Epigenome-Wide Association of Myocardial Infarction with DNA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Publ 45637 Issue Ch2 Page 27
Now I’m a Phase, Now I’m Not a Phase: On the Variability of Phases with Extraction and Ellipsis äeljko Bo'kovic´ On the basis of a number of cases where the status of X with respect to phasehood changes depending on the syntactic context in which X occurs, I argue for a contextual approach to phasehood whereby the highest phrase in the extended projection of all lexical categories—N, P, A, and V (passive and active)—functions as a phase. The relevant arguments concern extraction and ellipsis. I argue that ellipsis is phase- constrained: only phases and complements of phase heads can in prin- ciple undergo ellipsis. I show that A¯ -extraction out of an ellipsis site is possible only if the ellipsis site corresponds to a phasal complement. I also provide evidence for the existence of several AspectPs, all of which have morphological manifestations, in the VP domain of English and show that they crucially affect the phasehood of this domain. The article provides a uniform account of a number of superficially dif- ferent constructions involving extraction and ellipsis from Serbo- Croatian, Japanese, Turkish, and English. Keywords: phases, locality of movement, NP, ellipsis, numerals, aspect, P-stranding 1 Introduction This article addresses the central question of the theory of phases: what counts as a phase. On Chomsky’s (2000, 2001) approach, phasehood is in a sense rigid: the phasal status of a category does not depend on its syntactic context; thus, CPs and vPs are always phases.1 This runs counter to the spirit of the Minimalist predecessor of phases, barriers (more precisely, blocking categories; barriers are predecessors of phases in the sense that both barriers and phases are crucially used in defining opaque/nonopaque domains for extraction). -

Nagoya Section Annual Report 2018
1 IEEE Nagoya Section Annual Report 2018 PART A - SECTION SUMMARY A.1 Executive Summary – (Please follow the format given below) Section Executive Committee Member List (2019/2020) (a) Officers: Chair: Dr. Naohiro Hozumi (Professor, Toyohashi University of Technology) e-mail: [email protected] Vice Chair: Dr. Kenji Nakazawa (Professor, Kanazawa Institute of Technology) e-mail: [email protected] Secretary: Dr. Jun Sato (Professor, Nagoya Institute of Technology) e-mail: [email protected] Treasurer: Dr. Naoki Hayakawa (Professor, Nagoya University) e-mail: [email protected] Auditor: Mr. Takahiro Kozawa (TOYOTA Central R&D Labs., Inc.) e-mail: [email protected] (b) Standing Committee Chairs: Nomination Committee: Dr. Yuji Muramoto (Professor, Meijo University) e-mail: [email protected] Membership Development Committee: Dr. Yuki Funabora (Assistant Professor, Nagoya University) e-mail: [email protected] Technical Activities Committee: Dr. Kunihiko Sasaki (DENSO Corporation) e-mail: [email protected] Student Activities Committee: Dr. Katsuhiro Naito (Associate Professor, Aichi Institute of Technology) e-mail: [email protected] Award Committee: Dr. Eiji Okamoto (Associate Professor, Nagoya Institute of Technology) e-mail: [email protected] Chapter Operation Committee: Dr. Hideyuki Hasegawa (Professor, Toyama University) e-mail: [email protected] 2 (c) Past Chairs: 2017-2018 Chair: Dr. Yutaka Ishibashi (Professor, Nagoya Institute of Technology) e-mail: [email protected] 2015-2016 Chair: Dr. Takeshi Furuhashi (Professor, Nagoya University) e-mail: [email protected] 2009-2010 Chair, Milestone: Dr. Masayuki Nagao (Professor, Toyohashi University of Technology) e-mail: [email protected] Election Process of Section Officers and Auditors (1) The Nominations Committee consisting of two (2) or more members, not then Section Officers, shall be appointed by the Section Chair with the approval of the Section Executive Committee. -
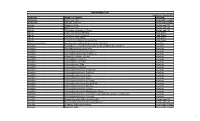
Unai Members List August 2021
UNAI MEMBER LIST Updated 27 August 2021 COUNTRY NAME OF SCHOOL REGION Afghanistan Kateb University Asia and the Pacific Afghanistan Spinghar University Asia and the Pacific Albania Academy of Arts Europe and CIS Albania Epoka University Europe and CIS Albania Polytechnic University of Tirana Europe and CIS Algeria Centre Universitaire d'El Tarf Arab States Algeria Université 8 Mai 1945 Guelma Arab States Algeria Université Ferhat Abbas Arab States Algeria University of Mohamed Boudiaf M’Sila Arab States Antigua and Barbuda American University of Antigua College of Medicine Americas Argentina Facultad de Ciencias Económicas de la Universidad de Buenos Aires Americas Argentina Facultad Regional Buenos Aires Americas Argentina Universidad Abierta Interamericana Americas Argentina Universidad Argentina de la Empresa Americas Argentina Universidad Católica de Salta Americas Argentina Universidad de Congreso Americas Argentina Universidad de La Punta Americas Argentina Universidad del CEMA Americas Argentina Universidad del Salvador Americas Argentina Universidad Nacional de Avellaneda Americas Argentina Universidad Nacional de Cordoba Americas Argentina Universidad Nacional de Cuyo Americas Argentina Universidad Nacional de Jujuy Americas Argentina Universidad Nacional de la Pampa Americas Argentina Universidad Nacional de Mar del Plata Americas Argentina Universidad Nacional de Quilmes Americas Argentina Universidad Nacional de Rosario Americas Argentina Universidad Nacional de Santiago del Estero Americas Argentina Universidad Nacional de -
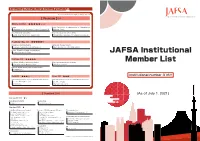
JAFSA Institutional Member List
Supporting Member(Social Business Partners) 43 ※ Classified by the company's major service [ Premium ](14) Diamond( 4) ★★★★★☆☆ Finance Medical Certificate for Visa Immunization for Studying Abroad Western Union Business Solutions Japan K.K. Hibiya Clinic Global Student Accommodation University management and consulting GSA Star Asia K.K. (Uninest) Waseda University Academic Solutions Corporation Platinum‐Exe( 3) ★★★★★☆ Marketing to American students International Students Support Takuyo Corporation (Lighthouse) Mori Kosan Co., Ltd. (WA.SA.Bi.) Vaccine, Document and Exam for study abroad Tokyo Business Clinic JAFSA Institutional Platinum( 3) ★★★★★ Vaccination & Medical Certificate for Student University management and consulting Member List Shinagawa East Medical Clinic KEI Advanced, Inc. PROGOS - English Speaking Test for Global Leaders PROGOS Inc. Gold( 2) ★★★☆ Silver( 2) ★★★ Institutional number 316!! Global Human Resources services・Study Abroad Information Global Human Resources services・Study Abroad Information Access Nextage Co.,Ltd Doorkel Co.,Ltd. DISCO Inc. Mynavi Corporation [ Standard ](29) (As of July 1, 2021) Standard20( 2) ★☆ Study Abroad Information Housing・Hotel Keibunsha MiniMini Corporation . Standard( 27) ★ Study Abroad Program and Support Insurance / Risk Management /Finance Telecommunication Arc Three International Co. Ltd. Daikou Insurance Agency Kanematsu Communications LTD. Australia Ryugaku Centre E-CALLS Inc. Berkeley House Language Center JAPAN IR&C Corporation Global Human Resources Development Fuyo Educations Co., Ltd. JI Accident & Fire Insurance Co., Ltd. JTB Corp. TIP JAPAN Fourth Valley Concierge Corporation KEIO TRAVEL AGENCY Co.,Ltd. Tokio Marine & Nichido Fire Insurance Co., Ltd. Originator Co.,Ltd. OKC Co., Ltd. Tokio Marine & Nichido Medical Service Co.,Ltd. WORKS Japan, Inc. Ryugaku Journal Inc. Sanki Travel Service Co.,Ltd. Housing・Hotel UK London Study Abroad Support Office / TSA Ltd. -

CURRICULUM VITAE Keiko Murasugi Department of British and American Studies, Graduate School of Humanities, Center for Linguistic
CURRICULUM VITAE Keiko Murasugi Department of British and American Studies, Graduate School of Humanities, Center for Linguistics, Nanzan University Address: 18Yamazato-cho, Showa-ku, Nagoya 466-8673 Japan Phone: (52) 832-3111 Fax: (52) 832-5330 mail: [email protected] EDUCATION 1983.3.1. B.A. in English and English Literature, Tsuda College 1985.3. M.A. in English Linguistics, Tsuda College 1989.1. M.A. in Linguistics, University of Connecticut 1991.3. Ph.D. in Linguistics, University of Connecticut EXPERIENCE (A) Full-Time Positions 1991.4.-1998.3. Associate Professor, Department of English and English Literature, Kinjo Gakuin University 1998.4.-2004.4. Associate Professor, Department of British and American Studies, Nanzan University 2004.4-present. Professor, Department of British and American Studies, Nanzan University (B) Short-term Visiting Appointments 1985.4.-1986.6. Lecturer, Tsuda English School 1988.9.-1990.8. Lecturer, Department of Modern Language, University of Connecticut. 1992.4.-1993.3. Faculty of Arts and Letters and the Graduate School, Tohoku University, Sendai, Miyagi. 1994.9.-1995.3. Nagoya City Junior College, School of Pre-school Education, Owari Asahi, Aichi. 1995.4.-1998.3. Faculty of Foreign Studies and Faculty of Humanities, Nanzan University, Nagoya, Aichi. 2002.4-2003.3. The University of the Air, Nagoya, Aichi. 2003.4-2004.3. Nagoya University, Nagoya, Aichi. 2004.4- 2011.3. Kinjo Gakuin University, Nagoya, Aichi. 2009.4-2010.3. Mie University, Tsu, Mie. 2010.4-2011.3. Kobe University, Hyogo, Hyogo. 2012.4- present. Nagoya City University, Nagoya, Aichi COURSES TAUGHT (A) Graduate: Introduction to English Linguistics, Syntax, Psycholinguistics, Seminar in Psycholinguistics, The Structure of English and Japanese. -

The 4Th International Symposium of Training Plan for Oncology Professionals
The 4 th International Symposium of Training Plan for Oncology Professionals February 27 (Sat), 28 (Sun), 2016 Sheraton Miyako Hotel Osaka"Main Hall Yamato-no-Ma" 6-1-55, Uehommachi, Tennoji-ku, Osaka 543-0001, JAPAN http://www.miyakohotels.ne.jp/osaka/english/ Hosted by 7-University Joint Project of Training Plan for Oncology Professionals Supporters Listed in no particular order 特定非営利活動法人 近畿がん診療推進ネットワーク Chugai Pharmaceutical Co., Ltd. Training Plan for Oncology Professionals gratefully acknowledges the generous support of organizations whose funding has made the 4th International Symposium possible. DAY 1 CONTENTS February 27 (Sat), 2016 4F Yamato no ma Opening Ceremony ▶ 11:00 – 11:10 Moderator Toshio Shimizu, M.D., Ph.D., Tsutomu Iwasa, M.D., Ph.D., Takeshi Yoshida, M.D., Ph.D., Junko Tanizaki, M.D., Ph.D. (Department of Medical Oncology, Kinki University Faculty of Medicine) Opening Remark Masayuki Iki, M.D., Ph.D. (Dean, Kinki University Faculty of Medicine) Introduction Kazuhiko Nakagawa, M.D., Ph.D. (Professor, Department of Medical Oncology, Kinki University Faculty of Medicine) Chugai Pharmaceutical Co., Ltd. Keynote Lecture ▶ 11:10 – 12:10 ......................................................................6 Chair: Tomoya Kawaguchi, M.D., Ph.D. (Associate Professor, Department of Respiratory Medicine, Graduate School of Medicine, Osaka City University) Kazuto Nishio, M.D., Ph.D. (Professor, Department of Genome Biology, Kinki University Faculty of Medicine) Molecular correlative studies in randomized clinical studies of angiogenesis inhibitors. Session 1 Radiation Oncology ▶ 12:40 – 14:00............................................................................................................................................8 Chair persons: Scott Bratman, M.D., Ph.D. (Princess Margaret Cancer Centre, Department of Radiation Oncology, University of Toronto, Canada) Ryohei Sasaki, M.D., Ph.D. -

Mie University Mie University Thailand Center for Education & Research at Thammasat University Contact Address: 1577 Kurimamachiya-Cho, Tsu City, Mie Pref
Mie University Mie University Thailand Center For Education & Research At Thammasat University Contact address: 1577 Kurimamachiya-cho, Tsu city, Mie pref. JAPAN http://www.cie.mie-u.ac.jp/en/cier/ We provide world-class community-based education and From Mie to the World! research results through harmonious coexistence of nature and mankind. Our Philosophy As a center of learning, Mie University strives to Our partnership has expended to 110 universities/ institutions in 36 contribute towards the “Development of Human countries/areas, conducting mutual exchange activities and Resources and Research,” enhancing the “Welfare of the international collaborative research. Society,” through the “Harmonious Coexistence of University International Nature and Mankind.” Students House The Center for International Education and Research Center for Foreign Students’ Dorm International Education & Research It was inaugurated on October 1st, 2005, as a special facility for Single 30 Rooms research and education. It aims through international education and Couple 5 Rooms research to nurture human resources contributing towards and to Women’ Dorm for promote globalization on campus and in the community. In addition, International Students Single 52 Rooms CIER plays an key role in carrying out international activities. Quad 8 Rooms Shared 14 Rooms 240 Capacity for International Students Single/Female International Activities 25 rooms Tri‐U International Joint Seminar & Symposium Alumni in Thailand This Seminar & Symposium is an academic meeting Thai Students’ Association in Japan under the Royal Patronage has a long hosted by Mie University (Japan), Chiang Mai University history of 76 years holding about 1,000 Thai students all over Japan. A (Thailand), Jiangsu University (China), and Bogor graduate student of Mie University, was taking a role of representative for the Agricultural University (Indonesia) in turn. -

Nation Knowledge Of
Members of the JANU Access ●Regular Members(86 national universities) ●Special Members(4 organizations) National Institutes for the Humanities, National Center of Sciences Bldg. 4F National Institutes of Natural Sciences, Hokkaido Branch (Gakujutsu Sogo Center) High Energy Accelerator Research Organization, Research Organization of Information and Systems (7 universities) To Suidobashi To Ochanomizu Hokkaido University, Hokkaido University of Education, Muroran Institute of Technology, To Kudanshita Yasukuni-dori Ave. Nation of Otaru University of Commerce, Obihiro University of Agriculture and Jimbocho Knowledge Veterinary Medicine, To Sudacho Asahikawa Medical University, Station Kitami Institute of Technology Shogakukan Tokyo Branch ● Tohoku Branch Metropolitan Expressway No.5 (12 universities) 5 Kyoritsu Hall To Kanda ●Gakushi Kaikan The University of Tokyo, ( 7 universities) ● Station Tokyo Medical and Dental University, Hirosaki University, Tokyo University of Foreign Studies, Iwate University, Hakusan-dori Ave. 2019 Tokyo Gakugei University, Tohoku University, Tokyo University of Agriculture and Technology, Miyagi University of Education, ● Tokyo University of the Arts, Akita University, Josui Kaikan To Kandabashi Tokyo Institute of Technology, Yamagata University, Tokyo University of Marine Science and Technology, Fukushima University C1 Metropolitan Expressway Loop Line Ochanomizu University, ●Palace Side Building The University of Electro-Communications, To Daikancho Hitotsubashi University, Entrance/Exit To Kandabashi National -

BY SHIGEKO OOISHI Faculty of Fisheries, Mie University, Tsu, Mie 514, Japan
NOTES AND NEWS SUEO M. SHIINO (1908-1978) BY SHIGEKO OOISHI Faculty of Fisheries, Mie University, Tsu, Mie 514, Japan Professor Sueo M. Shiino, Advisory editor of "Crustaceana", passed away on September 20, 1978, at Mie University Hospital. A distinguished carcinologist, a highly responsible researcher, and a much loved friend of his colleagues and students, Dr. Shiino has left them a much greater legacy than can be found in his - 137 publications the legacy of a devoted scientist, teacher and friend. He died before the publication of his last great work, a taxonomic paper on the sub- antarctic tanaid crustaceans collected by French scientists on board the survey ship "Marion-Dufresne". At the time of his death, he was director of Shima Marineland in Mie Prefecture. Born on the 1st of January, 1908 in Nagoya, Aichi Prefecture, Professor Shiino began his studies as a zoologist in 1927 in the Zoology Section, Faculty of Science, Kyoto University and graduated from the University in 1930, with a Master of Science degree. While studying at the University, he was trained by Professor Taku Komai and Professor Yo K. Okada who were pioneers in the field of zoology in Japan. After graduating from the University he stayed in the same Section as a researcher for one year. In 1931 Shiino was appointed assistant scientist at the Seto Marine Biological Laboratory, Kyoto University. He stayed at Shirahama, Wakayama Prefecture, where the Laboratory was located, for eleven years, and was appointed lecturer there in 1941. In 1934, while he was at Shirahama, he married Yukiko Ito of Nagoya. -

International Symposium on Affective Science and Engineering
Submission No.:C000005 Exploratory Survey on the Subjective Meaningfulness of Di... Affective Education Keywords: subjective meaningfulness, digitization, electr... ISASE 2019 Exploratory Survey on the Subjective Meaningfulness of Digitization among Nurses at two Hospitals in Japan Makoto Suzaki*, Shizu Hirohata*, Takashi Koseko**, Sachie Takeuchi***, Chiharu Miyata***, Mayumi Mizutani***, Mayumi Okita***, Yoshiko Takeda***, ****, Hiroki Funao***, ****, Takemasa Ishikawa***, Keiko Fukuroku***, Elke Düsch*****, and Yugo Narita***, ****** * Kinan Hospital, 4750 Atawa, Mihama town, Minami-Muro county, Mie 519-5293, Japan [email protected], [email protected] ** Department of Nursing, Mie University Hospital, 2-174, Edobashi, Tsu city, Mie 514-8507, Japan [email protected], [email protected] *** Course of Nursing Science, Graduate School of Medicine, Mie University, 2-174 Edobashi, Tsu city, Mie 514-8507, Japan [email protected], [email protected], [email protected] [email protected], [email protected], [email protected] [email protected], [email protected] **** Center for Medical and Nursing Education, Faculty of Medicine, Mie University, 2-174 Edobashi, Tsu city, Mie 514-8507, Japan *****Department of Economy in Social- and Healthcare, Catholic University of Applied Science Freiburg, 63 Karlstraße, 79104, Freiburg, Germany. [email protected] ******Department of Neurology, Mie University Hospital, 2-174, Edobashi, Tsu city, Mie 514-8507, Japan [email protected] Abstract: This survey aimed to evaluate the subjective meaningfulness of digitization using electronic medical records among Japanese nurses at two hospitals. -

1. Japanese National, Public Or Private Universities
1. Japanese National, Public or Private Universities National Universities Hokkaido University Hokkaido University of Education Muroran Institute of Technology Otaru University of Commerce Obihiro University of Agriculture and Veterinary Medicine Kitami Institute of Technology Hirosaki University Iwate University Tohoku University Miyagi University of Education Akita University Yamagata University Fukushima University Ibaraki University Utsunomiya University Gunma University Saitama University Chiba University The University of Tokyo Tokyo Medical and Dental University Tokyo University of Foreign Studies Tokyo Geijutsu Daigaku (Tokyo University of the Arts) Tokyo Institute of Technology Tokyo University of Marine Science and Technology Ochanomizu University Tokyo Gakugei University Tokyo University of Agriculture and Technology The University of Electro-Communications Hitotsubashi University Yokohama National University Niigata University University of Toyama Kanazawa University University of Fukui University of Yamanashi Shinshu University Gifu University Shizuoka University Nagoya University Nagoya Institute of Technology Aichi University of Education Mie University Shiga University Kyoto University Kyoto University of Education Kyoto Institute of Technology Osaka University Osaka Kyoiku University Kobe University Nara University of Education Nara Women's University Wakayama University Tottori University Shimane University Okayama University Hiroshima University Yamaguchi University The University of Tokushima Kagawa University Ehime -

25. Mie University (PDF/132KB)
Mie University Graduate School of Bioresources Graduate School code:25 Web site: http://www.bio.mie-u.ac.jp/en/index.html 1. Graduate School code 25 2. Maximum number of 3 (three) Participants per year participants ■Environmental Science ■Marine Science ■Meteorology ■Natural Disaster/ Disaster Prevention Science □Tourism □Politics 3. Fields of Study ■Economics ■Sociology □Education ■Engineering ■ Agriculture (incl. Fisheries) □Geology ■ ICT □Medical Science □Others( ) Plant Molecular Genetics and Breeding, Crop Science, Horticultural Crop Physiology, Animal Production, Grassland and Animal Feed Production, Plant Medicine, Insect Ecology, Vegetable Genomics and Breeding, Forest Conservation Ecology, Forest Mycology, Soil Science and Plant Nutrition, Torrent and Hillside Conservation Technology, Forest Engineering, Wood science and technology, Lignocellulose control science and technology, Sustainable Resource Economics, Farm Management and Rural Sociology, Economic System of Bioresources, Global Plant Resource Science, Global Resource utilization Science, Atmosphere and Climate Dynamics, Ocean Climate Laboratory, Sustainable Earth System Laboratory, Vadose Zone Hydrology, Agricultural and Food Systems, Water Environment and Natural Disasters, Forest Planning for the Environment, Applied Environmental Studies, Nature and Coexistence, Environmental Information and Technology, Productive Environment System, Environmental Control Sub Fields in Biology, Energy Utilization Engineering, Applied Geomorphology, Soil Resources Engineering, Water