Testing Bullet Slide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OM-85) on Frequency of Upper Respiratory Tract Infections and Size of Adenoid Tissue in Preschool Children with Adenoid Hypertrophy
STUDY PROTOCOL Effect of Vaxoral® (OM-85) on frequency of upper respiratory tract infections and size of adenoid tissue in preschool children with adenoid hypertrophy Study Product(s) Vaxoral® (OM-85) Indication Recurrent RTIs, adenoid hypertrophy Sponsor Dr Sami Ulus Maternity and Children Research and Training Hospital, Department of Pediatric Allergy and Immunology, Ankara, TURKEY Anticipated Turkey Countries Introduction OM-85 significantly reduces RTIs in children. This effect was proved by many clinical studies and meta-analyses1. A Cochrane meta-analysis first published in 2006 and updated recently (Del- Rio-Navarro 2012) showed that immunostimulants (IS) could reduce acute RTIs (ARTIs) by almost 39% when compared to placebo. Among the different IS, OM-85 showed the most robust evidence with 4 trials of “A quality” according to the Cochrane grading criteria. Pooling six OM-85 studies, the Cochrane review reported a mean number of ARTIs reduction by -1.20 [95% CI: - 1.75, -0.66] and a percentage difference in ARTIs by -35.9% [95% CI: -49.46, -22.35] compared to placebo1. Adenoid hypertrophy (AH) is one of the most important respiratory disease in preschool children2. In normal conditions adenoid tissue enlarges up to 5 years and become smaller afterwards. But in some children who have recurrent URTIs, it keeps growing and this can be associated with complications2. AH may cause recurrent respiratory infections and each infection contributes to enlargement of adenoid tissue thus promoting a vicious cycle. Additionally enlarged adenoids are known to be reservoir for microbes and cause of recurrent or long lasting RTIs3. AH is associated with chronic cough, recurrent and chronic sinusitis, recurrent tonsillitis, recurrent otitis media with effusion, recurrent other respiratory problems such as, nasal obstruction and sleep disturbances, sleep apneas2-3. -
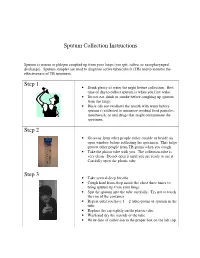
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Clinical Study Microbiological Profile of Adenoid Hypertrophy Correlates to Clinical Diagnosis in Children
Hindawi Publishing Corporation BioMed Research International Volume 2013, Article ID 629607, 10 pages http://dx.doi.org/10.1155/2013/629607 Clinical Study Microbiological Profile of Adenoid Hypertrophy Correlates to Clinical Diagnosis in Children Anita Szalmás,1 Zoltán Papp,2 Péter Csomor,2 József Kónya,1 István Sziklai,2 Zoltán Szekanecz,3 and Tamás Karosi2 1 Department of Medical Microbiology, Medical and Health Science Center, University of Debrecen, Nagyerdei Krt. 98, Debrecen 4032, Hungary 2 Department of Otolaryngology and Head and Neck Surgery, Medical and Health Science Center, University of Debrecen, Nagyerdei Krt. 98, Debrecen 4032, Hungary 3 Department of Rheumatology, Medical and Health Science Center, University of Debrecen, Nagyerdei Krt. 98, Debrecen 4032, Hungary Correspondence should be addressed to Tamas´ Karosi; [email protected] Received 24 April 2013; Accepted 23 August 2013 Academic Editor: Ralph Mosges¨ Copyright © 2013 Anita Szalmas´ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objective. Adenoid hypertrophy is a common condition in childhood, which may be associated with recurring acute otitis media (RAOM), otitis media with effusion (OME), and obstructive sleeppnea a syndrome (OSAS). These different clinical characteristics have some clinical overlap; however, they might be explained by distinct immunologic and infectious profiles and result in various histopathologic findings of adenoid specimens. Methods. A total of 59 children with adenoid hypertrophy undergoing adenoidectomy were studied. Three series of identical adenoid specimens were processed to hematoxylin-eosin (H.E.) and Gram staining and to respiratory virus specific real-time PCR, respectively. -

Factors Associated with Pleurisy in Pigs: a Case-Control Analysis of Slaughter Pig Data for England and Wales
Aus dem Zentrum für Klinische Tiermedizin der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Arbeit angefertigt unter der Leitung von Prof. Dr. Mathias Ritzmann Angefertigt am Cambridge Infectious Diseases Consortium, University of Cambridge, Department of Veterinary Medicine, Cambridge, UK (Dr. A W (Dan) Tucker) Factors associated with pleurisy in pigs: A case-control analysis of slaughter pig data for England and Wales Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Von Henrike Caroline Jäger aus Wiesbaden München 2012 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Univ.-Prof. Dr. Mathias Ritzmann Korreferent: Univ.-Prof. Dr. Dr. habil. Manfred Gareis Tag der Promotion: 9. Februar 2013 Meinem Vater Dr. med Sepp-Dietrich Jäger Table of Contents 4 TABLE OF CONTENTS I. INTRODUCTION ...................................................................................... 7 II. LITERATURE OVERVIEW .................................................................... 8 1. Anatomy and Physiology of the Pleura ....................................................8 2. Pleurisy ........................................................................................................9 2.1. Morphology ..................................................................................................9 2.2. Prevalence ..................................................................................................11 -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

Mediastinum and Subcutaneous Emphysema: a Rare Complication of a Common Procedure
Case Report Brunei Int Med J. 2017; 13 (1): 29-32 Post adenotonsillectomy pneumo- mediastinum and subcutaneous emphysema: A rare complication of a common procedure. Farah Wahida ABD MANAB1,2, Nor Shahida ABDUL MUTALLIB1, Hisham ABDUL RAH- MAN1, Hamidah MAMAT1 1Department of otorhinolaryngology-Head and Neck surgery, Hospital Sultan Abdul Halim, Kedah, Malaysia, 2Department of Otorhinolaryngology, Head and Neck Surgery, School of Medical Sciences, Universiti Sains Malaysia, Health Campus, 16150 Kubang Kerian, Kelantan, Malaysia ABSTRACT Cervicofacial and pneumomediastinum subcutaneous emphysema is a very rare complication of adenotonsillectomy procedure. Even though it is a self limiting complication and can be treated conservatively, it can alarming for the patient or patient’s family as well as leading to more seri- ous and fatal consequences occurring from tension pneumomediastinum. We report a case of incidental finding of pneumomediastinum in postadenotonsillectomy patient. He was managed conservatively and made an uneventful recovery. Keywords: tonsillectomy, subcutaneous emphysema, complication INTRODUCTION Case Report Adenotonsillectomy is a common surgical pro- A 12 year old boy was admitted to our Ear, cedure among paediatric age group. It is rela- Nose and Throat (ENT) ward for elective sur- tively a safe procedure with minimal compli- gery of adenotonsillectomy. The indication for cations. Common complications are intraoper- surgery was recurrent attacks of acute tonsil- ative or postoperative haemorrhage, infec- litis. He had underlying Allergic Rhinitis and tion, damaged to soft tissue and surrounding Bronchial Asthma. structure such as teeth, odynophagia and oropharyngeal edema.1 Cervicofacial and Patient was given general anaesthesia with pneumomediastinum subcutaneous emphyse- fentanyl, propofol and cisatracium during in- ma is a very rare complication. -

What Is Pertussis (Whooping Cough)?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What Is Pertussis (Whooping Cough)? Pertussis is a very contagious respiratory infection commonly known as ‘whooping cough’. It is caused by a bacterium called Bordetella pertussis. The infection became much less common after a successful vaccine was developed and given to children to help prevent infection. However, in recent years, the number of people infected with pertussis has increased and now is at the highest rate seen since the 1950’s. There is concern that this is due mainly to people not taking the pertussis (whooping cough) vaccination and adults who have not had a booster and their immune protection has weakened with age. Whooping cough usually starts as a mild cold-like illness get in the air. If you are close enough, you can breathe in these (upper respiratory infection). The pertussis bacteria enter the droplets or they can land on your mouth, nose, or eye. You lungs and cause swelling and irritation in the airways leading can also get the infection if you kiss the face of a person with to severe coughing fits. At times, people with whooping pertussis or get infected nose or mouth secretions on your cough can have a secondary pneumonia from other bacteria hands and then touch your own face to rub your eyes or nose. while they are ill. Whooping cough can cause very serious A person with pertussis can remain contagious for many weeks illness. It is most dangerous in young babies and can result unless treated with an antibiotic. in death. It spreads very easily and people who have the infection can still spread it to others for weeks after they What are the symptoms of Pertussis infection? become sick. -

Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT
University of Nebraska Medical Center DigitalCommons@UNMC Theses & Dissertations Graduate Studies Fall 12-18-2015 Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT Christopher C. Schultz University of Nebraska Medical Center Follow this and additional works at: https://digitalcommons.unmc.edu/etd Part of the Other Medical Specialties Commons Recommended Citation Schultz, Christopher C., "Evaluation of Upper Airway Changes Following Surgical Removal of the Adenoids Using 3-D Cone Beam CT" (2015). Theses & Dissertations. 54. https://digitalcommons.unmc.edu/etd/54 This Thesis is brought to you for free and open access by the Graduate Studies at DigitalCommons@UNMC. It has been accepted for inclusion in Theses & Dissertations by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. EVALUATION OF UPPER AIRWAY CHANGES FOLLOWING SURGICAL REMOVAL OF THE ADENOIDS USING 3-D CONE BEAM CT By Christopher C. Schultz, D.D.S A THESIS Presented to the Faculty of The Graduate College in the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Master of Science Medical Sciences Interdepartmental Area Oral Biology University of Nebraska Medical Center Omaha, Nebraska December, 2015 Advisory Committee: Sundaralingam Premaraj, BDS, MS, PhD, FRCD(C) Sheela Premaraj, BDS, PhD Peter J. Giannini, DDS, MS Stanton D. Harn, PhD i ACKNOWLEDGEMENTS I would like to express my thanks and gratitude to the members of my thesis committee: Dr. Sundaralingam Premaraj, Dr. Sheela Premaraj, Dr. Peter Giannini, and Dr. Stanton Harn. Your advice and assistance has been vital for the completion of the project. -

What Is Acute Respiratory Distress Syndrome?
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES What is Acute Respiratory Distress Syndrome? Acute Respiratory Distress Syndrome (ARDS) is a life-threatening illness in which the lungs are severely inflamed. Swelling throughout the lungs cause tiny blood vessels to leak fluid and the air sacs (alveoli) collapse or fill with fluid, preventing the lungs from working well. Patients with ARDS have problems getting enough oxygen into their blood so they must be given extra oxygen and will usually need a ventilator to breathe. Despite intensive treatment, about 40% of people with ARDS die from lung failure. Who gets ARDS? How is ARDS treated? It is estimated that ARDS affects about 150,000 Currently, there is no specific treatment for ARDS. Americans each year. ARDS can occur in many situations. Treatment consists of two goals: ARDS can affect people who have known lung disease or ■ treat any medical problem that led to the lung injury, other serious illnesses. A person can develop ARDS even and if he or she has not had lung disease or a lung problem in ■ support the person’s breathing (usually with a the past. ventilator) until the lungs heal. Most people with ARDS What causes ARDS? are treated in the hospital’s intensive care unit (ICU). The causes of ARDS are not well understood. Either Therapies commonly used for ARDS include: direct or indirect injuries can cause ARDS. Direct ■ Breathing support from a mechanical ventilator. injuries include: pneumonia, inhaling stomach contents ■ CLIP AND COPY AND CLIP Medicines to keep the person calm and comfortable (aspiration), breathing in harmful fumes or smoke, and while on the ventilator so that they can rest and injury to the chest that causes bruising of the lungs. -

What Is Acute Bronchitis?
What is acute bronchitis? FACT SHEET prepared by The Asthma and Respiratory Foundation NZ Acute bronchitis is an infection of the large bronchi (airways) in the lungs. The airways swell and thick mucus builds up inside them. It is often caused by the same viruses that cause the common cold. A minority of cases are caused by bacteria. How do I know that I have acute bronchitis? Acute bronchitis may accompany or closely follow a cold or influenza or may occur on its own. The major symptom of acute bronchitis is a productive cough that may bring up yellow or green sputum (phlegm). This cough can last several weeks. Some people may have shortness of breath and a wheeze. There may be other symptoms associated with the viral cause such as a runny nose, sore throat, fever, muscle aches and pains, sore eyes or headache, particularly early in the illness. Chest pain is not usually associated with bronchitis. Who gets acute bronchitis? Anyone can get acute bronchitis. It is more common in winter, especially during influenza outbreaks. Tobacco smoke and other air pollutants appear to worsen symptoms and may prolong the cough. People with a chronic lung disease can also get acute bronchitis, but may need different treatment. How is acute bronchitis treated? Most cases will go away after a few days or a week though the cough may linger for several weeks or months. This indicates that the airways are taking a longer time to heal. As most cases of acute bronchitis are caused by virus’s, antibiotics are usually not effective. -

Laryngotracheitis Caused by COVID-19
Prepublication Release A Curious Case of Croup: Laryngotracheitis Caused by COVID-19 Claire E. Pitstick, DO, Katherine M. Rodriguez, MD, Ashley C. Smith, MD, Haley K. Herman, MD, James F. Hays, MD, Colleen B. Nash, MD, MPH DOI: 10.1542/peds.2020-012179 Journal: Pediatrics Article Type: Case Report Citation: Pitstick CE, Rodriguez KM, Smith AC, Herman HK, Hays JF, Nash CB. A curious case of croup: laryngotracheitis caused by COVID-19. Pediatrics. 2020; doi: 10.1542/peds.2020-012179 This is a prepublication version of an article that has undergone peer review and been accepted for publication but is not the final version of record. This paper may be cited using the DOI and date of access. This paper may contain information that has errors in facts, figures, and statements, and will be corrected in the final published version. The journal is providing an early version of this article to expedite access to this information. The American Academy of Pediatrics, the editors, and authors are not responsible for inaccurate information and data described in this version. Downloaded from©2020 www.aappublications.org/news American Academy by of guest Pediatrics on September 30, 2021 Prepublication Release A Curious Case of Croup: Laryngotracheitis Caused by COVID-19 Claire E. Pitstick, DO, Katherine M. Rodriguez, MD, Ashley C. Smith, MD, Haley K. Herman, MD, James F. Hays, MD, Colleen B. Nash, MD, MPH Affiliations: Rush University Medical Center, Division of Pediatrics, Chicago, Illinois Address Correspondence to: Claire E. Pitstick, Department of Pediatrics, Rush University Medical Center, 1645 W Jackson Blvd Ste 200, Chicago, IL 60612 [[email protected]], 312-942-2200.