761172Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

T. Franklin Williams Scholars Program
Developing a New Generation of Medical Subspecialists with Expertise in Aging and Care of the Elderly T. Franklin Williams Scholars Program Report to T. Franklin Williams Scholars Program Evaluation Team ASP Geriatrics Steering Committee Integrating Geriatrics Project Evaluation Team May 2011 Submitted by: Erika D. Tarver Project Administrator Association of Specialty Professors 330 John Carlyle Road Suite 610 Alexandria, VA 22314 T: (703) 341-4540 F: (703) 519-1890 [email protected] Kevin P. High, MD Principal Investigator William R. Hazzard, MD Co-Principal Investigator Table of Contents Narrative Progress Report Application and Award Progress Summary of Success of T. Williams Scholars Program Appendices A. 2008 Scholars 24-Month Progress Reports Neena S. Abraham, MD (Note: This is Dr. Abraham’s final report) Steven G. Coca, DO Jeffrey G. Horowitz, MD Danelle F. James, MD Heidi Klepin, MD George C. Wang, MD 2009 Williams Scholars Progress Reports and Summary of 18-Month Questionnaire B. Peter Abadir, MD 12-month Progress Report C. Kathleen M. Akgun, MD 12-Month Progress Report Publication D. Alison Huang, MD 12-Month Progress Report Publication E. Eswar Krishnan, MD 12-Month Progress Report Publication F. Rohit Loomba, MD Publication G. Sharmilee Nyenhuis, MD 12-Month Progress Report Publication H. Peter P. Reese, MD 12-Month Progress Report Publication I. Erik B. Schelbert, MD 12-Month Progress Report Publication J. Helen Keipp Talbot, MD 12-Month Progress Report Publication K. Summary of 18-Month Questionnaire 2010 Williams Scholars Mentor Interviews and Summary of Six-Month Questionnaire L. Kellie Hunter-Campbell, MD Six-Month Mentor Interview M. -

Journal Pre-Proof
Journal Pre-proof Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. Jaworski PII: S2319-4170(20)30209-2 DOI: https://doi.org/10.1016/j.bj.2020.11.011 Reference: BJ 374 To appear in: Biomedical Journal Received Date: 2 September 2020 Revised Date: 6 November 2020 Accepted Date: 22 November 2020 Please cite this article as: Jaworski JP, Neutralizing monoclonal antibodies for COVID-19 treatment and prevention, Biomedical Journal, https://doi.org/10.1016/j.bj.2020.11.011. This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2020 Chang Gung University. Publishing services by Elsevier B.V. TITLE: Neutralizing monoclonal antibodies for COVID-19 treatment and prevention Juan P. JAWORSKI Consejo Nacional de Investigaciones Científicas y Técnicas, Buenos Aires, Argentina Instituto Nacional de Tecnología Agropecuaria, Buenos Aires, Argentina KEYWORDS: SARS-CoV-2, Coronavirus, Monoclonal Antibody, mAb, Prophylaxis, Treatment CORRESPONDING AUTHOR: Dr. Juan Pablo Jaworski, DVM, MSc, PhD. Consejo Nacional de Investigaciones Científicas y Técnicas Instituto de Virología, Instituto Nacional de Tecnología Agropecuaria Las Cabañas y de los Reseros (S/N), Hurlingham (1686), Buenos Aires, Argentina Tel / Fax: 054-11-4621-1447 (int:3400) [email protected] ABSTRACT The SARS-CoV-2 pandemic has caused unprecedented global health and economic crises. -

Fnl Operations and Additional Updates
Frederick National Laboratory Operations and Additional Updates Ethan Dmitrovsky, M.D. President, Leidos Biomedical Research and Laboratory Laboratory Director, Frederick National Laboratory for Cancer Research DEPARTMENT OF HEALTH AND HUMAN SERVICES • National Institutes of Health • National Cancer Institute Frederick National Laboratory is a Federally Funded Research and Development Center operated by Leidos Biomedical Research, Inc., for the National Cancer Institute Session Objectives • Review the Frederick National Laboratory rapid response to the pandemic. This is a case study for a Federally Funded Research and Development Center. • Show that this pivot did not prevent decisive quantitative or discovery science, translational research, and clinical trials. • Cite NCI and NIAID programs with major recent progress. • Answer your questions. Federally Funded Research and Development Center Operations Federally Funded Research and Development Center Contract Task Order Portfolio: • 5 Operational Task Orders - Benefits of services are recurring with annual funded appropriations. • NCI Task Order, 3 NIAID Task Orders, 1 Lease Task Order • 98 are Non-operational Task Orders • 38 are in Clinical Group • 47 are in Scientific Group • 13 are Facility or Infrastructure Refurbishments Task Orders • Extensive outreach to the broader research community is through subcontracting. Frederick National Laboratory Pivot with National Cancer Institute to Combat COVID-19 COVID-19 Publications ●Liu, G., et al. Cell Sys., In press, 2020. Pivot to ●Beigel, J.H. et al. New Engl. J. COVID-19 Med., 2020 ●Hicks, J., et al. medRxiv Response doi: https://doi.org/10.1101/2020.06 .22.20137695 Identifying genetic Testing and Clinical Trials to ●Klumpp-Thomas C., et al. determinants of validating Combat COVID-19 ► Identifying medRxivdoi: https://doi.org/10.110 SARS CoV 2 serologic assays Small molecule 1/2020.05.21.20109280. -

A Short Overview of Ebola Virus Disease
Short Communication Journal of Volume 6:4, 2021 DOI: 10.37421/jidm.2021.6.173 Infectious Diseases and Medicine A Short Overview of Ebola Virus Disease Akshay Thiwari* Department of Virology, University of Hyderabad, Hyderabad, Telangana, India Ebola [1] is an uncommon but lethal virus that causes fever, body Treatment for Ebola aches, diarrhea, and, in some cases, internal and external bleeding. The Ebola has no known cure, though researchers are working on one. For immune system and organs are harmed as the virus spreads through the the treatment of Ebola [2], two drug therapies have been authorized. Inmazeb body. As a result, the number of blood-clotting cells decreases. As a is a compound that consists of three monoclonal antibodies (atoltivimab, consequence, there is a lot of uncontrollable bleeding. Ebola hemorrhagic maftivimab, and odesivimab-ebgn). Ebanga (ansuvimab-zykl) is a monoclonal fever was the previous name for the outbreak, but it is now known as Ebola antibody that is given as an injection. It aids in stopping the virus from reaching virus. It kills up to 90% of those who become infected. the cell receptor. Doctors treat Ebola symptoms [3] with the following How does one contract Ebola? medication. Ebola isn't as infectious as viruses like the common cold, influenza, or Electrolytes and fluids, Oxygen (O2), Medication for high blood pressure, measles. Contact with the skin or bodily fluids of an infected animal, such as Transfusions of blood, and other diseases'. a monkey, chimp, or fruit bat, transmits the disease to humans. Then it Facts on Ebola passes from one person to the next in the same manner. -
February 2021 EPS Pipeline Report
Pipeline Report February 2021 Pipeline Report February 2021 © 2021 Envolve. All rights reserved. Page 1 This quarterly at-a-glance publication is developed by our Clinical Pharmacy Drug Information team to increase your understanding of the drug pipeline, Table of Contents ensuring you’re equipped with insights to prepare for shifts in pharmacy benefit management. In this issue, you’ll learn more about key themes and notable drugs referenced in the following points. COVID-19 1 > Veklury is currently the only agent that is FDA-approved for the treatment of COVID-19. Three additional therapeutics and two vaccines have been granted Emergency Use Authorization (EUA), and at least three more vaccines are Recent Specialty Drug Approvals1 4 expected to receive an EUA in the relatively near future. > The previous quarter noted the approval of several breakthrough therapies for rare or ultra-rare conditions, which previously had no available FDA-approved Recent Non-Specialty Drug Approvals 9 treatments — Zokinvy for Hutchinson-Gilford progeria syndrome and progeroid laminopathies, Oxlumo for primary hyperoxaluria type 1, and Imcivree for genetically mediated obesity. Upcoming Specialty Products 10 > Other notable approvals include: Lupkynis — the first oral therapy approved for lupus nephritis; Orladeyo — the first oral therapy approved as prophylaxis of hereditary angioedema attacks;Cabenuva – the first long-acting injectable antiretroviral therapy intended as maintenance treatment of HIV; and Breyanzi — Upcoming Non-Specialty Products 18 the -

HIV?AIDS Researchers at the NIH Clinical Center
The NIH Clinical Center treats a diverse group of patients from all over the world. It also draws researchers from different cultures and backgrounds. Learn more about some of the many researchers who conduct their work on the human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) at the Clinical Center. Thomas C. Quinn, M.D., M.Sc., conducts research for the National Institute of Allergy and Infectious Diseases at the NIH Clinical Center. He is a senior investigator and chief of the International HIV/STD Section of the Laboratory of Immunoregulation. Dr. Quinn obtained his M.D. from Northwestern University. He was a research associate in infectious diseases in the NIAID Laboratory of Parasitic Diseases and completed a fellowship in infectious diseases at the University of Washington. Since 1981, he has been assigned to the division of infectious diseases at Johns Hopkins University, where he became a professor of medicine in 1991. Dr. Quinn is a member of the Institute of Medicine and the National Academy of Sciences and is a fellow of the American Association for the Advancement of Science. His major areas of research are: Definition of epidemiologic features of HIV-1 and HIV-2 infections in developing countries and the United States Assessment of biomedical interventions to control HIV, including circumcision, prevention of mother-to-child transmission, pre-exposure prophylaxis, and vaccine development Assessment of the frequency of Chlamydia trachomatis infections in selected populations using noninvasive sensitive nucleic-acid amplification assays for diagnosis Evaluations of interventions to control blinding trachoma due to Chlamydia trachomatis in sub-Saharan Africa See the full program description. -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -

That Record-Breaking Sprint to Create a COVID-19 Vaccine The
NATIONAL INSTITUTES OF HEALTH • OFFICE OF THE DIRECTOR | VOLUME 29 ISSUE 5 • SEPTEMBER-OCTOBER 2021 That Record-breaking The Intersection of Man and Machine Sprint to Create a Bionics Gives New Hope to Those Living With Physical Disabilities COVID-19 Vaccine BY MICHAEL TABASKO, OD BY MELISSA GLIM At the end of 2019, most people were looking forward to an exciting 2020, a new decade starting with those magic numbers, 20-20, that denote a sharpness of vision. There would be the Summer Olympics in Japan and the U.S. presidential election. Meanwhile, intramural scientists at the National Institute of Allergy and Infectious Diseases’ Vaccine Research Center (VRC) were designing vaccines for several coronaviruses using a promising, new platform based on messenger RNA (mRNA). Everything changed on a Saturday morning in early January. Chinese scientists CREDIT: TH0MAS BULEA (LEFT); NIH CLINCAL CENTER (RICHT) had isolated a new coronavirus that was (Left) The NIH pediatric exoskeleton for children with cerebral palsy and other movement disorders uses custom actuators causing a serious epidemic in China’s Wuhan from Agilik developed as part of a cooperative research and development agreement with NIH, along with embedded sensors and microcontrollers, to provide overground gait training while worn. (Right) Alexander Theodorakos, a participant province and released its genetic sequence to in a research protocol at the NIH Clinical Center that is evaluating the new pediatric exoskeleton, and Thomas Bulea, the the scientific community around the world. study’s principal investigator, discuss how the device changes the way the legs move when walking. Barney Graham, director of the VRC’s Viral Pathogenesis Laboratory (VPL), and If popular culture is any indication, the notion that bionic technology will VRC research fellow Kizzmekia Corbett someday redefine the boundaries of human function has long held our collective dropped everything and began using this fascination. -

Nci-Plan-2013.Pdf
THE NATIONAL CANCER PROGRAM MANAGING THE NATION’S RESEARCH PORTFOLIO AN ANNUAL PLAN AND BUDGET PROPOSAL FOR FISCAL YEAR 2013 National Cancer Institute U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES National Institutes of Health Contents 1 Foreword 4 Provocative Questions 8 Center for Cancer Genomics 16 Introduction to Cancer Profiles 18 Pancreatic Ductal Adenocarcinoma 22 Colorectal Cancer 26 B-Cell Lymphoma 30 Renal Cell (Kidney) Cancer 34 GI Stromal Cancer 39 Research Focus: Comorbidities 42 Research Focus: Circulating Tumor Cells 44 Research Focus: Reducing Cancer Health Disparities 50 The Frederick National Laboratory for Cancer Research 61 Small Business Innovation Research, Small BusinessTechnology Transfer (SBIR, STTR) 66 NCI Center for Global Health 72 NCI-Designated Cancer Centers 83 Glossary of Terms 84 Budget FOREWORD The National Cancer Program MANAGING THE NATION’S RESEARCH PORTFOLIO his year marks the 75th anniversary of the founding of the National Cancer Institute, the first so-called “categorical institute” of what has become the National Institutes of Health, with its 27 Institutes and Centers. Over the years, the Congress and the public have generously supported the TNCI—and the NIH generally—with sustained budgetary increases. This was especially true for the NCI during the rapid expansion of its budget following the National Cancer Act of 1971 and for the NIH, including the NCI, during the 5-year doubling of its budget, launched in 1998. Both of these eras of rapid growth were remarkably fruitful. The first launched the pursuit of cancer genes and the molecular basis of oncogenesis, laying the foundation for the transformation of clinical oncology that is now occurring. -

NIHAA Update 1Velco111es Lerters and Eastern Europe and at the Undergradu 1968, a Period of Considerable Growth News from Its Readers
The Newsletter of the L NIH Alumni Association Summer 1999 Vol. 11, No. 2 date NIHAA Members Enjoy June Annual Meeting with Henney, Morella Alumni attendi ng the 1999 annual meeting of the NIH.AA were given a first-band briefing on FDA by Dr. Jane E. Henney, the receml y appointed FDA commissioner. Tbe audience also participated in a question and answer exchange witb Rep. Constance A. Morella (R-Md.), who was presented with tbe NIHAA 1999 Public Service Award. Almost I00 alumni attended the June 12 morning meeting at the Mary Woodard Lasker Center on the NIH campus. Henney, wbo was NCI deputy director for five of her lO years at NIH (1985-1995) spoke infonnalJy on some of FDA's principal concerns at this time: the agency's efforts to speed Shown at the NIHAA annual meeting are (from I} NIH alumna Dr. Jane E. Henney, FDA up review without sacrifice of quality commissioner, who spoke on "Back Home Again via Indiana, Kansas and New Mexico," and safeguards; tbe need for recruiting Dr. John F. Sherman, Rep. Constance A. Morella (R-Md.), who received the 1999 NIHAA Public Service Award, and Dr. William S. Jordan, Jr., outgoing NIHAA president. (see A flflual Meeting, p. 12) Director's Advisors Bat 6 for 7 in June Meeting In This Issue Page Choppin To Give Third Research Festival '99 J By Rich McManus NIHAA Shannon Lecture Ca/e11dar 5 The scorecard at the end of a daylong Dr. Purnell W. Cboppin, president of .News .from a11d about Nlf/A;/ me111be1:r (f session of lhe advisory committee to the Howard Hughes Medical lnstirure, the NIH director (ACD) on June 3 read A le11erjro1111he 11e111 Nlf/AIJ preside111 IO will deliver the third James A. -

Study Protocol, Including Amendment
Document Type: Study Protocol, including Amendment (Informed Consent Template located in Appendix I of the Protocol Version 1.0 and Version 2.0) Official Title: A Phase I, Open-Label, Dose-Escalation Study of the Safety and Pharmacokinetics of a Human Monoclonal Antibody, VRC-EBOMAB092-00-AB (MAb114), Administered Intravenously to Healthy Adults NCT Number: NCT03478891 Document/Date: Protocol Amendment Version 2.0: April 6, 2018 Protocol Version 1.0: February 21, 2018 Version 2.0 April 6, 2018 VACCINE RESEARCH CENTER Protocol VRC 608 (NIH 18-I-0069) A PHASE I, OPEN-LABEL, DOSE-ESCALATION STUDY OF THE SAFETY AND PHARMACOKINETICS OF A HUMAN MONOCLONAL ANTIBODY, VRC-EBOMAB092-00-AB (MAB114), ADMINISTERED INTRAVENOUSLY TO HEALTHY ADULTS Study Product Provided by: Vaccine Research Center (VRC) National Institute of Allergy and Infectious Diseases (NIAID) National Institutes of Health (NIH) Bethesda, MD Clinical Trial Sponsored by: NIAID/VRC/NIH, Bethesda, Maryland IND 138,090 Sponsored by: VRC/NIAID/NIH, Bethesda, Maryland Principal Investigator: Martin Gaudinski, MD VRC/NIAID/NIH Bethesda, MD 20892 IRB Initial Review Date: January 8, 2018 PRODUCT: VRC-EBOMAB092-00-AB (MAb114) PROTOCOL: VRC 608, VERSION 2.0 PROTOCOL DATE: APRIL 6, 2018 TABLE OF CONTENTS Page ABBREVIATIONS....................................................................................................................... 5 PRÉCIS.......................................................................................................................................... 8 1. INTRODUCTION............................................................................................................ -
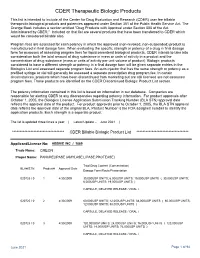
CDER Therapeutic Biologic Products List
CDER Therapeutic Biologic Products This list is intended to include all the Center for Drug Evaluation and Research (CDER) user fee billable therapeutic biological products and potencies approved under Section 351 of the Public Health Service Act. The Orange Book includes a section entitled "Drug Products with Approval under Section 505 of the Act Administered by CBER." Included on that list are several products that have been transferred to CDER which would be considered billable also. Program fees are assessed for each potency in which the approved (non-revoked, non-suspended) product is manufactured in final dosage form. When evaluating the specific strength or potency of a drug in final dosage form for purposes of assessing program fees for liquid parenteral biological products, CDER intends to take into consideration both the total amount of drug substance in mass or units of activity in a product and the concentration of drug substance (mass or units of activity per unit volume of product). Biologic products considered to have a different strength or potency in a final dosage form will be given separate entries in the Biologics List and assessed separate program fees. An auto-injector that has the same strength or potency as a prefilled syringe or vial will generally be assessed a separate prescription drug program fee. In certain circumstances, products which have been discontinued from marketing but are still licensed are not assessed program fees. Those products are identified on the CDER Discontinued Biologic Product List section. The potency information contained in this list is based on information in our database.