Cellulitis and Soft Tissue Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bacterial Skin Infections an Observational Study
RESEARCH Geoffrey Spurling Deborah Askew David King Geoffrey K Mitchell MBBS, DTM&H, FRACGP, is Senior PhD, is Senior Research Fellow, MBBS, MPH, FRACGP, is Senior Lecturer, MBBS, PhD, FRACGP, FAChPM, Lecturer, Discipline of General Practice, Discipline of General Practice, Discipline of General Practice, University is Associate Professor, Discipline University of Queensland. g.spurling@ University of Queensland. of Queensland. of General Practice, University of uq.edu.au Queensland. Bacterial skin infections An observational study Bacterial skin infections such as impetigo and boils are Background common, contagious, often painful, and have the potential to We aimed to determine the feasibility of measuring resolution rates of recur. They are caused by Staphylococcus aureus and bacterial skin infections in general practice. occasionally by Streptococcus pyogenes, and are transmitted Methods by skin-to-skin contact, fomite contact or contact with nasal Fifteen general practitioners recruited patients from March 2005 to carriers.1 In the United Kingdom, incidence of skin infections October 2007 and collected clinical and sociodemographic data at in children in 2005 was approximately 75 per 100 000.2 Skin baseline. Patients were followed up at 2 and 6 weeks to assess lesion infection rates are likely to be higher in warmer climates. The resolution. only Australian data we found were for one Northern Territory Results Aboriginal Medical Service (Danila Dilba), which recorded 7.5 Of 93 recruited participants, 60 (65%) were followed up at 2 and 6 per 100 consultations for localised skin infections.3 weeks: 50% (30) had boils, 37% (22) had impetigo, 83% (50) were prescribed antibiotics, and active follow up was suggested for 47% Suggested risk factors for impetigo include: household crowding, (28). -

Current Microbiological, Clinical and Therapeutic Aspects of Impetigo Lior Zusmanovich, Lior Charach and Gideon Charach*
ISSN: 2378-3656 Zusmanovich et al. Clin Med Rev Case Rep 2018, 5:205 DOI: 10.23937/2378-3656/1410205 Volume 5 | Issue 3 Clinical Medical Reviews Open Access and Case Reports CASE REPORT Current Microbiological, Clinical and Therapeutic Aspects of Impetigo Lior Zusmanovich, Lior Charach and Gideon Charach* Department of Internal Medicine “C”, Affiliated to Tel Aviv University, Israel *Corresponding author: Gideon Charach, Department of Internal Medicine “C”, Tel Aviv Sourasky Check for Medical Center, Sackler Medical School, Affiliated to Tel Aviv University, 6 Weizman Street, Tel Aviv updates 6423906, Israel, Tel: +972-3-6973766, Fax: +972-3-6973929, E-mail: [email protected] nonpurulent and purulent cellulitis, and treatment is Abstract based on extent of infection and risk factors. Abscesses Impetigo is a highly contagious infection of the epidermis, involve the dermis and deeper skin tissues as a result of seen especially among children, and transmitted through direct contact. Two bacteria are associated with impetigo: pus formation. S. aureus and GAS. Over 140 million people are suffering Impetigo is observed most frequently among chil- from impetigo at each time point, over 100 million are chil- dren. Two forms of impetigo exist, namely impetigo conta- dren 2-5 years of age and is transmitted through direct giosa, known as the non-bullous form and the second one contact [1]. Risk factors for impetigo include poor hy- being bullous impetigo which presents with large and fragile giene, low economic status, crowding and underlying bullae. Treatment options for impetigo include systemic an- scabies [2,3]. Important consideration is carriage of tibiotics, topical antibiotics as well as topical disinfectants. -

Naeglaria and Brain Infections
Can bacteria shrink tumors? Cancer Therapy: The Microbial Approach n this age of advanced injected live Streptococcus medical science and into cancer patients but after I technology, we still the recipients unfortunately continue to hunt for died from subsequent innovative cancer therapies infections, Coley decided to that prove effective and safe. use heat killed bacteria. He Treatments that successfully made a mixture of two heat- eradicate tumors while at the killed bacterial species, By Alan Barajas same time cause as little Streptococcus pyogenes and damage as possible to normal Serratia marcescens. This Alani Barajas is a Research and tissue are the ultimate goal, concoction was termed Development Technician at Hardy but are also not easy to find. “Coley’s toxins.” Bacteria Diagnostics. She earned her bachelor's degree in Microbiology at were either injected into Cal Poly, San Luis Obispo. The use of microorganisms in tumors or into the cancer therapy is not a new bloodstream. During her studies at Cal Poly, much idea but it is currently a of her time was spent as part of the undergraduate research team for the buzzing topic in cancer Cal Poly Dairy Products Technology therapy research. Center studying spore-forming bacteria in dairy products. In the late 1800s, German Currently she is working on new physicians W. Busch and F. chromogenic media formulations for Fehleisen both individually Hardy Diagnostics, both in the observed that certain cancers prepared and powdered forms. began to regress when patients acquired accidental erysipelas (cellulitis) caused by Streptococcus pyogenes. William Coley was the first to use New York surgeon William bacterial injections to treat cancer www.HardyDiagnostics.com patients. -

Inflammatory Or Infectious Hair Disease? a Case of Scalp Eschar and Neck Lymph Adenopathy After a Tick Bite
Case Report ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2021.35.005688 Adherent Serous Crust of the Scalp: Inflammatory or Infectious Hair Disease? A Case of Scalp Eschar and Neck Lymph Adenopathy after a Tick Bite Starace M1, Vezzoni R*2, Alessandrini A1 and Piraccini BM1 1Dermatology - IRCCS, Policlinico Sant’Orsola, Department of Specialized, Experimental and Diagnostic Medicine, Alma Mater Studiorum, University of Bologna, Italy 2Dermatology Clinic, Maggiore Hospital, University of Trieste, Italy *Corresponding author: Roberta Vezzoni, Dermatology Clinic, Maggiore Hospital, University of Trieste, Italy ARTICLE INFO ABSTRACT Received: Published: April 17, 2021 The appearance of a crust initially suggests inflammatory scalp diseases, although infectious diseases such as impetigo or insect bites should also be considered among April 27, 2021 the differential diagnoses. We report a case of 40-year-old woman presentedB. Burgdorferi to our, Citation: Starace M, Vezzoni R, Hair Disease Outpatient Service with an adherent serous crust on the scalp and lymphadenopathy of the neck. Serological tests confirmed the aetiology of while rickettsia infection was excluded. Lyme borreliosis can mimic rickettsia infection Alessandrini A, Piraccini BM. Adherent and may present as scalp eschar and neck lymphadenopathy after a tick bite (SENLAT). Serous Crust of the Scalp: Inflammatory Appropriate tests should be included in the diagnostic workup of patients with necrotic or Infectious Hair Disease? A Case of Scalp scalpKeywords: eschar in order to promptly set -
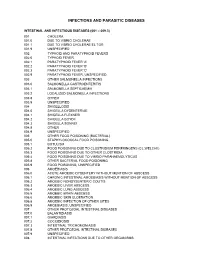
Diagnostic Code Descriptions (ICD9)
INFECTIONS AND PARASITIC DISEASES INTESTINAL AND INFECTIOUS DISEASES (001 – 009.3) 001 CHOLERA 001.0 DUE TO VIBRIO CHOLERAE 001.1 DUE TO VIBRIO CHOLERAE EL TOR 001.9 UNSPECIFIED 002 TYPHOID AND PARATYPHOID FEVERS 002.0 TYPHOID FEVER 002.1 PARATYPHOID FEVER 'A' 002.2 PARATYPHOID FEVER 'B' 002.3 PARATYPHOID FEVER 'C' 002.9 PARATYPHOID FEVER, UNSPECIFIED 003 OTHER SALMONELLA INFECTIONS 003.0 SALMONELLA GASTROENTERITIS 003.1 SALMONELLA SEPTICAEMIA 003.2 LOCALIZED SALMONELLA INFECTIONS 003.8 OTHER 003.9 UNSPECIFIED 004 SHIGELLOSIS 004.0 SHIGELLA DYSENTERIAE 004.1 SHIGELLA FLEXNERI 004.2 SHIGELLA BOYDII 004.3 SHIGELLA SONNEI 004.8 OTHER 004.9 UNSPECIFIED 005 OTHER FOOD POISONING (BACTERIAL) 005.0 STAPHYLOCOCCAL FOOD POISONING 005.1 BOTULISM 005.2 FOOD POISONING DUE TO CLOSTRIDIUM PERFRINGENS (CL.WELCHII) 005.3 FOOD POISONING DUE TO OTHER CLOSTRIDIA 005.4 FOOD POISONING DUE TO VIBRIO PARAHAEMOLYTICUS 005.8 OTHER BACTERIAL FOOD POISONING 005.9 FOOD POISONING, UNSPECIFIED 006 AMOEBIASIS 006.0 ACUTE AMOEBIC DYSENTERY WITHOUT MENTION OF ABSCESS 006.1 CHRONIC INTESTINAL AMOEBIASIS WITHOUT MENTION OF ABSCESS 006.2 AMOEBIC NONDYSENTERIC COLITIS 006.3 AMOEBIC LIVER ABSCESS 006.4 AMOEBIC LUNG ABSCESS 006.5 AMOEBIC BRAIN ABSCESS 006.6 AMOEBIC SKIN ULCERATION 006.8 AMOEBIC INFECTION OF OTHER SITES 006.9 AMOEBIASIS, UNSPECIFIED 007 OTHER PROTOZOAL INTESTINAL DISEASES 007.0 BALANTIDIASIS 007.1 GIARDIASIS 007.2 COCCIDIOSIS 007.3 INTESTINAL TRICHOMONIASIS 007.8 OTHER PROTOZOAL INTESTINAL DISEASES 007.9 UNSPECIFIED 008 INTESTINAL INFECTIONS DUE TO OTHER ORGANISMS -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Skin and Soft Tissue Infections Ohsuerin Bonura, MD, MCR Oregon Health & Science University Objectives
Difficult Skin and Soft tissue Infections OHSUErin Bonura, MD, MCR Oregon Health & Science University Objectives • Compare and contrast the epidemiology and clinical presentation of common skin and soft tissue diseases • State the management for skin and soft tissue infections OHSU• Differentiate true infection from infectious disease mimics of the skin Casey Casey is a 2 year old boy who presents with this rash. What is the best treatment? A. Soap and Water B. Ibuprofen, it will self OHSUresolve C. Dicloxacillin D. Mupirocin OHSUImpetigo Impetigo Epidemiology and Treatment OHSU Ellen Ellen is a 54 year old morbidly obese woman with DM, HTN and venous stasis who presented with a painful left leg and fever. She has had 3 episodes in the last 6 months. What do you recommend? A. Cefazolin followed by oral amoxicillin prophylaxis B. Vancomycin – this is likely OHSUMRSA C. Amoxicillin – this is likely erysipelas D. Clindamycin to cover staph and strep cellulitis Impetigo OHSUErysipelas Erysipelas Risk: lymphedema, stasis, obesity, paresis, DM, ETOH OHSURecurrence rate: 30% in 3 yrs Treatment: Penicillin Impetigo Erysipelas OHSUCellulitis Cellulitis • DEEPER than erysipelas • Microbiology: – 6-48hrs post op: think GAS… too early for staph (days in the making)! – Periorbital – Staph, Strep pneumoniae, GAS OHSU– Post Varicella - GAS – Skin popping – Staph + almost anything! Framework for Skin and Soft Tissue Infections (SSTIs) NONPurulent Purulent Necrotizing/Cellulitis/Erysipelas Furuncle/Carbuncle/Abscess Severe Moderate Mild Severe Moderate Mild I&D I&D I&D I&D IV Rx Oral Rx C&S C&S C&S C&S Vanc + Pip-tazo OHSUEmpiric IV Empiric MRSA Oral MRSA TMP/SMX Doxy What Are Your “Go-To” Oral Options For Non-Purulent SSTI? Amoxicillin Doxycycline OHSUCephalexin Doxycycline Trimethoprim-Sulfamethoxazole OHSU Miller LG, et al. -

Bacterial Infections Diseases Picture Cause Basic Lesion
page: 117 Chapter 6: alphabetical Bacterial infections diseases picture cause basic lesion search contents print last screen viewed back next Bacterial infections diseases Impetigo page: 118 6.1 Impetigo alphabetical Bullous impetigo Bullae with cloudy contents, often surrounded by an erythematous halo. These bullae rupture easily picture and are rapidly replaced by extensive crusty patches. Bullous impetigo is classically caused by Staphylococcus aureus. cause basic lesion Basic Lesions: Bullae; Crusts Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Impetigo page: 119 alphabetical Non-bullous impetigo Erythematous patches covered by a yellowish crust. Lesions are most frequently around the mouth. picture Lesions around the nose are very characteristic and require prolonged treatment. ß-Haemolytic streptococcus is cause most frequently found in this type of impetigo. basic lesion Basic Lesions: Erythematous Macule; Crusts Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Ecthyma page: 120 6.2 Ecthyma alphabetical Slow and gradually deepening ulceration surmounted by a thick crust. The usual site of ecthyma are the legs. After healing there is a permanent scar. The pathogen is picture often a streptococcus. Ecthyma is very common in tropical countries. cause basic lesion Basic Lesions: Crusts; Ulcers Causes: Infection search contents print last screen viewed back next Bacterial infections diseases Folliculitis page: 121 6.3 Folliculitis -

Abscesses Are a Serious Problem for People Who Shoot Drugs
Where to Get Your Abscess Seen Abscesses are a serious problem for people who shoot drugs. But what the hell are they and where can you go for care? What are abscesses? Abscesses are pockets of bacteria and pus underneath you skin and occasionally in your muscle. Your body creates a wall around the bacteria in order to keep the bacteria from infecting your whole body. Another name for an abscess is a “soft tissues infection”. What are bacteria? Bacteria are microscopic organisms. Bacteria are everywhere in our environment and a few kinds cause infections and disease. The main bacteria that cause abscesses are: staphylococcus (staff-lo-coc-us) aureus (or-e-us). How can you tell when you have an abscess? Because they are pockets of infection abscesses cause swollen lumps under the skin which are often red (or in darker skinned people darker than the surrounding skin) warm to the touch and painful (often VERY painful). What is the worst thing that can happen? The worst thing that can happen with abscesses is that they can burst under your skin and cause a general infection of your whole body or blood. An all over bacterial infection can kill you. Another super bad thing that can happen is a endocarditis, which is an infection of the lining of your heart, and “septic embolism”, which means that a lump of the contaminates in your abscess get loose in your body and lodge in your lungs or brain. Why do abscesses happen? Abscesses are caused when bad bacteria come in to contact with healthy flesh. -

Cellulitis (You Say, Sell-You-Ly-Tis)
Cellulitis (you say, sell-you-ly-tis) Any area of skin can become infected with cellulitis if the skin is broken, for example from a sore, insect bite, boil, rash, cut, burn or graze. Cellulitis can also infect the flesh under the skin if it is damaged or bruised or if there is poor circulation. Signs your child has cellulitis: The skin will look red, and feel warm and painful to touch. There may be pus or fluid leaking from the skin. The skin may start swelling. The red area keeps growing. Gently mark the edge of the infected red area How is with a pen to see if the red area grows bigger. cellulitis spread? Red lines may appear in the skin spreading out from the centre of the infection. Bad bacteria (germs) gets into broken skin such as a cut or insect bite. What to do Wash your hands before and Cellulitis is a serious infection that needs to after touching the infected area. be treated with antibiotics. Keep your child’s nails short and Go to the doctor if the infected area is clean. painful or bigger than a 10 cent piece. Don’t let your child share Go to the doctor immediately if cellulitis is bath water, towels, sheets and near an eye as this can be very serious. clothes. Make sure your child takes the antibiotics Make sure your child rests every day until they are finished, even if and eats plenty of fruit and the infection seems to have cleared up. The vegetables and drinks plenty of antibiotics need to keep killing the infection water. -

022291S015 Eltrombopag Clinical BPCA
CLINICAL REVIEW Application Type sNDA Application Number(s) 022291, S-015 Priority or Standard Priority Submit Date(s) December 19, 2014 Received Date(s) December 19, 2014 PDUFA Goal Date June 19, 2015 Division / Office Division of Hematology Products/OHOP Reviewer Name(s) Lori A. Ehrlich Review Completion Date May 26, 2015 Established Name Eltrombopag Trade Name Promacta® Therapeutic Class Thrombopoietin Agonist Applicant Glaxo SmithKline Formulation(s) Tablet Dosing Regimen 50 mg once daily Indication(s) Chronic ITP Intended Population(s) Pediatric patients ≥6 years old with chronic ITP Template Version: March 6, 2009 Reference ID: 3765521 Clinical Review Lori A. Ehrlich, MD, PhD NDA 022291, S-015 Promacta® (eltrombopag) tablets Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 8 1.1 Recommendation on Regulatory Action ............................................................. 8 1.2 Risk Benefit Assessment.................................................................................... 9 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies . 11 1.4 Recommendations for Postmarket Requirements and Commitments .............. 11 2 INTRODUCTION AND REGULATORY BACKGROUND ...................................... 11 2.1 Product Information .......................................................................................... 12 2.2 Tables of Currently Available Treatments for Proposed Indications ................. 12 2.3 Availability of Proposed Active Ingredient -

Pseudomonas Skin Infection Clinical Features, Epidemiology, and Management
Am J Clin Dermatol 2011; 12 (3): 157-169 THERAPY IN PRACTICE 1175-0561/11/0003-0157/$49.95/0 ª 2011 Adis Data Information BV. All rights reserved. Pseudomonas Skin Infection Clinical Features, Epidemiology, and Management Douglas C. Wu,1 Wilson W. Chan,2 Andrei I. Metelitsa,1 Loretta Fiorillo1 and Andrew N. Lin1 1 Division of Dermatology, University of Alberta, Edmonton, Alberta, Canada 2 Department of Laboratory Medicine, Medical Microbiology, University of Alberta, Edmonton, Alberta, Canada Contents Abstract........................................................................................................... 158 1. Introduction . 158 1.1 Microbiology . 158 1.2 Pathogenesis . 158 1.3 Epidemiology: The Rise of Pseudomonas aeruginosa ............................................................. 158 2. Cutaneous Manifestations of P. aeruginosa Infection. 159 2.1 Primary P. aeruginosa Infections of the Skin . 159 2.1.1 Green Nail Syndrome. 159 2.1.2 Interdigital Infections . 159 2.1.3 Folliculitis . 159 2.1.4 Infections of the Ear . 160 2.2 P. aeruginosa Bacteremia . 160 2.2.1 Subcutaneous Nodules as a Sign of P. aeruginosa Bacteremia . 161 2.2.2 Ecthyma Gangrenosum . 161 2.2.3 Severe Skin and Soft Tissue Infection (SSTI): Gangrenous Cellulitis and Necrotizing Fasciitis. 161 2.2.4 Burn Wounds . 162 2.2.5 AIDS................................................................................................. 162 2.3 Other Cutaneous Manifestations . 162 3. Antimicrobial Therapy: General Principles . 163 3.1 The Development of Antibacterial Resistance . 163 3.2 Anti-Pseudomonal Agents . 163 3.3 Monotherapy versus Combination Therapy . 164 4. Antimicrobial Therapy: Specific Syndromes . 164 4.1 Primary P. aeruginosa Infections of the Skin . 164 4.1.1 Green Nail Syndrome. 164 4.1.2 Interdigital Infections . 165 4.1.3 Folliculitis .