a γ-aminobutyric drawal threshold to a paw pressure test was measured before acid receptor type B antagonist. -

Corticosterone and Pyridostigmine/DEET Exposure
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Neurotoxicology Manuscript Author . Author Manuscript Author manuscript; available in PMC 2019 May 24. Published in final edited form as: Neurotoxicology. 2019 January ; 70: 26–32. doi:10.1016/j.neuro.2018.10.006. Corticosterone and pyridostigmine/DEET exposure attenuate peripheral cytokine expression: Supporting a dominant role for neuroinflammation in a mouse model of Gulf War Illness Lindsay T. Michalovicza, Alicia R. Lockera, Kimberly A. Kellya, Julie V. Millera, Zachary Barnesb,c, Mary Ann Fletcherb,c, Diane B. Millera, Nancy G. Klimasb,c, Mariana Morrisb, Stephen M. Lasleyd, and James P. O’Callaghana,* aHealth Effects Laboratory Division, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Morgantown, WV, USA bInstitute for Neuro-Immune Medicine, Nova Southeastern University, Ft. Lauderdale, FL, USA cMiami Veterans Affairs Medical Center, Miami, FL, USA dDepartment of Cancer Biology & Pharmacology, University of Illinois College of Medicine at Peoria, Peoria, IL, USA Abstract Gulf War Illness (GWI) is a chronic multi-symptom disorder experienced by as many as a third of the veterans of the 1991 Gulf War; the constellation of “sickness behavior” symptoms observed in ill veterans is suggestive of a neuroimmune involvement. Various chemical exposures and conditions in theater have been implicated in the etiology of the illness. Previously, we found that GW-related organophosphates (OPs), such as the sarin surrogate, DFP, and chlorpyrifos, cause neuroinflammation. The combination of these exposures with exogenous corticosterone (CORT), mimicking high physiological stress, exacerbates the observed neuroinflammation. The potential relationship between the effects of OPs and CORT on the brain versus inflammation in the periphery has not been explored. -

Tor Amendment Tagoor Laboratories Private Limited
ToR Amendment Tagoor Laboratories Private Limited ANNEXURE – I Details of Products as per Granted ToR and Amendment Required Production Capacity S. Ton /Month Therapeutic Product Name No As per Amendment category granted ToR Required 1 Abacavir sulfate 2.0 2.0 Anti HIV 2 Amitriptyline 5.0 10.0 Antidepressant 3 Atrovastatin Calcium 5.0 5.0 Hypercholesterolemia 4 Bupropion 5.0 5.0 Anti depressant 5 carisoprodol 2.0 2.0 Muscle Relaxant 6 Clopidogrelbisulfate 5.0 5.0 Antithrombotic 7 Cyclobenzaprine HCl 5.0 5.0 Muscle relaxant 8 Cyproheptadine HCl 5.0 10.0 Anti allergic 9 Desloratadine 5.0 5.0 Antihistamine 10 Domperidone 20.0 30.0 Anti emetic 11 Domperidone maleate 2.0 2.0 Anti emetic 12 Donepezil HCl 1.0 1.0 Alzheimer’s disease 13 Ebastine 5.0 5.0 Anti allergic 14 Esomeprazole Sodium 3.0 3.0 Anti ulcerative Esomeprazole Magnesium 3.0 3.0 Anti ulcerative 15 trihydrate 16 Fexofenadine Hydrochloride 6.0 15.0 Anti histamine 17 Haloperidol 2.0 2.0 Antipsychotic 18 Itopride Hydrochloride 2.0 2.0 Antispasmodics 19 Itraconazole 10.0 10.0 Antifungal 20 Ketrolac Tromethane 2.0 2.0 Anti Inflammatory 21 Lansoprazole 10.0 10.0 Ant ulcerative 22 Loperamide Hydrochloride 10.0 10.0 Anti diarrhea agent 23 Losartan Potassium 6.0 15.0 Anti Hypertensive 24 Nebivolol HCl 2.0 2.0 Anti Hypertensive 25 Nortriptyline HCl 2.0 2.0 Anti depressant 26 Omeprazole 40.0 40.0 Anti ulcerative 27 Omeprazole Sodium 2.0 2.0 Ant ulcerative Omeprazole Magnesium 2.0 2.0 Ant ulcerative 28 Dihydrate 29 Oxatomide 1.0 1.0 Antihistamine Pantoprazole Sodium Sesqui 10.0 20.0 Ant ulcerative 30 Hydrate 31 Pimozide 2.0 2.0 Antipsychotic 32 Pregabalin 2.0 2.0 Epileptic 33 Quetiapine Hemifumarate 2.0 2.0 Antipsychotic Prepared By Rightsource Industrial Solutions Pvt. -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Acetylcholinesterase Inhibitor Pyridostigmine Bromide Attenuates Gut Pathology and Bacterial Dysbiosis in a Murine Model of Ulcerative Colitis
Florida International University FIU Digital Commons HWCOM Faculty Publications Herbert Wertheim College of Medicine 10-23-2019 Acetylcholinesterase Inhibitor Pyridostigmine Bromide Attenuates Gut Pathology and Bacterial Dysbiosis in a Murine Model of Ulcerative Colitis SP Singh Hitendra S. Chand S. Banerjee H. Agarwal V. Raizada See next page for additional authors Follow this and additional works at: https://digitalcommons.fiu.edu/com_facpub Part of the Medicine and Health Sciences Commons This work is brought to you for free and open access by the Herbert Wertheim College of Medicine at FIU Digital Commons. It has been accepted for inclusion in HWCOM Faculty Publications by an authorized administrator of FIU Digital Commons. For more information, please contact [email protected]. Authors SP Singh, Hitendra S. Chand, S. Banerjee, H. Agarwal, V. Raizada, S. Roy, and M. Sopori Digestive Diseases and Sciences (2020) 65:141–149 https://doi.org/10.1007/s10620-019-05838-6 ORIGINAL ARTICLE Acetylcholinesterase Inhibitor Pyridostigmine Bromide Attenuates Gut Pathology and Bacterial Dysbiosis in a Murine Model of Ulcerative Colitis Shashi P. Singh1 · Hitendra S. Chand2 · Santanu Banerjee3 · Hemant Agarwal4 · Veena Raizada4 · Sabita Roy3 · Mohan Sopori1 Received: 30 March 2019 / Accepted: 10 September 2019 / Published online: 23 October 2019 © The Author(s) 2019 Abstract Background Ulcerative colitis (UC) is a Th2 infammatory bowel disease characterized by increased IL-5 and IL-13 expres- sion, eosinophilic/neutrophilic infltration, decreased mucus production, impaired epithelial barrier, and bacterial dysbiosis of the colon. Acetylcholine and nicotine stimulate mucus production and suppress Th2 infammation through nicotinic receptors in lungs but UC is rarely observed in smokers and the mechanism of the protection is unclear. -

Medical Control of the Glaucomas
Br J Ophthalmol: first published as 10.1136/bjo.56.3.272 on 1 March 1972. Downloaded from 272 call these cases of malignant glaucoma, using the old term in a new broader sense, or whether we devise a new terminology to describe such phenomena should perhaps await further experimentation. Conclusion Many questions still remain in regard to malignant glaucoma, and it is to be hoped that future observations will gradually elucidate them. Today, however, medical therapy consisting of the concurrent use of mydriatic-cycloplegic drops, carbonic anhydrase inhibitors, and hyperosmotic agents is available, and is proving to be effective in half the cases when continued for 5 days. In addition, the vitreous surgery described above is in our opinion a safe and reliable surgical procedure in cases of malignant glaucoma which are not relieved by medical therapy. COMMENTARY MALIGNANT GLAUCOMA Chandler's anterior chamber deepening procedure with gonioscopy used for diagnosis of the extent of synaechial closure of the angle does not seem to predispose to malignant glaucoma. Even though it is known that there is a predisposition to malignant glaucoma in the fellow eye, this eye should always be treated with a peripheral iridectomy as early as possible after the onset of malignant glaucoma in the opposite eye. No medical treatment of any sort should be given before the peripheral iridectomy, since both miotics and mydriatics may be dangerous before surgerycopyright. is performed. If the fellow eye has been operated upon when the angle has been completely open, then malignant glaucoma has not occurred. However, if angle-closure is present in the fellow eye at the time of surgery, then malignant glaucoma becomes very common. -
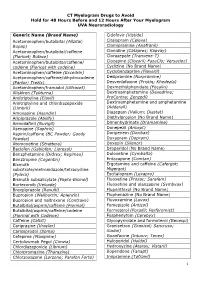
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology
CT Myelogram Drugs to Avoid Hold for 48 Hours Before and 12 Hours After Your Myelogram UVA Neuroradiology Generic Name (Brand Name) Cidofovir (Vistide) Acetaminophen/butalbital (Allzital; Citalopram (Celexa) Bupap) Clomipramine (Anafranil) Acetaminophen/butalbital/caffeine Clonidine (Catapres; Kapvay) (Fioricet; Butace) Clorazepate (Tranxene-T) Acetaminophen/butalbital/caffeine/ Clozapine (Clozaril; FazaClo; Versacloz) codeine (Fioricet with codeine) Cyclizine (No Brand Name) Acetaminophen/caffeine (Excedrin) Cyclobenzaprine (Flexeril) Acetaminophen/caffeine/dihydrocodeine Desipramine (Norpramine) (Panlor; Trezix) Desvenlafaxine (Pristiq; Khedezla) Acetaminophen/tramadol (Ultracet) Dexmethylphenidate (Focalin) Aliskiren (Tekturna) Dextroamphetamine (Dexedrine; Amitriptyline (Elavil) ProCentra; Zenzedi) Amitriptyline and chlordiazepoxide Dextroamphetamine and amphetamine (Limbril) (Adderall) Amoxapine (Asendin) Diazepam (Valium; Diastat) Aripiprazole (Abilify) Diethylpropion (No Brand Name) Armodafinil (Nuvigil) Dimenhydrinate (Dramamine) Asenapine (Saphris) Donepezil (Aricept) Aspirin/caffeine (BC Powder; Goody Doripenem (Doribax) Powder) Doxapram (Dopram) Atomoxetine (Strattera) Doxepin (Silenor) Baclofen (Gablofen; Lioresal) Droperidol (No Brand Name) Benzphetamine (Didrex; Regimex) Duloxetine (Cymbalta) Benztropine (Cogentin) Entacapone (Comtan) Bismuth Ergotamine and caffeine (Cafergot; subcitrate/metronidazole/tetracycline Migergot) (Pylera) Escitalopram (Lexapro) Bismuth subsalicylate (Pepto-Bismol) Fluoxetine (Prozac; Sarafem) -

Guideline for Preoperative Medication Management
Guideline: Preoperative Medication Management Guideline for Preoperative Medication Management Purpose of Guideline: To provide guidance to physicians, advanced practice providers (APPs), pharmacists, and nurses regarding medication management in the preoperative setting. Background: Appropriate perioperative medication management is essential to ensure positive surgical outcomes and prevent medication misadventures.1 Results from a prospective analysis of 1,025 patients admitted to a general surgical unit concluded that patients on at least one medication for a chronic disease are 2.7 times more likely to experience surgical complications compared with those not taking any medications. As the aging population requires more medication use and the availability of various nonprescription medications continues to increase, so does the risk of polypharmacy and the need for perioperative medication guidance.2 There are no well-designed trials to support evidence-based recommendations for perioperative medication management; however, general principles and best practice approaches are available. General considerations for perioperative medication management include a thorough medication history, understanding of the medication pharmacokinetics and potential for withdrawal symptoms, understanding the risks associated with the surgical procedure and the risks of medication discontinuation based on the intended indication. Clinical judgement must be exercised, especially if medication pharmacokinetics are not predictable or there are significant risks associated with inappropriate medication withdrawal (eg, tolerance) or continuation (eg, postsurgical infection).2 Clinical Assessment: Prior to instructing the patient on preoperative medication management, completion of a thorough medication history is recommended – including all information on prescription medications, over-the-counter medications, “as needed” medications, vitamins, supplements, and herbal medications. Allergies should also be verified and documented. -
Galantamine 4Mg/Ml Oral Solution Package Leaflet
Package leaflet: Information for the user Galantamine 4mg/ml Oral Solution Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. n Keep this leaflet. You may need to read it again. n If you have any further questions, ask your doctor or pharmacist. n This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. n If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Galantamine Oral Solution is and what it is used for 2. What you need to know before you take Galantamine Oral Solution 3. How to take Galantamine Oral Solution 4. Possible side effects 5. How to store Galantamine Oral Solution 6. Contents of the pack and other information 1. What Galantamine Oral Solution is and what it is used for What your medicine is The full name of your medicine is Galantamine 4mg/ml Oral Solution. In this leaflet the shorter name Galantamine is used. Galantamine belongs to a group of medicines known as ‘anti-dementia’ medicines. What your medicine is used for Galantamine is used in adults to treat the symptoms of mild to moderately severe Alzheimer’s disease. This is a type of dementia that alters the way the brain works. Alzheimer’s disease causes memory loss, confusion and changes in behaviour, which make it increasingly difficult to carry out normal daily tasks. -

Pharmacokinetics and Pharmacology of Drugs Used in Children
Drug and Fluid Th erapy SECTION II Pharmacokinetics and Pharmacology of Drugs Used CHAPTER 6 in Children Charles J. Coté, Jerrold Lerman, Robert M. Ward, Ralph A. Lugo, and Nishan Goudsouzian Drug Distribution Propofol Protein Binding Ketamine Body Composition Etomidate Metabolism and Excretion Muscle Relaxants Hepatic Blood Flow Succinylcholine Renal Excretion Intermediate-Acting Nondepolarizing Relaxants Pharmacokinetic Principles and Calculations Atracurium First-Order Kinetics Cisatracurium Half-Life Vecuronium First-Order Single-Compartment Kinetics Rocuronium First-Order Multiple-Compartment Kinetics Clinical Implications When Using Short- and Zero-Order Kinetics Intermediate-Acting Relaxants Apparent Volume of Distribution Long-Acting Nondepolarizing Relaxants Repetitive Dosing and Drug Accumulation Pancuronium Steady State Antagonism of Muscle Relaxants Loading Dose General Principles Central Nervous System Effects Suggamadex The Drug Approval Process, the Package Insert, and Relaxants in Special Situations Drug Labeling Opioids Inhalation Anesthetic Agents Morphine Physicochemical Properties Meperidine Pharmacokinetics of Inhaled Anesthetics Hydromorphone Pharmacodynamics of Inhaled Anesthetics Oxycodone Clinical Effects Methadone Nitrous Oxide Fentanyl Environmental Impact Alfentanil Oxygen Sufentanil Intravenous Anesthetic Agents Remifentanil Barbiturates Butorphanol and Nalbuphine 89 A Practice of Anesthesia for Infants and Children Codeine Antiemetics Tramadol Metoclopramide Nonsteroidal Anti-infl ammatory Agents 5-Hydroxytryptamine -

Retrospective Observation of Liver Function Parameters for 101 Patients Using Herbal Drugs for One Month
31 2 (2010 3 ) J Korean Oriental Med 2010;31(2):149-157 Original article 김동민1, 김회권2, 조성연3, 김용석1, 남상수1 1경희대학교 한의과대학 침구학교실, 2가평군 보건소, 3경희대학교 강남경희한방병원 침구과 Retrospective Observation of Liver Function Parameters for 101 Patients Using Herbal Drugs for One Month Dong-Min Kim 1, Hyee-Kwon Kim 2, Seong-Yeun Cho 3, Yong-Suk Kim 1, Sang-Soo Nam 1 1Dept. of Acupuncture & Moxibustion, College of Oriental Medicine, Kyung Hee University 2Gapyeong Public Health Center 3Dept. of Acupuncture & Moxibustion, Kangnam KyungHee Korean Hospital, Kyung Hee University Objective: The purpose of this study was to investigate the level of safety on liver functions when Korean herbal medicine was taken internally. Method: 101 inpatients who took Korean herbal medicine were enrolled and liver function test (aspartic aminotransferase, alanine aminotransferase, alkaline phosphatase, total bilirubin, gamma glutamyltranspeptidase, albumin, lactate dehydrogenase) was performed on admission and 1 month later. Results: In 101 patients, alkaline phosphatase and gamma glutamyltranspeptidase decreased significantly compared with the value taken on admission (p<0.05) but aspartic aminotransferase, alanine aminotransferase, total bilirubin, albumin, and lactate dehydrogenase were not significantly changed (p>0.05). In the patients who took Scutellaria baicalensis (n=34), alkaline phosphatase decreased and albumin increased significantly (p<0.05). Among the patients who took Atractylodes macrocephala (n=29), alkaline phosphatase decreased significantly (p<0.05). In the patients who took Glycyrrhiza uralensis or Paeonia lactiflora , liver function parameters were not significantly changed (p>0.05). On admission 11 patients had abnormal liver function and 2 patients had liver injury while 7 patients had abnormal liver function and 2 patients showed liver injury 1 month later.