Primary Hyperparathyroidism and Familial Hyperparathyroid Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

When Is It Minimally Invasive?
ORIGINAL ARTICLE Incision Length for Standard Thyroidectomy and Parathyroidectomy When Is It Minimally Invasive? Laurent Brunaud, MD; Rasa Zarnegar, MD; Nobuyuki Wada, MD; Philip Ituarte, PhD; Orlo H. Clark, MD; Quan-Yang Duh, MD Hypothesis: Current techniques for open conven- parathyroidectomy (PϽ.001). It was 4.1 cm for bilateral tional thyroidectomy or parathyroidectomy have evolved parathyroid exploration, but was reduced to 3.2 and 2.8 to enable a shorter incision (main proposition), and the cm for unilateral (PϽ.001) and focal (PϽ.001) explora- length of the incision is influenced by objective factors. tions, respectively. By multiple regression analysis, thy- roid specimen volume and patient body mass index were Design: Case series. independent predictors of incision length in thyroidec- tomy. Extent of exploration and resident training level Setting: University referral center. were independent predictors of incision length in parathyroidectomy. Patients and Intervention: Retrospective study of the most recent 200 primary consecutive routine thyroid and Conclusions: Current techniques for open conven- parathyroid operations (excluding neck dissections). tional thyroidectomy or parathyroidectomy have evolved to enable a shorter incision. Thyroid volume, patient body Main Outcome Measures: The length of incision was mass index, extent of the planned parathyroid explora- routinely measured with a ruler before the incision. tion, and the resident clinical training stage are impor- Univariate and multivariate analysis was performed to dis- tant variables for incision length in open operation and tinguish variables affecting length of incision. should be taken into account when minimally invasive thyroidectomy and parathyroidectomy are evaluated. Results: Mean length of the incision was 5.5 cm for to- tal thyroidectomy, 4.6 cm for lobectomy, and 3.5 cm for Arch Surg. -

Inadvertent Parathyroidectomy During Thyroid Surgery for Papillary Thyroid Carcinoma and Postoperative Hypocalcemia
ORIGINAL J Korean Thyroid Assoc ARTICLE Vol. 5, No. 1, May 2012 Inadvertent Parathyroidectomy during Thyroid Surgery for Papillary Thyroid Carcinoma and Postoperative Hypocalcemia Dongbin Ahn, MD1, Jin Ho Sohn, MD, PhD1, Jae Hyug Kim, MD1, Ji Young Park, MD2 and Junesik Park, MD, PhD3 Departments of Otolaryngology-Head and Neck Surgery1, Pathology2, School of Medicine, Kyungpook National University, Department of Otolaryngology-Head and Neck Surgery, School of Medicine, Catholic University of Daegu3, Daegu, Korea Background and Objectives: The aim of this article is to report our experience of inadvertent parathyroidectomy during thyroid surgery and to analyze its associated factors and clinical implications. In addition, we attempted to determined causative factors that result in permanent hypocalcemia after thyroid surgery. Materials and Methods: We performed a retrospective review of 500 patients who underwent thyroid surgery for the treatment of papillary thyroid carcinoma from 2004 to 2008. Results: Inadvertent parathyroidectomy was identified in 7.4% of patients and only 1 parathyroid gland was inadvertently removed in most cases. The incidence of inadvertent parathyroidectomy was not associated with gender, age, type of surgical procedure, tumor size, coexisting Hashimoto’s thyroiditis (HT), extra-thyroidal extension (ETE), lymph node (LN) metastasis, and surgeon’s experience. Nor was inadvertent parathyroidectomy associated with permanent postoperative hypocalcemia. Although operating time >120 min, ETE, and total thyroidectomy (TT) with central neck dissection (CND) were found to be related to permanent hypocalcemia on univariate analysis, tumor size ≥1 cm and surgeon’s experience ≤5 years was statistically associated with permanent hypocalcemia on both univariate and multivariate analyses. Conclusion: Although inadvertent parathyroidectomy is not an uncommon complication of thyroid surgery, it appears to have only modest clinical implications. -

Primary Hyperparathyroidism and Celiac Disease: a Population-Based Cohort Study
ORIGINAL ARTICLE Endocrine Care Primary Hyperparathyroidism and Celiac Disease: A Population-Based Cohort Study Jonas F. Ludvigsson, Olle Ka¨ mpe, Benjamin Lebwohl, Peter H. R. Green, Shonni J. Silverberg, and Anders Ekbom Department of Pediatrics (J.F.L.), O¨ rebro University Hospital, 701 85 O¨ rebro, Sweden; Clinical Epidemiology Unit (J.F.L., A.E.), Department of Medicine, Karolinska Institutet, 171 76 Stockholm, Sweden; Department of Medical Sciences (O.K.), Uppsala University, University Hospital, 751 85 Uppsala, Sweden; and Celiac Disease Center (B.L., P.H.R.G.), and Division of Endocrinology, Department of Medicine (S.J.S.), Columbia University College of Physicians and Surgeons, New York, New York 10032 Context: Celiac disease (CD) has been linked to several endocrine disorders, including type 1 dia- betes and thyroid disorders, but little is known regarding its association to primary hyperpara- thyroidism (PHPT). Objective: The aim of the study was to examine the risk of PHPT in patients with CD. Design and Setting: We conducted a two-group exposure-matched nonconcurrent cohort study in Sweden. A Cox regression model estimated hazard ratios (HR) for PHPT. Participants: We identified 17,121 adult patients with CD who were diagnosed through biopsy reports (Marsh 3, villous atrophy) from all 28 pathology departments in Sweden. Biopsies were performed in 1969–2008, and biopsy report data were collected in 2006–2008. Statistics Sweden then identified 85,166 reference individuals matched with the CD patients for age, sex, calendar period, and county. Main Outcome Measure: PHPT was measured according to the Swedish national registers on inpatient care, outpatient care, day surgery, and cancer. -

Drugs for the Treatment of Hypercalcaemia C. R. PATERSON
Postgrad Med J: first published as 10.1136/pgmj.50.581.158 on 1 March 1974. Downloaded from Postgraduate Medical Journal (March 1974) 50, 158-162. Drugs for the treatment of hypercalcaemia C. R. PATERSON M.A., D.M., M.R.C.PATH. Department of Clinical Chemistry, University of Dundee, Dundee Summary able commercially (Phosphate Sandoz). The initial Hypercalcaemia is ordinarily treated by treatment of dose is 1-3 g (of phosphorus) per day according to the underlying disorder. In some cases, as in malignant the size of the patient. The serum calcium should be disease, in vitamin D poisoning and after a failed checked daily at first and the dose adjusted appro- parathyroidectomy, the hypercalcaemia itself needs to priately so that the maintenace dose is the minimum be treated. A large number of methods have been consistent with control of the serum calcium. Oral advocated for this, but phosphate is the drug of choice phosphate therapy is effective in the management of in most patients. This paper outlines its use, mode of hypercalcaemia of malignant disease and myeloma action and side effects and reviews the other methods (Goldsmith and Ingbar, 1966; Goldsmith et al., proposed for the management of hypercalcaemia. 1968; Thalassinos and Joplin, 1968), in hyperpara- thyroidism (Dent, 1962; Goldsmith and Ingbar, 1966; Eisenberg, 1968), and in vitamin D poisoningProtected by copyright. Introduction (Goldsmith and Ingbar, 1966). The management of hypercalcaemia is ordinarily Intravenous phosphate therapy is used in the that of the underlying disorder (Wills, 1971; management of acute hypercalcaemia, especially in Henrard, 1971; Watson, 1972). There are, however, the patient who is vomiting or in coma. -

Postoperative Calcium Requirements in 6000 Patients Undergoing
Postoperative Calcium Requirements in 6,000 Patients Undergoing Outpatient Parathyroidectomy: Easily Avoiding Symptomatic Hypocalcemia Marie Vasher, MD, Arnold Goodman, MD, FACS, Douglas Politz, MD, FACS, FACE, James Norman, MD, FACS, FACE BACKGROUND: To determine the amount and duration of supplemental oral calcium for patients with varying clinical presentations discharged immediately after surgery for primary hyperparathyroidism. STUDY DESIGN: A 4-year, prospective, single-institution study of 6,000 patients undergoing parathyroidectomy for primary hyperparathyroidism and discharged within 2.5 hours. Based on our previous studies, patients are started on a sliding scale of oral calcium determined by a number of preoperative measures (ie, serum calcium, body weight, osteoporosis) beginning 3 hours post- operation and decreasing to a maintenance dose by week 3. Patients reported all hypocalcemia symptoms daily for 2 weeks. RESULTS: Seven parameters were found to have a substantial impact on the amount of calcium required to prevent symptomatic hypocalcemia: preoperative serum calcium Ͼ12 mg/dL, Ͼ13 mg/dL, and Ͼ13.5 mg/dL, bone density T score less than Ϫ3, morbid obesity, removal of Ͼ1 parathyroid, and manipulation/biopsy of all remaining glands (all p Ͻ 0.05). Each independent variable increased the daily calcium required by 315 mg/day. Using our scaled protocol, Ͻ8% of patients showed symptoms of hypocalcemia, nearly all of whom were successfully self-treated with additional oral calcium. Only 6 patients (0.1%) required a visit to the emergency room for IV calcium, all occurring on postoperative day 3 or later. CONCLUSION: After outpatient parathyroidectomy, a specific calcium protocol has been verified that elimi- nates development of symptomatic hypocalcemia in Ͼ92% of patients, identifies patients at high risk for hypocalcemia, and allows self-medication with confidence in a predictable fashion for those patients in whom symptoms develop. -

Radioguided Surgery of Primary Hyperparathyroidism Using the Low
Radioguided Surgery of Primary Hyperparathyroidism Using the Low-Dose 99mTc- Sestamibi Protocol: Multiinstitutional Experience from the Italian Study Group on Radioguided Surgery and Immunoscintigraphy (GISCRIS) Domenico Rubello, MD1; Maria Rosa Pelizzo, MD2; Giuseppe Boni, MD3; Riccardo Schiavo, MD4; Luca Vaggelli, MD5; Giuseppe Villa, MD6; Sergio Sandrucci, MD7; Andrea Piotto, MD2; Gianpiero Manca, MD3; Pierluigi Marini, MD8; and Giuliano Mariani, MD3 1Nuclear Medicine Service, “S. Maria della Misericordia” Hospital, Rovigo, Italy; 2Department of Surgery, University of Padua Medical School, Padua, Italy; 3Regional Center of Nuclear Medicine, University of Pisa Medical School, Pisa, Italy; 4Nuclear Medicine Service, “S. Camillo-Forlanini” Hospital, Rome, Italy; 5Nuclear Medicine Service, “Careggi” University Hospital, Florence, Italy; 6Nuclear Medicine Service, “S. Martino” University Hospital, Genoa, Italy; 7Department of Surgery, University of Turin Medical School, Turin, Italy; and 8Division of Surgery, “S. Camillo-Forlanini” Hospital, Rome, Italy (11%) of transient postoperative hypocalcemia. The probe was 99m This study evaluated the accuracy of 99mTc-sestamibi scintigra- of little help in patients with concomitant Tc-sestamibi–avid phy and neck ultrasonography in patients with primary hyper- thyroid nodules and not helpful at all in patients with negative parathyroidism (PHPT) and the role of intraoperative hand-held scan findings preoperatively. IQPTH measurement helped to ␥-probes in minimally invasive radioguided surgery (MIRS) of disclose some cases of multigland parathyroid disease. Con- patients with a high likelihood of a solitary parathyroid adenoma clusion: 99mTc-Sestamibi scintigraphy, especially if combined (PA). The study was undertaken under the aegis of the Italian with neck ultrasonography, is highly accurate in selecting PHPT Study Group on Radioguided Surgery and Immunoscintigraphy candidates for MIRS. -

Minimally Invasive Parathyroidectomy Versus Bilateral Neck Exploration for Primary Hyperparathyroidism
Minimally Invasive Parathyroidectomy Versus Bilateral Neck Exploration for Primary Hyperparathyroidism Amanda M. Laird, MD*, Steven K. Libutti, MD KEYWORDS Primary hyperparathyroidism Parathyroidectomy Intraoperative parathyroid hormone Surgery Minimally invasive parathyroidectomy KEY POINTS The gold-standard surgical management of primary hyperparathyroidism (10HPT) is cer- vical exploration and identification of all 4 parathyroid glands. Imaging techniques, including ultrasound, sestamibi scans, and 4D-CT scans, have made identification of single parathyroid adenomas possible. Intraoperative parathyroid hormone (PTH) monitoring is a method to confirm biochemical cure before a patient leaves the operating room. There is some debate surrounding optimal surgical management of 10HPT because cure rates between minimally invasive parathyroidectomy (MIP) and bilateral neck exploration (BNE) are equivalent. Advantages of MIP include reduced operative time, reduced recovery time, less postop- erative pain, and lower complication rate with respect to injury to parathyroid glands and recurrent laryngeal nerves. INTRODUCTION 10HPT is a common disease, with a prevalence as high as 3%.1 Many advances in the surgical management of 10HPT have been made since the first parathyroidectomy was performed by Felix Mandl in 1925.2 Traditional surgical management consists of identification of all 4 parathyroid glands through a transverse cervical incision.3 Bet- ter understanding of the disease, interest in the practice of endocrine neck surgery, The authors have nothing to disclose. Montefiore Medical Center/Albert Einstein College of Medicine, Greene Medical Arts Pavilion, 3400 Bainbridge Avenue, 4th Floor, Bronx, NY 10467, USA * Corresponding author. E-mail address: [email protected] Surg Oncol Clin N Am 25 (2016) 103–118 http://dx.doi.org/10.1016/j.soc.2015.08.012 surgonc.theclinics.com 1055-3207/16/$ – see front matter Ó 2016 Elsevier Inc. -

A Case of Cushing Syndrome with Both Secondary Hypothyroidism and Hypercalcemia Due to Postoperative Adrenal Insufficiency
Endocrine Journal 2004, 51 (1), 105–113 NOTE A Case of Cushing Syndrome with Both Secondary Hypothyroidism and Hypercalcemia Due to Postoperative Adrenal Insufficiency MASAHITO KATAHIRA, TSUTOMU YAMADA* AND MASAHIKO KAWAI* Department of Internal Medicine, Kyoritsu General Hospital, Nagoya 456-8611, Japan *Division of Endocrinology, Department of Internal Medicine, Okazaki City Hospital, Okazaki 444-8553, Japan Abstract. A 48-year-old woman was referred to our hospital because of secondary hypothyroidism. Upon admission a left adrenal tumor was also detected using computed tomography. Laboratory data and adrenal scintigraphy were compatible with Cushing syndrome due to the left adrenocortical adenoma, although she showed no response to the TRH stimulation test. Hypercortisolism resulting in secondary hypothyroidism was diagnosed. After a left adrenalectomy, hydrocortisone administration was begun and the dose was reduced gradually. After discharge on the 23rd postoperative day, she began to suffer from anorexia. ACTH level remained low, and serum cortisol, free thyroxine and TSH levels were within the normal range. Since her condition became worse, she was re-admitted on the 107th postoperative day at which time serum calcium level was high (15.6 mg/dl). Both ACTH response to the CRH stimulation test and TSH response to the TRH stimulation test were restored to almost normal levels, but there was no response of cortisol to CRH stimulation test. We diagnosed that the hypercalcemia was due to adrenal insufficiency. Although the serum calcium level decreased to normal after hydrocortisone was increased (35 mg/day), secondary hypothyroidism recurred. It was suggested that sufficient glucocorticoids suppressed TSH secretion mainly at the pituitary level, which resulted in secondary (corticogenic) hypothyroidism. -

PARANEOPLASTIC SYNDROMES: J Neurol Neurosurg Psychiatry: First Published As 10.1136/Jnnp.2004.040378 on 14 May 2004
PARANEOPLASTIC SYNDROMES: J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.040378 on 14 May 2004. Downloaded from WHEN TO SUSPECT, HOW TO CONFIRM, AND HOW TO MANAGE ii43 J H Rees J Neurol Neurosurg Psychiatry 2004;75(Suppl II):ii43–ii50. doi: 10.1136/jnnp.2004.040378 eurological manifestations of cancer are common, disabling, and often multifactorial (table 1). The concept that malignant disease can cause damage to the nervous system Nabove and beyond that caused by direct or metastatic infiltration is familiar to all clinicians looking after cancer patients. These ‘‘remote effects’’ or paraneoplastic manifestations of cancer include metabolic and endocrine syndromes such as hypercalcaemia, and the syndrome of inappropriate ADH (antidiuretic hormone) secretion. Paraneoplastic neurological disorders (PNDs) are remote effects of systemic malignancies that affect the nervous system. The term PND is reserved for those disorders that are caused by an autoimmune response directed against antigens common to the tumour and nerve cells. PNDs are much less common than direct, metastatic, and treatment related complications of cancer, but are nevertheless important because they cause severe neurological morbidity and mortality and frequently present to the neurologist in a patient without a known malignancy. Because of the relative rarity of PND, neurological dysfunction should only be regarded as paraneoplastic if a particular neoplasm associates with a remote but specific effect on the nervous system more frequently than would be expected by chance. For example, subacute cerebellar ataxia in the setting of ovarian cancer is sufficiently characteristic to be called paraneoplastic cerebellar degeneration, as long as other causes have been ruled out. -

Paraneoplastic Syndromes in Patients with Ovarian Neoplasia
202 Journal of the Royal Society of Medicine Volume 86 April 1993 Paraneoplastic syndromes in patients with ovarian neoplasia C N Hudson MChir FRCS FRCOG1 Marigold Curling MB BS2 Penelope Potsides' D G Lowe MD MRCPath MIBiol' 'The Association of Obstetricians and Gynaecologists, NE Thames Region and 2the Department ofHistopathology, St Bartholomew's Hospital Medical College, London EClA 7BE Keywords: paraneoplastic syndromes; ovarian cancer; prevalence Summary data at presentation of 908 patients with primary The prevalence of several paraneoplastic syndromes epithelial ovarian cancer, collected prospectively in associated with ovarian cancer was determined from the North East Thames Region. a clinicopathological study of 908 patients with primary ovarian malignancy in the North East Thames Data source Region. The diversity and rarity of these manifesta- In the 1970s a data bank for ovarian cancer in the tions are great and the explanation for them is North East Metropolitan Region was set up by difficult. Circumstantial evidence suggests that in the Association of Obstetricians and Gynaecologists some cases an autoimmune phenomenon is the most of the Region in association with the Regional plausible cause. Histopathologists Group. Data was entered either by pathologist or clinician, and as soon as a case Introduction was notified, the clinical data on an agreed proforma Paraneoplastic syndromes are systemic manifestations were obtained from the surgeon concerned - he/ ofcancer that cannot readily be explained by the local she provided details of the mode of presentation, or metastatic effects of a tumour or of hormones investigation, operative staging, and treatment. indigenous to the tissue in which the tumour arises. Histological material was reviewed centrally by The syndromes fall into four broad groups, in which the two of the authors. -
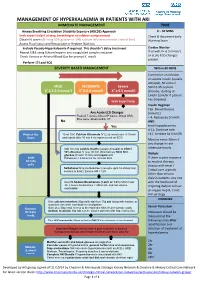
Management of Hyperkalaemia in Patients with Aki Immediate Management Time
MANAGEMENT OF HYPERKALAEMIA IN PATIENTS WITH AKI IMMEDIATE MANAGEMENT TIME ≥ Airway Breathing Circulation Disability Exposure (ABCDE) Approach 0 – 30 MINS Seek expert help if airway, breathing or circulation compromised Check & document Early Obtain IV access (If using 50% glucose or 10% calcium infusions consider central line) Warning Score Assess Fluid status and Resuscitate or Replace fluid loss Exclude Pseudo-Hyperkalaemia if required. This shouldn’t delay treatment Cardiac Monitor Repeat U&E using lithium heparin anti-coagulated sample container If unwell, K+ 6.5 mmol/L + or acute ECG changes Check Venous or Arterial Blood Gas for prompt K result P present Perform 12 Lead ECG SEVERITY BASED MANAGEMENT Within 60 MINS Commence an infusion of soluble insulin (usually actrapid), 50 units in MILD MODERATE Severe 50ml 0.9% sodium + + + K 5.5-5.9 mmol/l K 6-6.4 mmol/l K ≥ 6.5 mmol/l chloride, starting at 1ml/hr (2ml/hr if patient has diabetes) Seek Expert help Insulin Regimen Cap. Blood Glucose Any Acute ECG Changes (mmol/L) Peaked T waves, Absent P waves, Broad QRS, < 4: Reduce by 0.5ml/h Sine wave, Bradycardia, VT No AND Yes treat hypoglycaemia 4-11: Continue rate Protect the 10 ml 10% Calcium Gluconate IV (2.26 mmol) over 5-10 min >11: Increase by 0.5ml/h Heart and repeat after 10 min if no improvement on ECG Monitor every 30min if any change in rate Add 10 units soluble Insulin (usually Actrapid) to 250ml otherwise hourly 10% Glucose IV over 30 min (Alternatively 50ml 50% glucose IV over 15 min) and repeat until Dialysis Shift Potassium < 5.5mmol/L for at least 4hrs. -
Paraneoplastic Hypercalcaemia Associated with TCC of Bladder
Case Study TheScientificWorldJOURNAL (2004) 4, 1069–1070 ISSN 1537-744X; DOI 10.1100/tsw.2004.187 Paraneoplastic Hypercalcaemia Associated with TCC of Bladder A.B. Patel1,*, L. Wilson2, C. Blick2, and P. Meffan2 1Institute of Urology and Nephrology, UCL Medical School, Charles Bell House, 67 Riding House Street, London; 2Department of Urology, East Surrey Hospital, Redhill, Surrey and Sussex NHS Trust, U.K. E-mail: [email protected] Received July 14, 2004; Revised September 28, 2004; Accepted October 5, 2004; Published December 10, 2004 KEYWORDS: TCC, hypercalcaemia,paraneoplastic syndrome DOMAIN: urology Hypercalcaemia associated with transitional carcinoma of the bladder is rare in the absence of metastatic disease. We report a case of paraneoplastic hypercalcaemia associated with a high-grade, organ-confined bladder carcinoma, which resolved upon surgical resection of the tumour. CASE REPORT A 58-year-old woman presented with a 3-week history of weight loss, general malaise, and constipation as well as two episodes of macroscopic haematuria. Laboratory testing on admission to hospital showed marked hypercalcaemia (3.66, normal 2.15–2.60) associated with a PTH level of 1.3 (normal 0.5–5.5) and acute renal failure (BUN 37.5, creatinine 280). Ultrasound examination showed moderate right hydroureteronephrosis associated with a large, lobulated echogenic mass in the bladder. Immediate treatment involved intravenous colloid infusion, intravenous furosemide, and intravenous pamidronate in order to treat the hypercalcaemia. Subsequent transurethral bladder resection revealed grade 3 pT2 transitional cell carcinoma (TCC). Staging computerised tomography and bone scan showed no evidence of local or distant metastatic disease. The patient then underwent radical cystectomy and ileal conduit formation.