Notes on Black Mamba (Dendroaspis Polylepis) Envenomation Treatment Using the Pressure/ Immobilisation First Aid Technique G.V
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SINGITA SABI SAND, SOUTH AFRICA for the Month of December, Two Thousand and Fifteen
WILDLIFE REPORT SINGITA SABI SAND, SOUTH AFRICA For the month of December, Two Thousand and Fifteen Temperature Rainfall Recorded Sunrise & Sunset Average minimum: 22˚C (71.6˚F) For the month: 36 mm Sunrise 05:05 Average maximum: 34.2˚C (93.6˚F) For the year to date: 286 mm Sunset 18:46 Minimum recorded: 18◦C (64.4˚F) For the season to date: 173.2 mm Maximum recorded: 41˚C (105.8˚F) With a maximum record of 41˚C, the vegetation has been scorched by the hot conditions. Fortunately with the light rain that we did receive it’s allowed some of the flowering plants to blossom. Here's a highlights package of the month's sightings: Hyenas: It's such a joy when hyena cubs are about - they're curios and like to investigate everything around them. Lions: Lion sightings currently could not get any better! Two male lions of the Matimba coalition have been sighted on a few occasions, and they are gradually expanding their current territorial zone north of the river. The Mhangene pride continue to dominate the central area of Singita Sabi Sand. We watched a few interactions between the Majingalane male lions and the sub-adult males of the Mhangene pride that resulted in the young males being dispersed from the pride temporarily. One of the lionesses from the Mhangene pride has been seen with prominent suckle marks indicating that she has given birth. The lionesses has been seen moving in front of the lodges during the early morning and we suspect that the cubs are hidden in the river just east of Boulders Lodge. -

Dendroaspis Viridis
Dendroaspis viridis The western green mamba (Dendroaspis viridis), also known as the West African green mamba or Hallowell's green mamba, is a long, thin, and highly venomous snake of the mamba genus, Dendroaspis. This species was first described in 1844 by the American herpetologist Edward Hallowell. The western green mamba is a fairly large and predominantly arboreal species, capable of navigating through trees swiftly and gracefully. It will also descend to ground level to pursue prey such as rodents and other small mammals. The western green mamba is a very alert, nervous, and extremely agile snake that lives mainly in the coastal tropical rainforest, thicket, Scientific Classification and woodland regions of western Africa. Like all the other mambas, the western green mamba is a highly venomous elapid species. Its Kingdom: Anamalia venom is a highly potent mixture of rapid-acting presynaptic and Phylum: Cordata postsynaptic neurotoxins (dendrotoxins), cardiotoxins and fasciculins. Class: Reptilia Some consider this species to not be a particularly aggressive snake, Order: Squamata but others have suggested that they are extremely nervous and are Suborder: Serpentes prone to attack aggressively when cornered. Conflict with humans is Family: Elapidae low compared to some other species found in the region. Bites to Geunus Dendroaspis people by this species are quite uncommon. Their mortality rate, Species D.Viridis however, is high; many of the recorded bites have been fatal. Rapid progression of severe, life-threatening symptoms are hallmarks of Binomial Name mamba bites. Bites with envenomation can be rapidly fatal. Dendroaspis viridis (Hallowell, 1844)[2] Taxonomy Dendroaspis viridis was first described by the American herpetologist and physician Edward Hallowell in 1844.[2][5] In addition to being called the western green mamba, this species is also commonly known as [6] the West African green mamba or Hallowell's green mamba. -

The Medical Threat of Mamba Envenoming in Sub-Saharan Africa
Downloaded from orbit.dtu.dk on: Oct 06, 2021 The medical threat of mamba envenoming in sub-Saharan Africa revealed by genus- wide analysis of venom composition, toxicity and antivenomics profiling of available antivenoms Ainsworth, Stuart; Petras, Daniel; Engmark, Mikael; Süssmuth, Roderich D.; Whiteley, Gareth; Albulescu, Laura-Oana; Kazandjian, Taline D.; Wagstaff, Simon C.; Rowley, Paul; Wüster, Wolfgang Total number of authors: 16 Published in: Journal of Proteomics Link to article, DOI: 10.1016/j.jprot.2017.08.016 Publication date: 2018 Document Version Peer reviewed version Link back to DTU Orbit Citation (APA): Ainsworth, S., Petras, D., Engmark, M., Süssmuth, R. D., Whiteley, G., Albulescu, L-O., Kazandjian, T. D., Wagstaff, S. C., Rowley, P., Wüster, W., Dorrestein, P. C., Arias, A. S., M. Gutierrez, J., Harrison, R., Casewell, N. R., & Calvete, J. J. (2018). The medical threat of mamba envenoming in sub-Saharan Africa revealed by genus-wide analysis of venom composition, toxicity and antivenomics profiling of available antivenoms. Journal of Proteomics, 172, 173-189. https://doi.org/10.1016/j.jprot.2017.08.016 General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Users may download and print one copy of any publication from the public portal for the purpose of private study or research. You may not further distribute the material or use it for any profit-making activity or commercial gain You may freely distribute the URL identifying the publication in the public portal If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. -
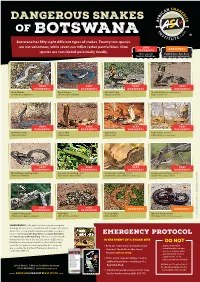
Botswana Has Fifty Eight Different Types of Snakes
DANGEROUS SNAKES OF B OT SWA NA Botswana has fifty eight different types of snakes. Twenty two species are not venomous, while seven can inflict rather painful bites. Nine VERY DANGEROUS species are considered potentially deadly. DANGEROUS Has caused Painful bite, but does human fatalities not require antivenom VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Black Mamba Black Mamba Snouted Cobra Snouted Cobra - banded phase (Dendroaspis polylepis) (Dendroaspis polylepis) (Naja annulifera) (Naja annulifera) VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Anchieta’s Cobra Cape Cobra Cape Cobra Cape Cobra - juvenile (Naja anchietae) (Naja nivea) (Naja nivea) (Naja nivea) Photo Marius Burger VERY VERY VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Mozambique Spitting Cobra Common Boomslang - male Common Boomslang - female Common Boomslang - juvenile (Naja mossambica) (Dispholidus typus viridis) (Dispholidus typus viridis) Photo André Coetzer (Dispholidus typus viridis) VERY VERY DANGEROUS DANGEROUS DANGEROUS DANGEROUS Southern Twig Snake Puff Adder Horned Adder Bibron’s Stiletto Snake (Thelotornis capensis capensis) (Bitis arietans arietans) (Bitis caudalis) (Atractaspis bibronii) Photo Warren Dick © Johan Marais African Snakebite Institute Snakebite African © Johan Marais JOHAN MARAIS is the author of various books on reptiles including the best-seller A Complete Guide to Snakes of Southern Africa. He is a popular public speaker and offers a variety of courses including Snake Awareness, Scorpion Awareness EMERGENCY PROTOCOL and Venomous Snake Handling. Johan is accredited by the International Society of Zoological Sciences (ISZS) and is a IN THE EVENT OF A SNAKE BITE Field Guides Association of Southern Africa (FGASA) and DO NOT ww Travel Doctor-approved service provider. His courses are 1 Keep the victim calm, immobilized and .. -

Zambia & Malawi
Zambia & Malawi - The Best of Africa Naturetrek Tour Report 2 - 9 October 2016 Red-billed Oxpeckers on Kudu in middle of breeding herd of Elephants Red-necked Spurfowl Looking at African Skimmers near Mwalasi Enjoying Sable Antelopes Report and images by Samuel Lenard Chihana Naturetrek Mingledown Barn Wolf's Lane Chawton Alton Hampshire GU34 3HJ UK T: +44 (0)1962 733051 E: [email protected] W: www.naturetrek.co.uk Tour Report Zambia & Malawi - The Best of Africa Tour participants: Samuel Lenard Chihana (Local Guide) with four Naturetrek Clients Please note that this tour report only covers the first part of the tour, in Malawi, that was led by Samuel Lenard Chihana. We do not have reports from the other Local Guides. Day 1 Sunday 2nd October In flight to Kamuzu International Airport. Day 2 Monday 3rd October Weather: overcast and cloudy. We met at Kamuzu International Airport and, having sorted immigration formalities, changed their money and loaded the vehicle, we started our drive to Mvuu around 2.35pm. Along a Forest Reserve at Linthipe I offered them a packed lunch and they had an opportunity to walk around and stretch their legs. During our lunch break we saw Southern Citril and Bronze Manikin, flying and perched. On our way from the airport and just before stopping we saw Pied Crows, Lilac-breasted Rollers and House Sparrows. We also saw White-necked Ravens as we passed Dedza. We arrived at around 7.45pm. I gave them a briefing during check in, mentioning all activities offered in the Camp, including Village Tours, Rhino tracking, Sanctuary Drives and Hides, Help Malawi and School Visiting, and also the opportunity to visit or participate in Bat or Carnivore Research, if interested. -

Seven Day Rwanda Birding and Nature Tour- Customized
AVIAN SAFARIS Seven Day Rwanda Birding and Nature Tour- Customized February 18 to 24, 2018 Tour Leader: Crammy Wanyama Trip Report and Photos By Crammy Wanyama Red-throated ALethe – One of The Albertine Rift Endemics Seen Rwanda, a very small country located in the heart of Africa, has become a darling to many world travellers in a very shot time. The reasons for this quick development will be noticed without a single explanation! A beautiful country gifted in several aspects; very welcoming people with some of the most honest smiles you can imagine, panoramic views of impressive mountain ranges and water bodies some of which earn her, her popular identity as “The Land of a Thousand Hills”, this is also one of the only three homes of Mountain Gorillas and the actual place where the famous Dian Fossey based her studies that attracted the world’s Avian Safaris: Email: [email protected] Website: http://www.aviansafaris.com AVIAN SAFARIS attention to these endangered apes. Rwanda is a birder’s heaven, the diversity of habitats here host some of the most sought after birds on the continent, a prime example are the albertine rift ranges which harbor several of the regional endemics and yet the local authority does good maintenance of designated trails that make it easy to find them. Ian and myself had the pleasure to enjoy this country, from Kigali its very beautiful and 3rd world most green city in the world, to Akagera National Park the jewel of the east and Nyungwe forest the incomparable home to the Albertine Rift endemics. -

Presentation Title
World Environment Day 2017 World Environment Day 2017 THEME: Connecting People to Nature THEME:Tool Box Wastewater Talk VeoliaTool Middle Box Talk East Veolia Middle East Each World Environment Day is organized around a theme that focuses attention on a particularly pressing environmental concern. The theme for 2017, ‘Connecting People to Nature’, urges us to get outdoors and into nature, to appreciate its beauty and to think about how we are part of nature and how intimately we depend on it. It challenges us to find fun and exciting ways to experience and cherish this vital relationship. Nature’s gifts are often hard to value in monetary terms. Like clean air, they are often Billions of rural people around the world spend every taken for granted, at least until they become working day ‘connected to nature’ and appreciate full well scarce. However, economists are developing their dependence on natural water supplies and how nature ways to measure the multi-trillion-dollar worth provides their livelihoods in the form of fertile soil. They are of many so-called ‘ecosystem services’, from among the first to suffer when ecosystems are threatened, insects pollinating fruit trees to the leisure, whether by pollution, climate change or over-exploitation. health and spiritual benefits of a hike up a valley. WATCH THESE VIDEOS !!! Click on images The Veolia Tool Kit for World Environment Day is to raise awareness on the environment and biodiversity protection! Station 1 • Veolia & the Environment The idea is an Interactive Roadshow/Workshop Format with different Station 2 • Protected areas in the region people at each station to present the subject: • Each has a station and presents the different facts, devices and challenges • Teams walk around the stations and Station 3 • Game - Animal per nationality speak to each of the stations Station 4 • How can you help ? There are about 1500 protected areas in the 22 countries of the region (Middle East & North Africa), but only five countries have protected more than 10% of their land. -

2008 Trip Report KENYA
KENYA TRIP REPORT AUGUST 2008 August 1 / LAKE NAIVASHA & NAIVASHA COUNTRY CLUB I awoke to a steady drizzle that accompanied me on our journey through Nairobi and to the Longonot Escarpment which begins the descent to the Rift Valley 1500’ below. At least it was clear enough so one could see a good distance across the valley but the skies remained heavily overcast. A lorry failed to negotiate a bend and was on its side but there was enough room for one lane to get by. Once on the valley floor Pied Crows and Cape Rooks became common roadside birds, and in one place they were feeding on a pair of road kill hyenas. In a wheat field 3 Secretary Birds, terrestrial feeding raptors, kept their distance from each other and worked the rows searching for something to eat. Once we reached the entrance to the Naivasha Country Club a Bronzed Sunbird was busy feeding on Leonotis flower heads. Kenya Rufous Sparrows and Streaky Seedeaters were amongst the short grasses while a Rufous-naped Lark was singing from on top of a stalk. In the car park one was immediately struck by all the different colors of the bougainvillea bushes. A Tropical Boubou was collecting nesting material and a White- headed Barbet and Red-eyed Doves were quite happy feeding in a berry tree as a Red-chested Cuckoo’s 3-noted calls rang out from the top of a Yellow-barked Acacia, locally known as a fever tree. Once on the manicured lawns of the grounds Sacred Ibis wander about as peacocks would on an estate and Superb Starlings are constantly busy moving about from the lawn to the lower tree branches. -

Report of the Presence of Wild Animals
Report of the Presence of Wild Animals The information recorded here is essential to emergency services personnel so that they may protect themselves and your neighbors, provide for the safety of your animals, ensure the maximum protection and preservation of your property, and provide you with emergency services without unnecessary delay. Every person in New York State, who owns, possesses, or harbors a wild animal, as set forth in General Municipal Law §209-cc, must file this Report annually, on or before April 1, of each year, with the clerk of the city, village or town (if outside a village) where the animal is kept. A list of the common names of animals to be reported is enclosed with this form. Failure to file as required will subject you to penalties under law. A separate Report is required to be filed annually for each address where a wild animal is harbored. Exemptions: Pet dealers, as defined in section 752-a of the General Business Law, zoological facilities and other exhibitors licensed pursuant to U.S. Code Title 7 Chapter 54 Sections 2132, 2133 and 2134, and licensed veterinarians in temporary possession of dangerous dogs, are not required to file this report. Instructions for completing this form: 1. Please print or type all information, using blue or black ink. 2. Fill in the information requested on this page. 3. On the continuation sheets, fill in the information requested for each type of animal that you possess. 4. Return the completed forms to the city, town, or village clerk of each municipality where the animal or animals are owned, possessed or harbored. -

Southern Tanzania: Endemic Birds & Spectacular Mammals
SOUTHERN TANZANIA: ENDEMIC BIRDS & SPECTACULAR MAMMALS SEPTEMBER 18–OCTOBER 6, 2018 Tanzanian Red-billed Hornbill © Kevin J. Zimmer LEADERS: KEVIN ZIMMER & ANTHONY RAFAEL LIST COMPILED BY: KEVIN ZIMMER VICTOR EMANUEL NATURE TOURS, INC. 2525 WALLINGWOOD DRIVE, SUITE 1003 AUSTIN, TEXAS 78746 WWW.VENTBIRD.COM SOUTHERN TANZANIA: ENDEMIC BIRDS & SPECTACULAR MAMMALS September 18–October 6, 2018 By Kevin Zimmer After meeting in Dar es Salaam, we kicked off our inaugural Southern Tanzania tour by taking a small charter flight to Ruaha National Park, at 7,800 square miles, the largest national park in all of east Africa. The scenery from the air was spectacular, particularly on our approach to the park’s airstrip. Our tour was deliberately timed to coincide with the dry season, a time when many of the trees have dropped their leaves, heightening visibility and leaving the landscapes starkly beautiful. This is also a time when the Great Ruaha River and its many smaller tributaries dwindle to shallow, often intermittent “sand rivers,” which, nonetheless, provide natural game corridors and concentration points for birds during a time in which water is at a premium. Bateleur, Ruaha National Park, Sept 2018 (© Kevin J. Zimmer) After touching down at the airstrip, we disembarked to find our trusty drivers, Geitan Ndunguru and Roger Mwengi, each of them longtime friends from our Northern Tanzania tours, waiting for us with their safari vehicles ready for action. The first order of business was to head to the lodge for lunch, but a large, mixed-species coven of Victor Emanuel Nature Tours 2 Southern Tanzania, 2018 vultures could not be ignored, particularly once we discovered the reason for the assemblage—a dead Hippo, no doubt taken down the previous night as it attempted to cross from one river to another, and, the sated Lion that had been gorging itself ever since. -

Namibia:Rugged Mountains, Living Deserts, and Etosha
Tropical Birding Trip Report NAMIBIA NOVEMBER, 2017 Namibia: Rugged Mountains, Living Deserts, and Etosha 1 - 16 November, 2017 TOUR LEADER: Charley Hesse Report & photos by Charley Hesse. Namibia evokes images of dry, barren landscapes, and this is in part true, but many of these are incredibly scenic and remarkeably full of life. We visited several distinct ecotypes, from the dry, Kalahari scrub and thornveld of the Khomas Hochland plateau, to rocky edges to the escarpment, and from the ancient, dune-filled Namib Desert to the dry open plains of Etosha National Park. We tracked down Namibia’s only geopolitical endemic, the Dune Lark at Sossusvlei, the endangered Hartemann’s Mountain Zebra crossing the Namib desert, and the charismatic near- endemic Rockrunner and White-tailed Shrike in the stunning Erongo Mountains. We found the iconic Welwitschia mirabilis (practically a living fossil) and enjoyed the mysterious rock engravings at Twyfelfontein. We delved into the fascinating culture of the Himba tribe in the neighbouring Kaokoland, and for a grand finale, we experienced the amazing Etosha National Park with its associated megafauna. As well as sightings of lions. leopards and elephants galore, we enjoyed the unique photographic opportunities of some wonderful birdlife. It was truly an unforgettable trip. www.tropicalbirding.com +1-409-515-9110 [email protected] Tropical Birding Trip Report NAMIBIA NOVEMBER, 2017 1st November – Arrival in Windhoek On the arrival day in Windhoek, we had a short stroll near our hotel. The name of which was the local name for Helmeted Guineafowl, and there were a dozen running around just outside the gate. -

The Heart of the Savannah Comic Book
ANIMAL FACTS Cheetah (Acinonyx jubatus): AGE RANGE: 10-14 years in wild. IUCN RED LIST: Vulnerable. FEATURES: Small, rounded head on a long neck; a flexible spine, deep chest, special feet pads for traction, and a Top speeds of up to 80 miles long tail for balance. per hour. DIET: Gazelle, impala, antelope, hares, The only feline with non- and small birds. retractable claws, which helps PREDATORS: Humans, leopard, eagle, with traction. hyena, and lion. The black "tear tracks" running from the inside corner of each eye to the mouth serves to protect the eyes Lion (Panthera leo): from sunlight. AGE RANGE: 10-18 years in the wild. IUCN RED LIST: Vulnerable. FEATURES: Mane around the head and neck, deep chest, strong legs and canines, and special feet pads for traction. Second largest living big cat DIET: Wilderbeest, zebra, antelope, after the tiger. and impala. Manes on male lions darken PREDATORS: Humans, hyena, leopard, with age- a thicker and darker and jackal. mane signifies a healthy feline. Lionesses do not have manes. Its roar can be heard from over 5 miles away. Thomson's Gazelle (Gazella thomsonii): AGE RANGE: 10-11 years in the wild. IUCN RED LIST: Least concern. FEATURES: Light coat with dark stripes, white patch on the rump underneath tail, and males have ridged horns that curve backwards. Fourth fastest land animal DIET: Leaves, stems, herbs, short with top speeds of up to 55 grasses, and shoots. miles per hour. PREDATORS: Humans, cheetah, hyena, Females can have shorter lion, and leopard. horns or none at all. Most common gazelle species in East Africa.