Toxicological Profile for Nickel
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Development of the Periodic Table and Its Consequences Citation: J
Firenze University Press www.fupress.com/substantia The Development of the Periodic Table and its Consequences Citation: J. Emsley (2019) The Devel- opment of the Periodic Table and its Consequences. Substantia 3(2) Suppl. 5: 15-27. doi: 10.13128/Substantia-297 John Emsley Copyright: © 2019 J. Emsley. This is Alameda Lodge, 23a Alameda Road, Ampthill, MK45 2LA, UK an open access, peer-reviewed article E-mail: [email protected] published by Firenze University Press (http://www.fupress.com/substantia) and distributed under the terms of the Abstract. Chemistry is fortunate among the sciences in having an icon that is instant- Creative Commons Attribution License, ly recognisable around the world: the periodic table. The United Nations has deemed which permits unrestricted use, distri- 2019 to be the International Year of the Periodic Table, in commemoration of the 150th bution, and reproduction in any medi- anniversary of the first paper in which it appeared. That had been written by a Russian um, provided the original author and chemist, Dmitri Mendeleev, and was published in May 1869. Since then, there have source are credited. been many versions of the table, but one format has come to be the most widely used Data Availability Statement: All rel- and is to be seen everywhere. The route to this preferred form of the table makes an evant data are within the paper and its interesting story. Supporting Information files. Keywords. Periodic table, Mendeleev, Newlands, Deming, Seaborg. Competing Interests: The Author(s) declare(s) no conflict of interest. INTRODUCTION There are hundreds of periodic tables but the one that is widely repro- duced has the approval of the International Union of Pure and Applied Chemistry (IUPAC) and is shown in Fig.1. -
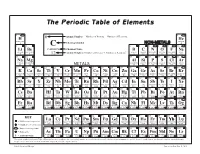
The Periodic Table of Elements
The Periodic Table of Elements 1 2 6 Atomic Number = Number of Protons = Number of Electrons HYDROGENH HELIUMHe 1 Chemical Symbol NON-METALS 4 3 4 C 5 6 7 8 9 10 Li Be CARBON Chemical Name B C N O F Ne LITHIUM BERYLLIUM = Number of Protons + Number of Neutrons* BORON CARBON NITROGEN OXYGEN FLUORINE NEON 7 9 12 Atomic Weight 11 12 14 16 19 20 11 12 13 14 15 16 17 18 SODIUMNa MAGNESIUMMg ALUMINUMAl SILICONSi PHOSPHORUSP SULFURS CHLORINECl ARGONAr 23 24 METALS 27 28 31 32 35 40 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 POTASSIUMK CALCIUMCa SCANDIUMSc TITANIUMTi VANADIUMV CHROMIUMCr MANGANESEMn FeIRON COBALTCo NICKELNi CuCOPPER ZnZINC GALLIUMGa GERMANIUMGe ARSENICAs SELENIUMSe BROMINEBr KRYPTONKr 39 40 45 48 51 52 55 56 59 59 64 65 70 73 75 79 80 84 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 RUBIDIUMRb STRONTIUMSr YTTRIUMY ZIRCONIUMZr NIOBIUMNb MOLYBDENUMMo TECHNETIUMTc RUTHENIUMRu RHODIUMRh PALLADIUMPd AgSILVER CADMIUMCd INDIUMIn SnTIN ANTIMONYSb TELLURIUMTe IODINEI XeXENON 85 88 89 91 93 96 98 101 103 106 108 112 115 119 122 128 127 131 55 56 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 CESIUMCs BARIUMBa HAFNIUMHf TANTALUMTa TUNGSTENW RHENIUMRe OSMIUMOs IRIDIUMIr PLATINUMPt AuGOLD MERCURYHg THALLIUMTl PbLEAD BISMUTHBi POLONIUMPo ASTATINEAt RnRADON 133 137 178 181 184 186 190 192 195 197 201 204 207 209 209 210 222 87 88 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 FRANCIUMFr RADIUMRa RUTHERFORDIUMRf DUBNIUMDb SEABORGIUMSg BOHRIUMBh HASSIUMHs MEITNERIUMMt DARMSTADTIUMDs ROENTGENIUMRg COPERNICIUMCn NIHONIUMNh -

How to Deal with Distressingly Dry Skin? — by Melissa Raue, PA-C How to Deal with Distressingly Dry Skin?
How To Deal With Distressingly Dry Skin? — By Melissa Raue, PA-C How To Deal With Distressingly Dry Skin? During the winter, some people’s skin often gets so dry that it flakes, cracks, or even bleeds. What can they do? Should they wash more or less often? Apply more moisturizer? Here are several preventive measures that will keep you comfortable and out of the doctor’s office. 1 Bathe daily. A 5-10 minute warm bath or shower adds moisture to the skin. Longer or hotter showers remove moisture and wash away natural protective oils. Close the 2 bathroom door. When taking that bath or shower, keep the door to the bathroom shut. This keeps the much-needed humidity in the room. Use a mild cleanser. 3 Deodorant bars, fragrance in soaps, and products containing alcohol strip natural oils from the skin, which dries the skin. Gently pat the skin dry. 4 Rubbing hard removes moisture and irritates sensitive dry skin. 5 Apply moisturizer within 3 minutes of getting out of the bath or shower. Many people think that moisturizer adds moisture to the skin. This is incorrect! Moisturizer traps existing water in the skin, preventing the water from evaporating. Moisturize 6 again if you need to! If skin is noticeably dry and uncomfortable, moisturizing more frequently throughout the day can help the skin heal. And will help prevent dry skin from returning. Ointments and creams will be more effective than lotions. Choose your moisturizer 7 by ingredients, not price. Moisturizer does not need to be expensive to be effective. -

The Nickel Silvers
Copper Development Association The Nickel Silvers Design Data and Applications 1965 Please note this publication is provided as an archive copy. The information given may therefore not be current. The Nickel Silvers Design Data and Applications 1965 Copper Development Association Copper Development Association is a non-trading organisation sponsored by the copper producers and fabricators to encourage the use of copper and copper alloys and to promote their correct and efficient application. Its services, which include the provision of technical advice and information, are available to those interested in the utilisation of copper in all its aspects. The Association also provides a link between research and user industries and maintains close contact with other copper development associations throughout the world. Website: www.copperinfo.co.uk Email: [email protected] Copyright: All information in this document is the copyright of Copper Development Association Disclaimer: Whilst this document has been prepared with care, Copper Development Association can give no warranty regarding the contents and shall not be liable for any direct, indirect or consequential loss arising out of its use Contents Contents ...............................................................................................................................................................1 Introduction .........................................................................................................................................................2 -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly. -

Unraveling the Underlying Heavy Metal Detoxification Mechanisms Of
microorganisms Review Unraveling the Underlying Heavy Metal Detoxification Mechanisms of Bacillus Species Badriyah Shadid Alotaibi 1, Maryam Khan 2 and Saba Shamim 2,* 1 Department of Pharmaceutical Sciences, College of Pharmacy, Princess Nourah Bint Abdulrahman University, Riyadh 11671, Saudi Arabia; [email protected] 2 Institute of Molecular Biology and Biotechnology (IMBB), Defence Road Campus, The University of Lahore, Lahore 55150, Pakistan; [email protected] * Correspondence: [email protected] Abstract: The rise of anthropogenic activities has resulted in the increasing release of various contaminants into the environment, jeopardizing fragile ecosystems in the process. Heavy metals are one of the major pollutants that contribute to the escalating problem of environmental pollution, being primarily introduced in sensitive ecological habitats through industrial effluents, wastewater, as well as sewage of various industries. Where heavy metals like zinc, copper, manganese, and nickel serve key roles in regulating different biological processes in living systems, many heavy metals can be toxic even at low concentrations, such as mercury, arsenic, cadmium, chromium, and lead, and can accumulate in intricate food chains resulting in health concerns. Over the years, many physical and chemical methods of heavy metal removal have essentially been investigated, but their disadvantages like the generation of chemical waste, complex downstream processing, and the uneconomical cost of both methods, have rendered them inefficient,. Since then, microbial bioremediation, particularly the Citation: Alotaibi, B.S.; Khan, M.; use of bacteria, has gained attention due to the feasibility and efficiency of using them in removing Shamim, S. Unraveling the heavy metals from contaminated environments. Bacteria have several methods of processing heavy Underlying Heavy Metal metals through general resistance mechanisms, biosorption, adsorption, and efflux mechanisms. -

Health Risk Assessments of Arsenic and Toxic Heavy Metal Exposure in Drinking Water in Northeast Iran
Alidadi et al. Environmental Health and Preventive Medicine (2019) 24:59 Environmental Health and https://doi.org/10.1186/s12199-019-0812-x Preventive Medicine RESEARCHARTICLE Open Access Health risk assessments of arsenic and toxic heavy metal exposure in drinking water in northeast Iran Hosein Alidadi1,4†, Seyedeh Belin Tavakoly Sany2,4† , Batoul Zarif Garaati Oftadeh3,4,7*, Tafaghodi Mohamad5,7, Hosein Shamszade6 and Maryam Fakhari7 Abstract Background: Arsenic and heavy metals are the main cause of water pollution and impact human health worldwide. Therefore, this study aims to assess the probable health risk (non-carcinogenic and carcinogenic risk) for adults and children that are exposed to arsenic and toxic heavy metals (Pb, Ni, Cr, and Hg) through ingestion and dermal contact with drinking water. Method: In this study, chemical analysis and testing were conducted on 140 water samples taken from treated drinking water in Mashhad, Iran. The health risk assessments were evaluated using hazard quotient (HQ), hazard index (HI), and lifetime cancer risk (CR). Results: The results of the HQ values of arsenic and heavy metals for combined pathways were below the safety level (HQ < 1) for adults, while the HI for children were higher than the safety limit in some stations. Likewise, Cr showed the highest average contribution of HItotal elements (55 to 71.2%) for adult and children population. The average values of total carcinogenic risk (TCR) through exposure to drinking water for children and adults were 1.33 × 10−4 and 7.38 × 10−5, respectively. Conclusion: Overall, the CRtotal through exposure to drinking water for children and adults was borderline or higher than the safety level of US EPA risk, suggesting the probability of carcinogenic risk for the children and adults to the carcinogenic elements via ingestion and dermal routes. -

Removal of Heavy Metal Ions from Wastewater by Chemically Modified Agricultural Waste Material As Potential Adsorbent-A Review
International Journal of Current Engineering and Technology E-ISSN 2277 – 4106, P-ISSN 2347 – 5161 ©2018 INPRESSCO®, All Rights Reserved Available at http://inpressco.com/category/ijcet Review Article Removal of Heavy Metal Ions from Wastewater by Chemically Modified Agricultural Waste Material as Potential Adsorbent-A Review Jyotikusum Acharya#^, Upendra Kumar^ and P. Mahammed Rafi#* #Department of Civil Engineering, Mallareddy Institute of Technology and Sciences, Hyderabad, India ^Department of Civil Engineering, National Institute of Technology, Silchar, Assam, India Received 05 March 2018, Accepted 08 May 2018, Available online 11 May 2018, Vol.8, No.3 (May/June 2018) Abstract Heavy metal remediation of aqueous streams is of special concern due to recalcitrant and persistency of heavy metals in environment. Conventional treatment technologies for the removal of these toxic heavy metals are not economical and further generate huge quantity of toxic chemical sludge. Agricultural waste materials being economic and eco- friendly due to their unique biochemical composition, availability in abundance, renewable, low in cost and more efficient are seem to be viable option for heavy metal remediation. The major advantages of biosorption over conventional treatment methods include: low cost, high efficiency, minimization of chemical or biological sludge, regeneration of biosorbents and possibility of metal recovery. It is well known that cellulosic waste materials can be obtained and employed as cheap adsorbents and their performance to remove heavy metal ions can be affected upon chemical treatment. In general, chemically modified plant wastes exhibit higher adsorption capacities than unmodified forms. The functional groups present in agricultural waste biomass viz. acetamido, alcoholic, carbonyl, phenolic, amido, amino, sulphydryl groups etc. -

Special-Purpose Nickel Alloys
© 2000 ASM International. All Rights Reserved. www.asminternational.org ASM Specialty Handbook: Nickel, Cobalt, and Their Alloys (#06178G) Special-Purpose Nickel Alloys NICKEL-BASE ALLOYS have a number of meet special needs. The grades considered in ganese, and copper, a 0.005% limit on iron, and unique properties, or combinations of proper- this section include the following: a 0.02% limit on carbon. This high purity re- ties, that allow them to be used in a variety of sults in lower coefficient of expansion, electri- specialized applications. For example, the high • Nickel 200 (99.6% Ni, 0.04% C) cal resistivity, Curie temperature, and greater resistivity (resistance to flow of electricity) and • Nickel 201 (99.6% Ni, 0.02% C maximum) ductility than those of other grades of nickel heat resistance of nickel-chromium alloys lead • Nickel 205 (99.6% Ni, 0.04% C, 0.04% Mg) and makes Nickel 270 especially useful for to their use as electric resistance heating ele- • Nickel 233 (see composition in table that fol- some electronics applications such as compo- ments. The soft magnetic properties of lows) nents of hydrogen thyratrons and as a substrate nickel-iron alloys are employed in electronic • Nickel 270 (99.97% Ni) for precious metal cladding. devices and for electromagnetic shielding of computers and communication equipment. Iron- Composition limits and property data on sev- eral of these grades can be found in the article nickel alloys have low expansion characteris- Resistance Heating Alloys tics as a result of a balance between thermal ex- “Wrought Corrosion-Resistant Nickels and pansion and magnetostrictive changes with Nickel Alloys” in this Handbook. -

Nickel in Drinking-Water (2005)
WHO/SDE/WSH/05.08/55 English only Nickel in Drinking-water Background document for development of WHO Guidelines for Drinking-water Quality © World Health Organization 2005 The illustration on the cover page is extracted from Rescue Mission: Planet Earth,© Peace Child International 1994; used by permission. This document may be freely reviewed, abstracted, reproduced and translated in part or in whole but not for sale or for use in conjunction with commercial purposes. Inquiries should be addressed to: [email protected]. The designations employed and the presentation of the material in this document do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. The World Health Organization does not warrant that the information contained in this publication is complete and correct and shall not be liable for any damages incurred as a result of its use. Preface One of the primary goals of WHO and its member states is that “all people, whatever their stage of development and their social and economic conditions, have the right to have access to an adequate supply of safe drinking water.” A major WHO function to achieve such goals is the responsibility “to propose .. -

Remediation of Nickel Ion from Wastewater by Applying Various Techniques: a Review
ISSN: 2576-6732 (Print) ISSN: 2576-6724 (Online) Acta Chemica Malaysia (ACMY) 2019, VOLUME 3, ISSUE 1 Remediation of Nickel ion from wastewater by applying various techniques: a review Ameet Kumara, Aamna Baloucha, Ashfaque Ahmed Pathanb, Abdullaha, Muhammad Saqaf Jagirania, Ali Muhammad Mahara, Muneeba Zubaira, Benazir Lagharia. aNational Centre of Excellence in Analytical Chemistry University of Sindh Jamshoro bDepartment of Civil Engineering, Mehran University of Engineering and Technology, Jamshoro, Pakistan *Corresponding author email: [email protected] DOI : 10.2478/acmy-2019-0001 Abstract: The remediation of organic and inorganic pollutants from the aqueous environment has touched a certain level with the development of research. Environmental pollution is increasing day by day due to industrial activities which cause a negative effect on human health and the ecosystem. Nowadays, heavy metals have a special concern due to its toxicity, persistence and bioaccumulation in nature. Toxic metals like chromium, nickel, arsenic, lead, mercury, cadmium are the main contaminants of water because they are non-biodegradable in nature. Nickel is also a toxic metal, mostly used in industries because of its anticorrosion behaviour. As a consequence nickel is present in the wastage of electroplating, tableware, metal finishing, plastics manufacturing, nickel-cadmium batteries, fertilizers and mining industries and these waste have dangerous impact on the human health and environment and causes the diseases i.e. diarrhea, anemia, hepatitis, kidney damage, gastrointestinal distress, skin dermatitis, and central nervous system dysfunction. In the present review article, several techniques are discussed for the treatment of nickel from the industrial environment. The elimination of nickel from wastewater is not important only for economic purposes but also for environmental safety. -

Urine Elements Resource Guide
Urine Elements Resource Guide Science + Insight doctorsdata.com Doctor’s Data, Inc. Urine Elements Resource Guide B Table of Contents Sample Report Sample Report ........................................................................................................................................................................... 1 Urine Toxic Metals Profile Introduction .................................................................................................................................................................................3 Aluminum .....................................................................................................................................................................................3 Antimony .......................................................................................................................................................................................4 Arsenic ............................................................................................................................................................................................ 4 Barium ............................................................................................................................................................................................. 5 Beryllium ........................................................................................................................................................................................5 Bismuth .........................................................................................................................................................................................