203255Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Signifor, INN-Pasireotide
Package leaflet: Information for the user Signifor 10 mg powder and solvent for suspension for injection Signifor 20 mg powder and solvent for suspension for injection Signifor 30 mg powder and solvent for suspension for injection Signifor 40 mg powder and solvent for suspension for injection Signifor 60 mg powder and solvent for suspension for injection pasireotide Read all of this leaflet carefully before you start using this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor, nurse or pharmacist. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor, nurse or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Signifor is and what it is used for 2. What you need to know before you use Signifor 3. How to use Signifor 4. Possible side effects 5. How to store Signifor 6. Contents of the pack and other information 1. What Signifor is and what it is used for Signifor is a medicine that contains the active substance pasireotide. It is used to treat acromegaly in adult patients. It is also used to treat Cushing’s disease in adult patients for whom surgery is not an option or for whom surgery has failed. Acromegaly Acromegaly is caused by a type of tumour called a pituitary adenoma which develops in the pituitary gland at the base of the brain. -

GHRH Excess and Blockade in X-LAG Syndrome
A F Daly, P A Lysy, GHRH in X-LAG syndrome 23:3 161–170 Research C Desfilles et al. GHRH excess and blockade in X-LAG syndrome Adrian F Daly1,*, Philippe A Lysy3,*,Ce´line Desfilles5,6,*, Liliya Rostomyan1, Amira Mohamed5,6, Jean-Hubert Caberg2, Veronique Raverot8, Emilie Castermans2, Etienne Marbaix4, Dominique Maiter9, Chloe Brunelle3, Giampaolo Trivellin7, Constantine A Stratakis7, Vincent Bours2, Christian Raftopoulos10, Veronique Beauloye3, Anne Barlier5,6 and Albert Beckers1 1Department of Endocrinology, Centre Hospitalier Universitaire de Lie` ge, University of Lie` ge, Domaine Universitaire du Sart-Tilman, 4000 Lie` ge, Belgium 2Department of Human Genetics, Centre Hospitalier Universitaire de Lie` ge, University of Lie` ge, Domaine Universitaire du Sart-Tilman, 4000 Lie` ge, Belgium 3Pediatric Endocrinology Unit, Universite´ Catholique de Louvain, Avenue Hippocrate 10, 1200 Brussels, Belgium 4Cliniques Universitaires Saint Luc and Department of Pathology, Universite´ Catholique de Louvain, Avenue Hippocrate 10, 1200 Brussels, Belgium 5Laboratory of Molecular Biology, APHM, Hoˆ pital la Conception, 13385, Marseille, France 6Aix Marseille Universite´ , CRNS, CRN2M-UMR 7286, 13344, Marseille, France 7Section on Endocrinology and Genetics, Program on Developmental Endocrinology and Genetics (PDEGEN) and Pediatric Endocrinology Inter-institute Training Program, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), National Institutes of Health (NIH), Bethesda, Maryland 20892, USA 8Laboratoire d’Hormonologie -
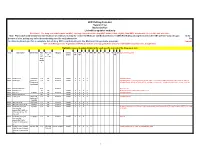
Drug Code List
HCPCS/Drug Code List Version 13.2 Revised 6/1/21 List will be updated routinely Disclaimer: For drug codes that require an NDC, coverage depends on the drug NDC status (rebate eligible, Non-DESI, non-termed, etc) on the date of service. Note: Physician/Facility-administered medications are reimbursed using the Centers for Medicare and Medicaid Services (CMS) Part B Drug pricing file found on the CMS website--www.cms.gov. In the absence of a fee, pricing may reflect the methodolgy used for retail pharmacies. Go to data.medicaid.gov for a complete list of drug NDCs participating in the Medicaid drug rebate program. Consult with each Managed Care Organization (MCO) about their coverage guidelines and prior authroization requirements, if applicable. Highlights represent updated material for each specific revision of the Drug Code List. Code Description Brand Name NDC NDC unit Category Service AC CAH P NP MW MH HS PO OPH HI ID DC Special Instructions req. of Limits OP OP TF for measure drug rebate ? 90281 human ig, im Gamastan Yes ML Antisera NONE X X X X Closed 3/31/13. 90283 human ig, iv Gamimune, Yes ML Antisera NONE X X X X Closed 3/31/13. Cost invoice required with claim. Restricted to ICD-9 diagnoses codes 204.10 - 204.12, Flebogamma, 279.02, 279.04, 279.06, 279.12, 287.31, and 446.1, and must be included on claim form, effective 10/1/09. Gammagard 90287 botulinum antitoxin N/A Antisera Not Covered 90288 botulism ig, iv No ML NONE X X X X Requires documentation and medical review 90291 cmv ig, iv Cytogam Yes ML Antisera NONE X X X X Closed 3/31/13. -

Pharmacological Management of Acromegaly: a Current Perspective
Neurosurg Focus 29 (4):E14, 2010 Pharmacological management of acromegaly: a current perspective SUNIL MANJILA , M.D.,1 Osmo N D C. WU, B.A.,1 FAH D R. KHAN , M.D., M.S.E.,1 ME H ree N M. KHAN , M.D.,2 BAHA M. AR A F AH , M.D.,2 AN D WA rre N R. SE L M AN , M.D.1 1Department of Neurological Surgery, The Neurological Institute, and 2Division of Clinical and Molecular Endocrinology, University Hospitals Case Medical Center, Cleveland, Ohio Acromegaly is a chronic disorder of enhanced growth hormone (GH) secretion and elevated insulin-like growth factor–I (IGF-I) levels, the most frequent cause of which is a pituitary adenoma. Persistently elevated GH and IGF-I levels lead to substantial morbidity and mortality. Treatment goals include complete removal of the tumor causing the disease, symptomatic relief, reduction of multisystem complications, and control of local mass effect. While trans- sphenoidal tumor resection is considered first-line treatment of patients in whom a surgical cure can be expected, pharmacological therapy is playing an increased role in the armamentarium against acromegaly in patients unsuitable for or refusing surgery, after failure of surgical treatment (inadequate resection, cavernous sinus invasion, or transcap- sular intraarachnoid invasion), or in select cases as primary treatment. Three broad drug classes are available for the treatment of acromegaly: somatostatin analogs, dopamine agonists, and GH receptor antagonists. Somatostatin analogs are considered as the first-line pharmacological treatment of acromegaly, although effica- cy varies among the different formulations. Octreotide long-acting release (LAR) appears to be more efficacious than lanreotide sustained release (SR). -

To Download a List of Prescription Drugs Requiring Prior Authorization
Essential Health Benefits Standard Specialty PA and QL List July 2016 The following products require prior authorization. In addition, there may be quantity limits for these drugs, which is notated below. Therapeutic Category Drug Name Quantity Limit Anti-infectives Antiretrovirals, HIV SELZENTRY (maraviroc) None Cardiology Antilipemic JUXTAPID (lomitapide) 1 tab/day PRALUENT (alirocumab) 2 syringes/28 days REPATHA (evolocumab) 3 syringes/28 days Pulmonary Arterial Hypertension ADCIRCA (tadalafil) 2 tabs/day ADEMPAS (riociguat) 3 tabs/day FLOLAN (epoprostenol) None LETAIRIS (ambrisentan) 1 tab/day OPSUMIT (macitentan) 1 tab/day ORENITRAM (treprostinil diolamine) None REMODULIN (treprostinil) None REVATIO (sildenafil) Soln None REVATIO (sildenafil) Tabs 3 tabs/day TRACLEER (bosentan) 2 tabs/day TYVASO (treprostinil) 1 ampule/day UPTRAVI (selexipag) 2 tabs/day UPTRAVI (selexipag) Pack 2 packs/year VELETRI (epoprostenol) None VENTAVIS (iloprost) 9 ampules/day Central Nervous System Anticonvulsants SABRIL (vigabatrin) pack None Depressant XYREM (sodium oxybate) 3 bottles (540 mL)/30 days Neurotoxins BOTOX (onabotulinumtoxinA) None DYSPORT (abobotulinumtoxinA) None MYOBLOC (rimabotulinumtoxinB) None XEOMIN (incobotulinumtoxinA) None Parkinson's APOKYN (apomorphine) 20 cartridges/30 days Sleep Disorder HETLIOZ (tasimelteon) 1 cap/day Dermatology Alkylating Agents VALCHLOR (mechlorethamine) Gel None Electrolyte & Renal Agents Diuretics KEVEYIS (dichlorphenamide) 4 tabs/day Endocrinology & Metabolism Gonadotropins ELIGARD (leuprolide) 22.5 mg -

Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future
International Journal of Molecular Sciences Review Somatostatin Analogues in the Treatment of Neuroendocrine Tumors: Past, Present and Future Anna Kathrin Stueven 1, Antonin Kayser 1, Christoph Wetz 2, Holger Amthauer 2, Alexander Wree 1, Frank Tacke 1, Bertram Wiedenmann 1, Christoph Roderburg 1,* and Henning Jann 1 1 Charité, Campus Virchow Klinikum and Charité, Campus Mitte, Department of Hepatology and Gastroenterology, Universitätsmedizin Berlin, 10117 Berlin, Germany; [email protected] (A.K.S.); [email protected] (A.K.); [email protected] (A.W.); [email protected] (F.T.); [email protected] (B.W.); [email protected] (H.J.) 2 Charité, Campus Virchow Klinikum and Charité, Campus Mitte, Department of Nuclear Medicine, Universitätsmedizin Berlin, 10117 Berlin, Germany; [email protected] (C.W.); [email protected] (H.A.) * Correspondence: [email protected]; Tel.: +49-30-450-553022 Received: 3 May 2019; Accepted: 19 June 2019; Published: 22 June 2019 Abstract: In recent decades, the incidence of neuroendocrine tumors (NETs) has steadily increased. Due to the slow-growing nature of these tumors and the lack of early symptoms, most cases are diagnosed at advanced stages, when curative treatment options are no longer available. Prognosis and survival of patients with NETs are determined by the location of the primary lesion, biochemical functional status, differentiation, initial staging, and response to treatment. Somatostatin analogue (SSA) therapy has been a mainstay of antisecretory therapy in functioning neuroendocrine tumors, which cause various clinical symptoms depending on hormonal hypersecretion. Beyond symptomatic management, recent research demonstrates that SSAs exert antiproliferative effects and inhibit tumor growth via the somatostatin receptor 2 (SSTR2). -

Regulatory Mechanisms of Somatostatin Expression
International Journal of Molecular Sciences Review Regulatory Mechanisms of Somatostatin Expression Emmanuel Ampofo * , Lisa Nalbach, Michael D. Menger and Matthias W. Laschke Institute for Clinical & Experimental Surgery, Saarland University, 66421 Homburg/Saar, Germany; [email protected] (L.N.); [email protected] (M.D.M.); [email protected] (M.W.L.) * Correspondence: [email protected]; Tel.: +49-6841-162-6561; Fax: +49-6841-162-6553 Received: 25 May 2020; Accepted: 9 June 2020; Published: 11 June 2020 Abstract: Somatostatin is a peptide hormone, which most commonly is produced by endocrine cells and the central nervous system. In mammals, somatostatin originates from pre-prosomatostatin and is processed to a shorter form, i.e., somatostatin-14, and a longer form, i.e., somatostatin-28. The two peptides repress growth hormone secretion and are involved in the regulation of glucagon and insulin synthesis in the pancreas. In recent years, the processing and secretion of somatostatin have been studied intensively. However, little attention has been paid to the regulatory mechanisms that control its expression. This review provides an up-to-date overview of these mechanisms. In particular, it focuses on the role of enhancers and silencers within the promoter region as well as on the binding of modulatory transcription factors to these elements. Moreover, it addresses extracellular factors, which trigger key signaling pathways, leading to an enhanced somatostatin expression in health and disease. Keywords: somatostatin; pre-prosomatostatin; δ-cells; central nervous system (CNS); gut; hypothalamus; cAMP resonse element (CRE); pancreas/duodenum homeobox protein (PDX)1; paired box protein (PAX)6; growth hormone (GH); brain-derived neurotrophic factor (BDNF); glutamateric system; pancreas 1. -

Hypothalamic-Pituitary Axes
Hypothalamic-Pituitary Axes Hypothalamic Factors Releasing/Inhibiting Pituitary Anterior Pituitary Hormones Circulating ACTH PRL GH Hormones February 11, 2008 LH FSH TSH Posterior Target Pituitary Gland and Hormones Tissue Effects ADH, oxytocin The GH/IGF-I Axis Growth Hormone Somatostatin GHRH Hypothalamus • Synthesized in the anterior lobe of the pituitary gland in somatotroph cells PITUITARY • ~75% of GH in the pituitary and in circulation is Ghrelin 191 amino acid single chain peptide, 2 intra-molecular disulfide bonds GH Weight; 22kD • Amount of GH secreted: IGF-I Women: 500 µg/m2/day Synthesis IGF- I Men: 350 µg/m2/day LIVER Local IGF-I Synthesis CIRCULATION GH Secretion: Primarily Pulsatile Pattern of GH Secretion Regulation by two hypothalamic in a Healthy Adult hormones 25 Sleep 20 Growth - SMS Hormone 15 Somatostatin Releasing GHRH + GH (µg/L) Hormone Inhibitory of 10 Stimulatory of GH Secretion GH Secretion 05 0 GHRH induces GH Somatostatin: Decreases to allow 0900 2100 0900 synthesis and secretion Clocktime GH secretory in somatotrophs Bursts GH From: “Acromegaly” by Alan G. Harris, M.D. 1 Other Physiological Regulators of GH Secretion Pharmacologic Agents Used to Stimulate GH Secretion Amino Sleep Exercise Stress Acids Fasting Glucose Stimulate hypothalamic GHRH or Inhibit Somatostatin Hypothalamus GHRH SMS Hypoglycemia(Insulin) Pituitary L-dopa Arginine Clonidine GHRH + - SMS Pyridostigmine GH Target Tissues Metabolic & Growth Promoting GH Effects IGF-I Insulin-like growth factor I (IGF-I) Major Determinants of Circulating -

And Signifor LAR (Pasireotide) Prior Authorization with Quantity Limit
Signifor (pasireotide) and Signifor LAR (pasireotide) Prior Authorization with Quantity Limit Program Summary Signi for is the only target in this prior authorization program. Signifor LAR is not targeted in this pharmacy prior authorization program. This program applies to Commercial, NetResults A series, SourceRx, and Health Insurance Marketplace formularies. OBJECTIVE The intent of the Signifor (pasireotide) and Signifor LAR Prior Authorization (PA) program is to appropriately select patients for treatment according to product labeling and/or clinical studies and/or clinical practice guidelines. The program will approve for doses within the set limit. Doses above the set limit will be approved if the requested quantity is below the FDA limit and cannot be dose optimized or when the quantity is above the FDA limit and the prescriber has submitted documentation in support of therapy with a higher dose for the intended diagnosis. TARGET DRUGS Signifor (pasireotide) PRIOR AUTHORIZATION CRITERIA FOR APPROVAL Initial Evaluation Signifor will be approved for INITIAL USE when ALL of the following are met: 1. If Signifor, ONE of the following: A. The patient has a diagnosis of Cushing’s disease and ONE of the following: I. The patient has had recurrence or persistence after pituitary surgical resection OR II. The patient is not a candidate for pituitary surgical resection OR B. The patient has another FDA approved diagnosis AND 2. If Signifor LAR, ONE of the following: A. The patient has a diagnosis of acromegaly and ONE of the following: I. The use of requested agent is for adjunctive therapy with irradiation to alleviate acromegaly symptoms OR II. -

A Comparison Between Octreotide-LAR and Lanreotide-SR in the Chronic Treatment of Acromegaly
European Journal of Endocrinology (1999) 141 267–271 ISSN 0804-4643 CLINICAL STUDY A comparison between octreotide-LAR and lanreotide-SR in the chronic treatment of acromegaly R Cozzi, D Dallabonzana, R Attanasio, M Barausse and G Oppizzi Division of Endocrinology, Niguarda Hospital, Milan, Italy (Correspondence should be addressed to R Cozzi, Division of Endocrinology, Ospedale Niguarda, Piazza Ospedale Maggiore 3, I-20162 Milano, Italy; Email: [email protected]) Abstract Background: At present long-acting somatostatin analogs represent the first-line medical treatment of acromegaly. These drugs produce stable suppression of GH in most sensitive patients and IGF-I normalization in many; they also increase the compliance of acromegalic patients. The recent availability of octreotide (OC)-LAR, a somatostatin analog to be administered at 28-day intervals, has prompted us to compare, in the same group of patients, its effects and those of another somatostatin analog already available, lanreotide-SR (LSR, to be administered at 14-day intervals). Patients: Twelve somatostatin analog-sensitive acromegalic patients with active disease were enrolled in a prospective open sequential study after giving their informed consent. After chronic treatment with LSR (6–24 months), the patients were changed to treatment with OC-LAR, without wash-out. LSR had been administered at individually tailored dosages (30 mg i.m. at 7–21-day intervals, median 10 days – every 7 days in seven patients, 10 days in two patients, 14 days in two patients and 21 days in one patient) according to GH and IGF-I responses. Disease stability was obtained, as shown by maximal GH/IGF-I suppression without any significant hormonal change between the last two control measurements. -

Developing Synthetic Peptide-Based Inhibitors of Human Growth Hormone Receptor
Developing Synthetic Peptide-Based Inhibitors of Human Growth Hormone Receptor A Thesis Presented to The Honors Tutorial College Ohio University In Partial Fulfillment of the Requirements for Graduation from the Honors Tutorial College with the degree of Bachelor of Science in Chemistry by Maya R. Sattler May 2018 2 Acknowledgements This thesis represents the work a large number of people, to whom I am incredibly grateful. Thank you first and foremost to my adviser, Dr. Justin Holub, whose patience and teaching has been outstanding for the entire three years I have worked with him and been his student, all the way to the final deadline. Thank you to Dr. John Kopchick for allowing me the opportunity to explore a different area of research and a different laboratory environment. Both Dr. Lauren McMills and Dean Cary Frith have offered wonderful support and guidance through my entire HTC career and I will forever be appreciative. There are also many fellow students that have helped me with work and encouragement. Thank you to my fellow students in the Holub laboratory, especially Najah Alqaeisoom who was my first teacher and a delight to work with, and Danushka Arachchige who was always willing to help, no matter the problem. I would also like to thank my colleagues at Edison Biotechnology Institute for their support in all things trivial and otherwise. Dr. Reetobrata Basu in particular made all of the cell work possible through his teaching, assistance, and reassurances. Lastly, I am grateful to a larger community of people in Athens and worldwide that helped me through my four years of undergraduate studies and will continue to support me as I continue to progress. -

SIGNIFOR LAR for Injectable Suspension: 10 Mg, 20 Mg, 30 Mg, 40 Mg, and SIGNIFOR LAR Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------DOSAGE FORMS AND STRENGTHS------------------- These highlights do not include all the information needed to use SIGNIFOR LAR for injectable suspension: 10 mg, 20 mg, 30 mg, 40 mg, and SIGNIFOR LAR safely and effectively. See full prescribing information 60 mg, powder in a vial to be reconstituted with the provided 2 mL diluent. for SIGNIFOR LAR. (3) SIGNIFOR® LAR (pasireotide) for injectable suspension, for -------------------------------CONTRAINDICATIONS------------------------------ intramuscular use None. (4) Initial U.S. Approval: 2012 ---------------------------WARNINGS AND PRECAUTIONS-------------------- ------------------------RECENT MAJOR CHANGES------------------------------ • Hyperglycemia and Diabetes: Sometimes severe. Monitor glucose levels Indications and Usage , Cushing’s Disease (1.2) 6/2018 periodically during therapy. Monitor glucose levels more frequently in the Dosage and Adminisration (2) 6/2018 months that follow initiation or discontinuation of SIGNIFOR LAR Warnings and Precautions (5) 6/2018 therapy and following SIGNIFOR LAR dose adjustment. Use anti-diabetic treatment if indicated per standard of care. (2.1, 5.1) --------------------------INDICATIONS AND USAGE----------------------------- SIGNIFOR LAR is a somatostatin analog indicated for the treatment of: • Bradycardia and QT Prolongation: Use with caution in at-risk patients; • Patients with acromegaly who have had an inadequate response to surgery Evaluate ECG and electrolytes prior to dosing and periodically while on and/or for whom surgery is not an option. (1.1) treatment. (2.1, 5.2, 7.1) • Patients with Cushing’s disease for whom pituitary surgery is not an option • Liver Test Elevations: Evaluate liver enzyme tests prior to and during or has not been curative (1.2). treatment. (2.1, 5.3) -----------------------DOSAGE AND ADMINISTRATION----------------------- • Cholelithiasis: Monitor periodically.