Kenya Landscape Analysis for Neglected Tropical Diseases (Ntds), WASH and Behaviour Change 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
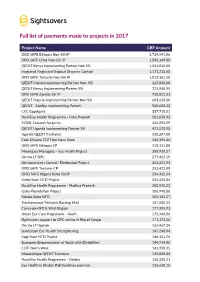
Full List of Payments Made to Projects in 2017
Full list of payments made to projects in 2017 Project Name GBP Amount DfID SAFE Ethiopia Non-SSI IP 3,724,841.06 DfID SAFE Chad Non-SSI IP 1,893,149.00 QEDJT Kenya Implementing Partner Non SSI 1,261,816.00 Inegrated Neglected Tropical Diseases Control 1,171,233.68 DfID SAFE Tanzania Non-SSI IP 1,013,161.50 QEDJT Malawi Implementing Partner Non-SSI 825,000.00 QEDJT Kenya Implementing Partner SSI 721,960.95 DfID SAFE Zambia SSI IP 720,031.31 QEDJT Nigeria Implementing Partner Non SSI 603,658.00 QEDJT - Zambia Implementing Partner 580,608.32 CEC Gopalganj 557,718.51 Rural Eye Health Programme - Uttar Pradesh 501,838.92 87001 Cataract Surgeries 462,293.59 QEDJT Uganda Implementing Partner SSI 421,538.90 Uganda QEDJT Trachoma 380,297.00 Cote D'Ivoire CDTI Northern Zone 340,192.64 DfID SAFE Ethiopia CP 318,111.00 Mwangaza Morogoro – Eye Health Project 289,938.37 Oncho LF DRC 277,423.19 Onchocerciasis Control/ Elimination Project 261,231.91 DfID SAFE Tanzania CP 252,433.00 DFID SAFE Nigeria Kano SSI IP 234,412.34 Kebbi State NTD Project 225,634.84 Rural Eye Health Programme - Madhya Pradesh 208,938.23 Gates Foundation Project 206,998.88 Sokoto State NTD 203,103.27 Trachomatous Trichiasis Backlog Mali 187,888.23 Cameroon NTDs West Region 177,395.91 Urban Eye Care Programme - South 175,348.06 Sightsavers support to OPC-oncho in Rep of Congo 171,173.56 Oncho LF Uganda 165,967.34 Sunderban Eye Health Strengthening 147,240.04 Kogi State NTD Project 146,131.74 Economic Empowerment of Youth with Disabilities 144,914.08 CDTI North West 141,950.35 Mozambique -
Sightsavers-Annual-Review-2012.Pdf
Annual review 2012 Contents President’s welcome 3 Our mission, our methods 4 How we measure our progress 5 How we prevent and cure blindness 7 We invest in training eye health workers and volunteers, in-country 8 We aim to eliminate blinding trachoma from 24 countries 11 We plan on eliminating river blindness from 14 countries 12 We work for long-term change 14 We work to make education accessible to blind children 16 We work towards social inclusion 18 Where we work 20 Bereket and Besufigad Funding innovation 21 Sisay, from Booddachi town in the Oromia Raising our international profile 23 region of Ethiopia both What our supporters say about us 24 suffer from trachoma. Without vital antibiotic Income and expenditure 25 treatment they would both face a future of blindness. A word from our Chief Executive 26 Thank you 27 © Dominic Nahr / Magnum / Sightsavers 2 Annual review 2012 Sightsavers President HRH Princess Alexandra © Dominic Nahr / Magnum / Sightsavers 3 © Zul Mukhida / Sightsavers © Zul The Sightsavers SIM Card Our mission, (Strategy Implementation and Monitoring Card) our methods Sightsavers’ strategy map Our vision: No one is blind from avoidable causes; visually impaired people participate equally in society Sightsavers’ vision is of a Our focus isn’t just on short-term goals – we Our mission: To eliminate avoidable blindness and promote equality of opportunity for disabled people are looking to make long-term change in the world where no one is blind countries where we work. Sightsavers is working with the Kamuli Visually -

Why Water, Sanitation and Hygiene Are Vital for Eliminating Neglected Tropical Diseases
WASH Why water, sanitation and hygiene are vital for eliminating neglected tropical diseases Brief Now is the time to say goodbye to neglected tropical diseases © Sightsavers/Jason Mulikita © Sightsavers/Jason Children from Ngangula Primary School carrying water to school in Chikankata, Zambia. Contents 4 14 Introduction Using WASH data to combat NTDs 5 17 WASH: the facts Social behaviour change communication: the practices that underpin WASH 6 WASH: our key programmes 18 Preparing for the future 8 Working with communities: helping neighbours and friends stay 19 trachoma free References 9 The challenges of delivering WASH 10 Why WASH is worth the investment 11 Encouraging collaboration between the WASH and NTD sectors Cover image 12 Peace Kiende, 11, a student at Developing tools to support Antuaduru Primary School sings a WASH programmes song that helps her remember how to wash her hands and face, as part of the Sightsavers’ WASH project in Meru, Kenya. ©Sightsavers/Andrew Renneisen 3 Introduction In communities where water is scarce, supplies are often reserved for drinking or farming, meaning hygiene and sanitation are sidelined. Poor hygiene is linked to people in people’s habits, community, culture or contracting and spreading bacterial and national tradition, but these practices are parasitic infections, including a number potentially harmful because they help of neglected tropical diseases (NTDs). trachoma and other NTDs to spread. Improving access to clean water, good sanitation and hygiene (often referred Closely linked to some of our WASH work to by the acronym ‘WASH’) is critical in is the WHO-approved ‘SAFE’ strategy preventing and treating these diseases. -

Crafting Alliances
05-Wei-45241.qxd 2/14/2007 5:16 PM Page 191 CHAPTER 5 Crafting Alliances egardless of how successful a social enterprise is at mobilizing funds, most R organizations will inevitably face resource and capacity constraints as a limiting factor to achieving their mission. The resources that any single organi- zation brings to bear on a social problem are often dwarfed by the magnitude and complexity of most social problems. Thus, social entrepreneurs often pursue alliance approaches as a means to mobilizing resources, financial and nonfinan- cial, from the larger context and beyond their own organizational boundaries, to achieve increased mission impact. Social enterprise alliances among nonprofits, nonprofits and business, nonprofits and government, and even across all sectors in the form of tripartite alliances between nonprofit, government, and business have become increasingly common in recent years. Because alliances capitalize on the resources and capacities of more than one organization and capture syn- ergies that would otherwise often go unrealized, they have the potential to gen- erate mission impact far beyond what the individual contributors could achieve independently. This chapter first describes some alliance trends in the social sec- tor and illustrates them with case examples. Next, we introduce a conceptual framework that can be helpful for developing an alliance strategy. Finally, we briefly introduce the chapter’s two case studies, which offer readers an opportu- nity for in-depth analysis of a range of alliance approaches. ALLIANCE TRENDS Increased Competition Increased competition due to a growing number of nonprofits coupled with recent overall declines in social sector funding have contributed to a dramatic 191 05-Wei-45241.qxd 2/14/2007 5:16 PM Page 192 192 Entrepreneurship in the Social Sector increase in the number and form of social enterprise alliances. -

A Nsw Public Health Laboratory Network
A NSW PUBLIC HEALTH LABORATORY NETWORK John Rooney formerly Specialist Medical Adviser AIDS/Infectious Diseases Branch, NSW Health Department ROLES OF DESIGNATED PUBLIC hIEALTH LABORATORIES •Capacity to respond to Statewide public health his article outlines a proposal to establish a Public requirements, including outbreak investigations, in THealth Laboratory Network (PHLN) in NSW, designed conjunction with the N5W Health Department. to meet requirements for high quality public health • Policy development (e.g. as a result of changing laboratory services and laboratory expertise by building on patterns of antibiotic resistance). existing services and facilities. The proposed PHLN, with • Education (e.g. the development and updating of the State's network of Public Health Units and the NSW testing algorithms for general practitioners and public Health Department's AIDS/Infectious Diseases and health practitioners). Environmental Health, Food and Nutrition Branches, will • Providing a Statewide and/or national reference provide an integrated public health service for the laboratory function. surveillance and control of infectious diseases, and the • Coordinating the NSW contribution to State, national capacity to monitor the safety of food arid water and the risk and international laboratory networks to facilitate the of harm from exposure to toxic substances in the collation and analysis of epidemiological data. environment. • Analysis and reporting of Statewide data in conjunction with the NSW Health Department. The PHLN will comprise a network of public health • Providing advice on changes in technology and laboratories formally designated to provide specified opportunities for improved efficiency in the services. Individual laboratories will represent foci of laboratory contribution to public health Statewide expertise in specific public health areas, while in investigations. -
Understanding the Effects of Poor Sanitation on Public Health, the Environment and Well-Being Homa Bay County - Report of Research Findings
Understanding the Effects of Poor Sanitation on Public Health, the Environment and Well-being Homa Bay County - Report of research findings June 2018 Kenya Country Office Ngong Lane, off Ngong Road P.O. Box 30776, 00100 Nairobi, Kenya Tel.: +254 724 463355 Email: [email protected] Executive Summary Poor sanitation is linked to diarrhoeal diseases, which are among the leading causes of morbidity and mortality in children under five. It is also associated with a number of infectious and nutritional outcomes which have great bearing on the health and well-being of the child. This study was conducted to gain more insights into the effects of poor sanitation on public health, the environment and well-being in Homa Bay County. The results of this case-control study show that the majority of adult respondents (the child’s caregiver) were females (85%), with the majority in both the case and control groups (41%) aged 30-39. A small proportion were aged under 19 (2.5% in the control group and 5.4% in the cases). A considerable proportion of respondents had basic education, with 27.5% of the control group and 31.3% of the case group having completed primary school and 18.9% and 15.8% in the control and cases categories respectively having completed secondary school. About 70% of the respondents lived in their own homes and about a quarter were renting (29% controls and 26.7% cases), with most of the homes being either one- or two- More bedroomed. The results suggest a potential link between household poverty and the respondents in incidence of child diarrhoea: the control group households had higher annual incomes than those in the case group and more control families were in the middle wealth the control had quintile than case families. -

The Power of Public Health Surveillance Public Health Approach
DOI: 10.32481/djph.2020.07.016 The Power of Public Health Surveillance Rick Hong, MD; Rebecca Walker, PhD, JD, MSN; Gregory Hovan; Lisa Henry, MHSA; Rick Pescatore, DO Delaware Division of Public Health Never has an emergency battered Delaware to such public health, economic, social, and emotional extremes like the one presented by coronavirus disease 2019 (COVID-19). Strict disease mitigation strategies were led by Governor John Carney’s March 22, 2020 State of Emergency declaration that closed non-essential businesses and schools, and included a Stay-at- Home order. As of June 11, 2020, the state is experiencing fewer hospitalizations and deaths due to COVID-19. The decreasing trends in the percentage of positive COVID-19 cases and hospitalizations1 were the result of many statewide infection control measures such as closures of non-essential businesses, use of face coverings, social distancing, general hand hygiene, and community testing. As Delaware reopens in phases, the Delaware Department of Health and Social Services, Division of Public Health (DPH) – the state’s lead health agency – is conducting public health surveillance. Case investigations and contact tracing have impacted disease transmission rates by identifying those needing isolation or quarantine. These measures will continue as our society moves towards normalcy. Public Health Approach Public health issues are diverse and dynamic, involving many significant public health threats such as infectious diseases, chronic diseases, emergencies, injuries, and environmental health problems.2 A public health concern should be addressed by one consistent approach, similar to an all-hazards response in disaster management regardless of the type of event (Figure 1). -
Public Health Emergency Preparedness and Response Capabilities
Public Health Emergency Preparedness and Response Capabilities National Standards for State, Local, Tribal, and Territorial Public Health Centers for Disease October 2018 Control and Prevention Center for Preparedness Updated January 2019 and Response Table of Contents Introduction . 1. Public Health Emergency Preparedness Cooperative Agreement Program..........................2 Capability Update Initiative ....................................................................3 Using the Capability Standards for Strategic Planning . .7 Public Health Emergency Preparedness and Response Capabilities Planning Model .................7 Phase 1: Assess Current State ...................................................................8 Phase 2: Determine Strategies and Activities.....................................................9 Phase 3: Develop Plans........................................................................10 At-A-Glance: Capability Definitions, Functions, and Summary of Changes . .11 Capability 1: Community Preparedness.........................................................11 Capability 2: Community Recovery.............................................................12 Capability 3: Emergency Operations Coordination ..............................................12 Capability 4: Emergency Public Information and Warning ........................................13 Capability 5: Fatality Management ............................................................13 Capability 6: Information Sharing ..............................................................14 -
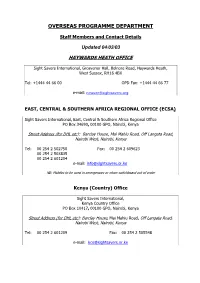
Overseas Programme Department
OVERSEAS PROGRAMME DEPARTMENT Staff Members and Contact Details Updated 04/03/03 HAYWARDS HEATH OFFICE Sight Savers International, Grosvenor Hall, Bolnore Road, Haywards Heath, West Sussex, RH16 4BX Tel: +1444 44 66 00 OPD Fax: +1444 44 66 77 e-mail: [email protected] EAST, CENTRAL & SOUTHERN AFRICA REGIONAL OFFICE (ECSA) Sight Savers International, East, Central & Southern Africa Regional Office PO Box 34690, 00100 GPO, Nairobi, Kenya Street Address (for DHL etc): Barclay House, Mai Mahiu Road, Off Langata Road, Nairobi West, Nairobi, Kenya Tel: 00 254 2 502750 Fax: 00 254 2 609623 00 254 2 503835 00 254 2 601204 e-mail: [email protected] NB: Mobiles to be used in emergencies or when switchboard out of order Kenya (Country) Office Sight Savers International, Kenya Country Office PO Box 10417, 00100 GPO, Nairobi, Kenya Street Address (for DHL etc): Barclay House, Mai Mahiu Road, Off Langata Road, Nairobi West, Nairobi, Kenya Tel: 00 254 2 601209 Fax: 00 254 2 505548 e-mail: [email protected] Malawi Country Office Office Address: Sight Savers International, Malawi Country Office, Area 3/310, Baron Avenue, P/Bag A197, Lilongwe, Malawi Tel: 002651 750453 Fax: 00 2651 750450 002651 758210 e-mail: [email protected] Uganda Office Address: Sight Savers International, 3rd Floor, Colline House, Pilkington Road, Kampala, Uganda Tel: 00 256 41 230299 Fax: 00 256 41 230338 e-mail: [email protected] Tanzania Office Address: Sight Savers International, PO Box 2513, Dar es Salaam, Tanzania Street Address for DHL: Plot No. 327, -

Quality Assessment of an Antimicrobial Resistance Surveillance System in a Province of Nepal
Tropical Medicine and Infectious Disease Article Quality Assessment of an Antimicrobial Resistance Surveillance System in a Province of Nepal Jyoti Acharya 1,* , Maria Zolfo 2 , Wendemagegn Enbiale 3,4, Khine Wut Yee Kyaw 5 , Meika Bhattachan 6, Nisha Rijal 1, Anjana Shrestha 1, Basudha Shrestha 7, Surendra Kumar Madhup 8, Bijendra Raj Raghubanshi 9 , Hari Prasad Kattel 10, Piyush Rajbhandari 11 , Parmananda Bhandari 12, Subhash Thakur 13, Saroj Sharma 14, Dipendra Raman Singh 15 and Runa Jha 1 1 National Public Health Laboratory, Kathmandu 44600, Nepal; [email protected] (N.R.); [email protected] (A.S.); [email protected] (R.J.) 2 Institute of Tropical Medicine, 2000 Antwerp, Belgium; [email protected] 3 Department of Dermatology and Venereology, BahirDar University, 1996 Bahir Dar, Ethiopia; [email protected] 4 Amsterdam UMC, Academic Medical Centre, Department of Dermatology, Amsterdam Institute for Infection and Immunity (AI&I), University of Amsterdam, 7057 Amsterdam, The Netherlands 5 International Union against Tuberculosis and Lung Disease, Paris, France and International Union against Tuberculosis and Lung Disease, Mandalay 11061, Myanmar; [email protected] 6 World Health Organization, Health Emergencies Unit, Kathmandu 44700, Nepal; [email protected] 7 Kathmandu Model Hospital, Kathmandu 44600, Nepal; [email protected] Citation: Acharya, J.; Zolfo, M.; 8 Dhulikhel Hospital, Dhulikhel 45200, Nepal; [email protected] Enbiale, W.; Kyaw, K.W.Y.; 9 KIST Medical College Teaching Hospital, Lalitpur 44700, Nepal; [email protected] Bhattachan, M.; Rijal, N.; Shrestha, A.; 10 Tribhuwan University Teaching Hospital, Kathmandu 44600, Nepal; [email protected] 11 Shrestha, B.; Madhup, S.K.; Patan Hospital, Patan Academy of Health Sciences, Lalitpur 44700, Nepal; [email protected] 12 Raghubanshi, B.R.; et al. -

Orange County Public Health Laboratory QUALITY MANUAL FOR
Orange County Public Health Laboratory QUALITY MANUAL FOR THE WATER QUALITY LABORATORY 600 Shellmaker Road Bldg. A Newport Beach, CA 92660 2018 OCWQL‐Quality Manual Index: 101 Version: 1.0 Page 3 of 42 Table of Contents 1.0 Introduction 2.0 References 3.0 Definitions and Acronyms 4.0 Management Requirements 4.1 Organization 4.2 Management 4.3 Document Control 4.4 Review of Requests, Tenders, and Contracts 4.5 Subcontracting 4.6 Purchasing Services and Supplies 4.7 Service to Client 4.8 Complaints 4.9 Control of Non‐Conforming Events 4.10 Improvement 4.11 Corrective Action 4.12 Preventative Action 4.13 Control of Records 4.14 Internal Audits 4.15 Management Review 4.16 Data integrity Investigations 5.0 Technical Requirements 5.1 General 5.2 Personnel 5.3 Accommodation and Environmental Conditions 5.4 Environmental Methods and Validation 5.5 Calibration 5.6 Measurement Traceability 5.7 Sample Collection 5.8 Sample Handling 5.9 Quality Assurance 5.10 Reporting 6.0 Microbiology Testing 6.1 Introduction 6.2 Scope 6.3 Terms and Definitions 6.4 Method Selection 6.5 Method Validation OCWQL‐Quality Manual Index: 101 Version: 1.0 Page 4 of 42 6.6 Demonstration of Capability (DOC) 6.7 Technical Requirements 7.0 Appendices 7.1 Organization Chart 7.2 List of Test Method SOPs 7.3 Equipment List 7.4 Signatory Sheet 7.5 Personnel Qualification Principle Analyst 7.6 Data Integrity 7.7 Reagent Grade Water 7.8 Change Log OCWQL‐Quality Manual Index: 101 Version: 1.0 Page 5 of 42 1.0 Introduction The Water Quality Laboratory (WQL) is one of five technical areas of the Orange County Public Health Laboratory (OCPHL). -
Policy Guide for Public Health Laboratory Test Service Sharing
Policy Guide for Public Health Laboratory Test Service Sharing Laboratory Efficiencies Initiative April 2014 LABORATORY LEI EFFICIENCIES INITIATIVE Transforming to a Sustainable Public Health Laboratory System Suggested Citation Association of Public Health Laboratories (APHL); Centers for Disease Control and Prevention. Policy guide for public health laboratory test service sharing. Silver Spring, MD: APHL; 2014. Available at: http://www.aphl.org/lei. This report was supported by Cooperative Agreement # U60HM000803 from the Centers for Disease Control and Prevention (CDC) and the Assistant Secretary for Preparedness and Response. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Information in this report does not constitute legal advice. The report is not intended as a substitute for professional or other advice. CONTENTS ABBREVIATIONS USED IN THIS GUIDE ............................................................................................... ii SUMMARY ............................................................................................................................................... 1 1. INTRODUCTION .............................................................................................................................. 3 1.1 The Policy Guide’s Purpose ....................................................................................................... 3 1.2 The Public Health Laboratory